Translate this page into:
Tufted angioma successfully treated with topical timolol gel-forming solution
Corresponding author: Dr. Laxmisha Chandrashekar, Department of Dermatology, Venereology and Leprology, JIPMER, Puducherry - 605 006, India. laxmishac@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Behera B, Remya R, Chandrashekar L, Thappa DM, Gochhait D. Tufted angioma successfully treated with topical timolol gel-forming solution. Indian J Dermatol Venereol Leprol 2021;87:581-4.
Sir,
A four-month-old male child born out of nonconsanguineous marriage was brought by his parents with the complaint of a slowly growing pigmented lesion on the right leg since birth. The lesion was not associated with any history of bleeding or ulceration. Cutaneous examination revealed a solitary, well-defined, reddish-brown, firm plaque of size 6 cm × 3cm circumferentially encircling two-thirds of the right lower leg in a horseshoe manner, sparing the posterior-lateral area [Figure 1]. There was no thrill or bruit. Other mucocutaneous and systemic examinations were within normal limits. Differential diagnoses of infantile hemangioma, tufted angioma, vascular malformation and congenital dermatofibrosarcoma protuberans were considered. A skin biopsy showed tufts of proliferating vessels in the dermis and superficial subcutis in a cannonball distribution surrounded by empty crescent-shaped vessel and fibrous tissue. The vascular tufts were composed of closely packed epithelioid and spindle-shaped endothelial cells and were surrounded by pericytes. On immunohistochemistry, the endothelial cells were highlighted by CD31 and the pericytes by smooth muscle antigen [Figure 2]. A diagnosis of tufted angioma was made. The coagulation profile was within the normal limits. The child was treated with timolol 0.5% gel-forming solution thrice daily. Four months after starting treatment, there was almost complete resolution of the lesion [Figure 3], following which the dose