Translate this page into:
Transparency imaging: A new complementary tool for the assessment of melanocytic nevi
2 Department of Dermatology, Hospital del Bierzo, Ponferrada, León, Spain
3 Dermatology Section, Memorial Sloan Kettering Cancer Center, Hauppauge, New York 11788, USA
Correspondence Address:
Francisco V�zquez-L�pez
Department of Dermatology, Asturias Central Universitary Hospital, Oviedo University. C/Calle Carretera de Rub�n, s/n, 33011 Oviedo, Asturias
Spain
| How to cite this article: Vald�s-Pineda F, Manj�n-Haces J, de Castro CG, Marghoob AA, V�zquez-L�pez F. Transparency imaging: A new complementary tool for the assessment of melanocytic nevi. Indian J Dermatol Venereol Leprol 2015;81:283-285 |
Sir,
Manual measurement of melanocytic nevi is only performed with rulers which are not satisfactory for irregular and large lesions and give no information about shape. Transparency tracing is a standard measurement tool for skin wound areas, which is reliable, sensitive to changes in size and suitable for routine clinical wound assessment, in most clinical settings. [1],[2],[3],[4] Transparency tracing of skin wounds entails tracing the contour on a transparent film with a permanent pen in order to make periodic comparisons for evaluating treatment outcome by means of overlap of transparency tracing with the real wound contour or by morphometry.
In spite of the large experience in wounds, transparency tracing has not yet been applied for the assessment of melanocytic nevi. Transparency tracing could be especially relevant for the assessment of melanocytic nevi in settings with limited access to digital equipment and for measuring intermediate congenital melanocytic nevi. Because the accuracy of baseline images is crucial, our pilot study was focused on this step.
The procedure of transparency tracing of melanocytic nevi is explained in [Figure - 1] and [Figure - 2]. The reproducibility of melanocytic nevi transparency tracing was evaluated by means of scoring the overlap with the real melanocytic nevi contour on 100 common melanocytic nevi lesions from 42 patients (20 males and 22 females). The scoring was performed first over single and later over duplicated transparency tracing by a single observer, as follows:
 |
| Figure 1: (a) The material used for transparency tracing of melanocytic nevi is simple to obtain and of negligible cost: A translucent flexible film (3M) (support for image records) and a fine permanent ink pen for transparencies (Stabilo F, 0.4 mm width) for tracing contours; this material is showed herein for drawing the border of an intermediate melanocytic nevus located on the back of a child. Transparency tracing method is carried out in three steps: (i) Baseline image acquisition; (ii) Storage of records; (iii) Retrieval and comparison of records with the lesion contour or with further images. (b) To trace each image (segmentation), the film is placed against the skin and over the pigmented lesion; the melanocytic nevi contour is then meticulously traced on the film. The position of the film over the lesion is standardized by always using the vertical axis as the reference. (c) The overlap of the previous transparency tracing over the intermediate melanocytic nevi contour is shown in this figure. The dermoscopic appearance of the lesion is shown in the inset. Digital instruments such as the Fotofinder dermoscope include computerized contour detection and measurement of melanocytic nevi but less than 2 cm in diameter. Transparency tracings of melanocytic nevi allow measurement and contour register of larger pigmented lesions. (d) Transparency tracing is shown herein adjacent to the intermediate melanocytic nevi lesion. Envelopes can be used as files for these records |
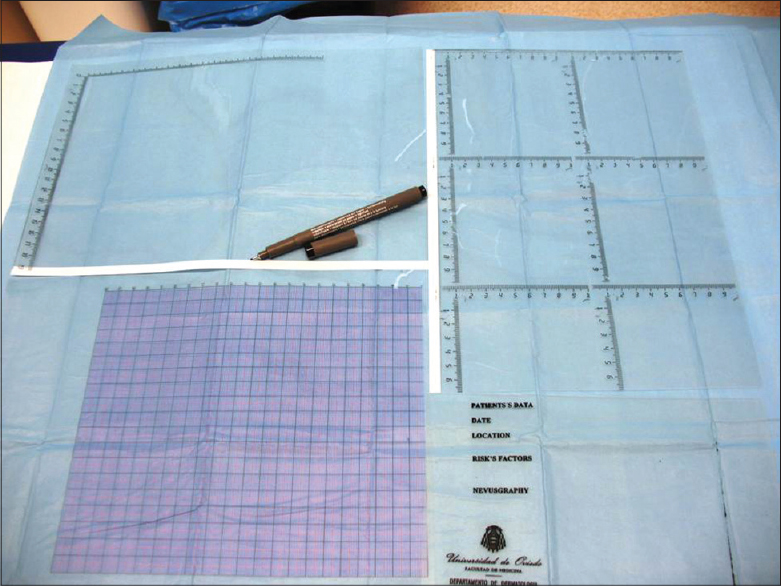 |
| Figure 2: As is shown herein, measurement of melanocytic nevi can be facilitated by printing different scales on the transparencies. Morphometric measurement of the surface area of the transparency tracing can be performed by placing it over square grids, and counting the number of squares (or crossover points) falling on the tracing of the lesion. The film may be provided with an area for tracing lesions and a printed area for recording the patient data and location of the lesion |
- Single transparency tracing. It was scored as accurate (complete overlap with the outline of the melanocytic nevi lesion) or as inaccurate (incomplete overlap with the melanocytic nevi)
- Duplicated transparency tracing (performed twice on the same day). They were scored as accurate (complete overlap both between both transparency tracing and with the real lesion) or as inaccurate (incomplete overlap between them). The reproducibility of the scoring method was evaluated by means of a test-retest, on two separate days (interval of 3-4 weeks, in order to eliminate real changes in melanocytic nevi lesions), and was indirectly tested by means of Cohen′s Kappa statistics.