was made twice daily, then once daily, and stopped over the next two months. There was no recurrence of the lesion one year after stopping treatment. During the therapy, the parents did not complain about any adverse reactions. Before the initiation of timolol therapy, the child’s blood pressure, heart rate and glucose level were normal. On day-one, the child’s blood pressure and heart rate were measured at a 6-h interval. The parents were advised to measure the blood pressure and heart rate every week at a nearby hospital. The mother was educated to breastfeed the child frequently and notice for any hypoglycemic symptoms. At each monthly follow-up visit, the child’s blood sugar was within normal limits.

- Solitary well-defined reddish-brown plaque on the right lower leg
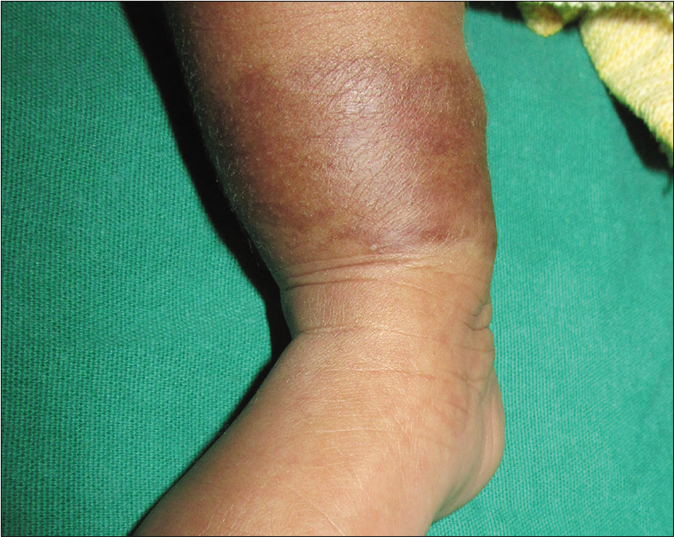
- Closer view of the plaque
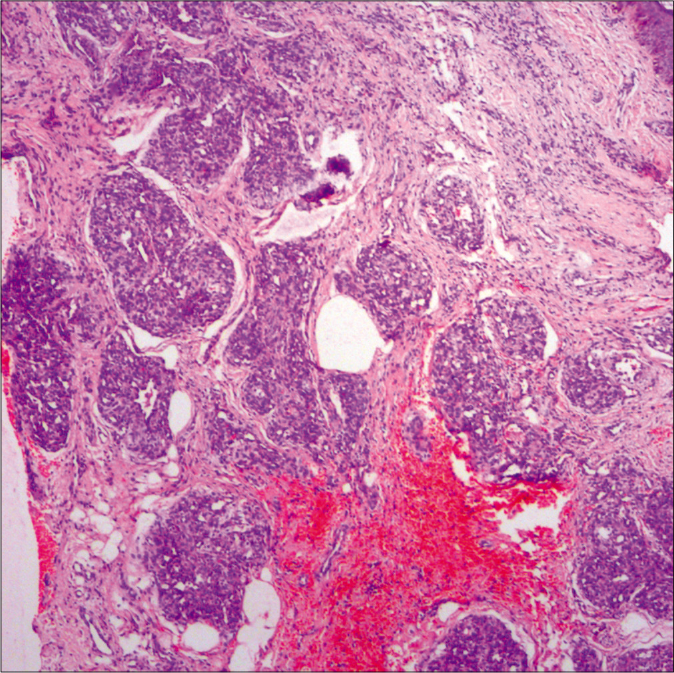
- Tufts of proliferating vessels in a cannonball distribution surrounded by empty crescent-shaped vessels and fibrous tissue (H and E, ×50)
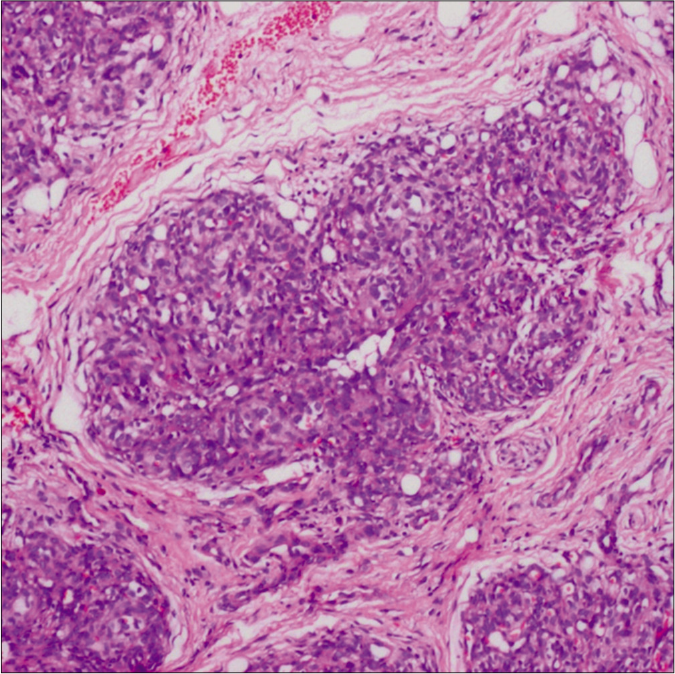
- A tuft of proliferating vessels (H and E, ×100)
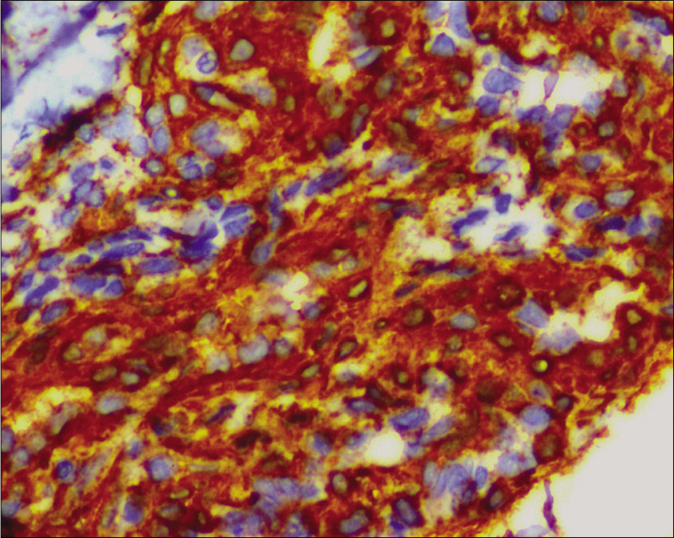
- Immunohistochemistry highlighting CD31 positive endothelial cells (IHC, ×400)
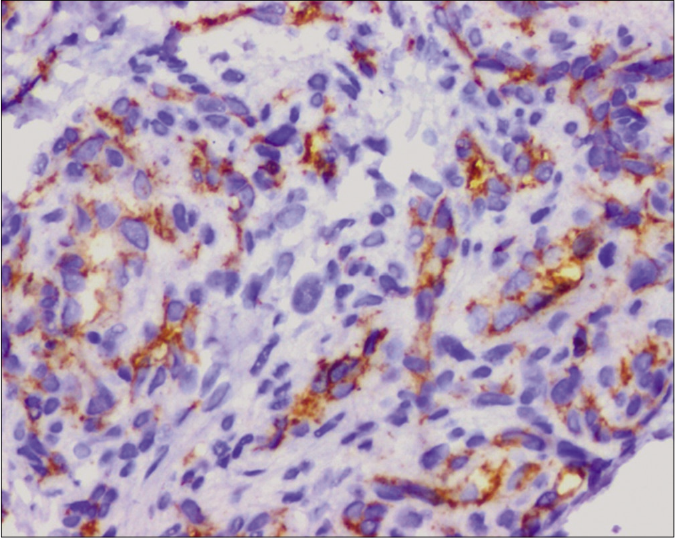
- Immunohistochemistry showing smooth muscle antigen-positive pericytes (IHC, ×400)

- Complete resolution of the tufted angioma

- Complete resolution of the tufted angioma
Tufted angioma is a rare benign vascular tumor that commonly occurs in infancy and childhood. It can be both congenital and acquired and rarely affects adults. It usually presents as a dusky red or violaceous solitary tumor or infiltrating plaque. Associated hyperhidrosis or hypertrichosis can rarely be seen.1 Tufted angioma can have a variable clinical outcome. It can spontaneously regress partially or completely or can enlarge rapidly, leading to life-threatening coagulopathy called the Kasabach-Merritt phenomenon.
On histopathology, the diagnosis is clinched by the presence of proliferating capillaries in cannonball distribution in the dermis and upper subcutis along with lymphatic-like vessels, as in our case.1
Treatment options available for tufted angioma are systemic corticosteroids, vincristine, radiotherapy, interferon, aspirin, ticlopidine, sirolimus, surgical resection and embolization. A meta-analysis by Liu et al. found vincristine to be a better option for the treatment of tufted angioma.2 Sirolimus is increasingly being used in steroid-resistant vascular tumors associated with the Kasabach-Merritt phenomenon.3 The use of topical timolol in vascular proliferation is encouraged by the therapeutic success of oral propranolol in both infantile hemangioma and tufted angioma. A case of tufted angioma without the Kasabach-Merritt phenomenon was successfully managed with oral propranolol.4 We decided to use topical timolol gel-forming solution, instead of oral propranolol, due to the relatively small size of the lesion and no associated complications.
Timolol is a nonselective beta-blocker with activity against both β1 and β2 adrenergic receptors.5 It acts by causing vasoconstriction, blockade of the proangiogenic signaling pathway and apoptosis.5 It has been effectively used in the treatment of both complicated and uncomplicated infantile hemangioma.6 Various formulations like timolol eye drops, gel, gel-forming solution and hydrogel have been used for the treatment of infantile hemangioma with frequencies varying from twice daily to five times daily.7 Timolol gel-forming solution is preferred over other topical solutions because of its less systemic absorption. Systemic side effects like hypotension, bradycardia, hypoglycemia and bronchospasm are rare with topical timolol, but due caution is advised when used in mucosal surfaces or ulcerated lesions, preterm infants, and in occluded areas like diaper region. Dalla Costa et al. have advocated a simplified approach regarding the dose of timolol gel-forming solution to be used, that is, the maximum drops of timolol gel-forming solution to be used per day is equal to the bodyweight of the child in kilograms.8
According to the parents, the plaque was slowly growing until the child presented to us, and the improvement only started after the application of the timolol gel-forming solution. It is difficult to predict the role of spontaneous resolution in the subsidence of the plaque of tufted angioma in the index case. Another advantage of the use of timolol gel-forming solution was the absence of residual skin change following therapy, in contrast to the reports of residual cutaneous changes after spontaneous resolution of tufted angioma.9 A non-regressing painful tufted angioma in a five-year-old girl without any features of the Kasabach-Merritt phenomenon completely resolved by topical timolol maleate 0.5% ophthalmic solution without any recurrence has been reported.10
In conclusion, we are reporting an unusual presentation of tufted angioma as a reddish-brown horseshoe-shaped plaque on the right leg that was successfully treated by a timolol gel-forming solution. Topical timolol gel-forming solution can be a safe and effective therapeutic option for the treatment of uncomplicated tufted angioma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical spectrum of tufted angiomas in childhood: A report of 13 cases and a review of the literature. Arch Dermatol. 2010;146:758-63.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of kaposiform hemangioendothelioma and tufted angioma. Int J Cancer. 2016;139:1658-66.
- [CrossRef] [PubMed] [Google Scholar]
- Successful management of steroid-resistant vascular tumors associated with the Kasabach-Merritt phenomenon using sirolimus. J Dermatol. 2018;45:580-3.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of tufted angioma with propranolol. J Dermatol. 2014;41:1120-2.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of topical timolol on response rate and adverse events in infantile hemangioma: A meta-analysis. Arch Dermatol Res. 2018;310:261-9.
- [CrossRef] [PubMed] [Google Scholar]
- Topical timolol: A safer alternative for complicated and un-complicated infantile hemangiomas. Indian J Dermatol. 2013;58:330.
- [CrossRef] [PubMed] [Google Scholar]
- Topical application of 0.5% timolol maleate hydrogel for the treatment of superficial infantile hemangioma. Front Oncol. 2017;7:137.
- [CrossRef] [PubMed] [Google Scholar]
- Doing the math: A simple approach to topical timolol dosing for infantile hemangiomas. Pediatr Dermatol. 2018;35:276-7.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital, self-regressing tufted angioma. Arch Dermatol. 2006;142:749-51.
- [CrossRef] [PubMed] [Google Scholar]
- Topical timolol maleate for treatment of tufted angioma. J Dermatol. 2019;46:e402-3.
- [CrossRef] [Google Scholar]