In the first set, the strength of agreement of the accuracy scoring single transparency tracing (overlap with the real lesion) was good: Kappa value 0.70; 43 (86%) agreements (SE of Kappa, 0.12; 95% confidence interval from 0.32 to 0.80). In the second set (duplicated transparency imaging), the strength of agreement of transparency imaging accuracy scoring (overlap with the real lesion and with the paired transparency imaging) was "very good": Kappa 0.82; 46 (92%) agreements (SE of Kappa 0.08; 95% confidence interval from 0.66 to 0.98).
Our study showed that several factors are important in order to standardize the tracing of transparency tracing: (i) fixing the patient′s position, which influenced the shape of melanocytic nevi in some locations; (ii) fixing the transparency tracing position along the vertical axis of the lesion; and (iii) tracing the melanocytic nevi lesion meticulously. In addition, it was observed that location and morphology also influenced the accuracy of transparency tracing: Melanocytic nevi located in less accessible areas (such as ears, interdigital areas of the foot) and melanocytic nevi disclosing thin irregularities and ill-defined border were the most frequently misrecorded (more than 95% of these lesions were evaluated as inaccurate).
We were unable to find any previous reports concerning the use of transparency tracing for the assessment of melanocytic nevi. [5] There is no gold standard for validating visual tests, but their accuracy could be assessed by repetition or consensus. [6] By means of a Kappa statistical analysis, we found that the reproducibility of the scoring of the accuracy of baseline melanocytic nevi - transparency tracing could be increased by obtaining duplicated transparency tracing, providing more valid support for this technique. Our observations suggested that selection of those melanocytic nevi lesions likely to be more accurately traced with transparency tracing could be performed by taking into account several factors such as location or type of melanocytic nevi border. In addition, the patient position must be fixed. [7]
The range of tools, digitized or not, applied for the assessment of melanocytic nevi includes rulers, photographic methods, and dermoscopy. The availability of techniques besides rulers for manually documenting melanocytic nevi seems appropriate, especially for intermediate lesions. It seems likely that melanocytic nevi, transparency tracing, in combination with other techniques may have a role for this purpose even in a digitized era. In our opinion, transparency tracings are not in opposition but are complementary to other devices for the assessment of melanocytic nevi.
Digital instruments, such as the Fotofinder dermoscope, include computerized, automatic contour detection and measurement of melanocytic nevi but it can be applied only to melanocytic nevi less than 1.5 cm in diameter. Most common small congenital and acquired melanocytic nevi can be digitally measured with this device, but not intermediate congenital melanocytic nevi, which are larger than this upper limit. Transparency tracing seems to be of special value in this setting as a complementary tool, allowing objective measurement and contour comparison of intermediate melanocytic nevi lesions which may be followed clinically with self-examination and with the assistance of a caregiver, if appropriate.
In contrast, methods such as "side by side" photographic comparisons (digital or not), without attempting to reproduce the outline, may be applied for ill-defined melanocytic nevi lesions where transparency tracing is frequently inaccurate.
To conclude, transparency tracing of melanocytic nevi is a simple, low cost, and manual complementary device. Transparency tracing may be useful for patient self-assessment, for clinical monitoring of intermediate congenital melanocytic nevi, as a complement to other digital techniques, and for the assessment of melanocytic nevi in settings with limited access to digital equipment. In order to apply transparency tracing for measurement or surveillance of melanocytic nevi, we would like to propose the term manual nevusgraphy or transparency imaging.
| 1. |
Samad A, Hayes S, French L, Dodds S. Digital imaging versus conventional contact tracing for the objective measurement of venous leg ulcers. J Wound Care 2002;11:137-40.
[Google Scholar]
|
| 2. |
Wunderlich RP, Peters EJ, Armstrong DG, Lavery LA. Reliability of digital videometry and acetate tracing in measuring the surface area of cutaneous wounds. Diabetes Res Clin Pract 2000;49:87-92.
[Google Scholar]
|
| 3. |
Griffin JW, Tolley EA, Tooms RE, Reyes RA, Clift JK. A comparison of photographic and transparency-based methods for measuring wound surface area. Phys Ther 1993;73:117-22.
[Google Scholar]
|
| 4. |
Majeske C. Reliability of wound surface area measurements. Phys Ther 1992;72:138-41.
[Google Scholar]
|
| 5. |
Bahmer FA. Wound measurement made truly simple by point counting. Arch Dermatol 1999;135:991-2.
[Google Scholar]
|
| 6. |
Joel G, Schmid-Saugeon P, Guggisberg D, Cerottini JP, Braun R, Krischer J, et al. Validation of segmentation techniques for digital dermoscopy. Skin Res Technol 2002;8:240-9.
[Google Scholar]
|
| 7. |
Vázquez-López F, Manjón-Haces JA, López-Escobar M, Pérez-Oliva N, Marghoob AA. Sequential image analysis and measurement of pigmented lesions: False variations due to patient positioning. Clin Exp Dermatol 2003;28:657-60.
[Google Scholar]
|
Fulltext Views
2,563
PDF downloads
1,427





