Translate this page into:
Tumor of follicular infundibulum: An unsuspected cause of macular hypopigmentation
2 Apollo Gleneagles Hospitals, Kolkata, India
3 Divyakiran Skin Diseases Treatment, Lasers and Cosmetology Centre, Meerut, Uttar Pradesh, India
Correspondence Address:
Meenakshi Batrani
Delhi Dermatology Group, 10, Aradhana Enclave, R. K. Puram, Sector 13, New Delhi - 110 066
India
| How to cite this article: Kubba A, Batrani M, Taneja A, Jain V. Tumor of follicular infundibulum: An unsuspected cause of macular hypopigmentation. Indian J Dermatol Venereol Leprol 2014;80:141-144 |
Abstract
We present three cases of a rare eruptive variant of tumor of follicular infundibulum. Two patients presented with hypopigmented macules. The clinical differential diagnoses considered in these two cases were vitiligo, lichen sclerosus et atrophicus, and idiopathic guttate hypomelanosis. In the third case, the lesions were hypopigmented flat topped maculo-papules diagnosed clinically as verruca plana. In all three cases, the histopathological features of plate like growth of pale keratinocytes connected to the epidermis and peritumoral condensation of elastic fibers were diagnostic. Although no satisfactory treatment is available, the exclusion of other clinical differential diagnosis particularly vitiligo with its psychosocial implications underscores the importance of skin biopsy.Introduction
Tumor of follicular infundibulum was first described by Mehergen and Butler in 1961. [1] Two clinical variants are known, a common solitary and a rare eruptive form. Tumor of follicular infundibulum has been reported to arise in nevus sebaceous and rarely in association with Cowden′s disease. [2] Histopathologically, tumor of follicular infundibulum-like reactive epidermal changes have been seen as an incidental finding with fibrous histiocytoma, basal cell carcinoma, seborrhoeic keratosis, actinic keratosis, squamous cell carcinoma, melanoma in situ, desmoplastic melanoma, junctional melanocytic nevus, lentigo, hybrid cyst (with features of epidermoid and trichilemmal cyst), epidermal inclusion cyst, epidermoid cyst, trichilemmoma and tinea versiclor. [1],[3],[4]
We report three cases of an uncommon eruptive form of tumor of follicular infundibulum presenting as hypopigmented lesions.
Case Report
Case 1
A 45-year-old male presented with multiple hypopigmented slightly raised flat topped maculo-papular lesions on the left beard area and a few on neck and chest [Figure - 1]a. The lesions gradually increased in number over a period of 18 years. The clinical diagnosis was verruca plana.
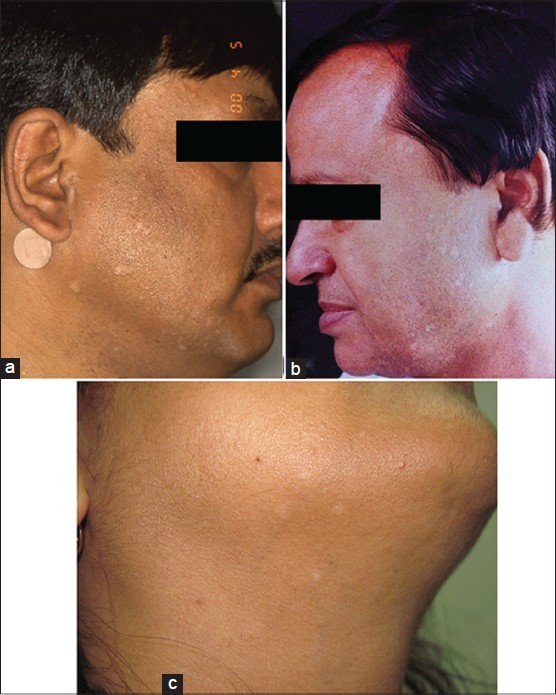 |
| Figure 1: (a) Case 1, flat topped slightly raised hypopigmented maculo-papular lesions on beard area and neck. (b) Case 2, numerous hypopigmented macules on forehead and lateral aspect of cheek. (c) Case 3, four, discrete, small hypopigmented macules, on submandibular region and neck |
Case 2
A 55-year-old male presented with approximately 50-60 hypopigmented lesions on the face particularly on the forehead and mandibular area. The lesions were present for 2 years and had been gradually increasing in number. The lesions were small hypopigmented macules with irregular slightly angulated shapes [Figure - 1]b. The clinical differential diagnoses were vitiligo and lichen sclerosus et atrophicus.
Case 3
A 47-year-old female presented with a one year history of hypopigmented macules and was worried that she had developed vitiligo. The lesions were four discrete, circular, hypopigmented macules, 1-4 mm in size, with ill-defined borders. They were localized to the right side of the neck and submandibular region [Figure - 1]c. The clinical differentials were idiopathic guttate hypomelanosis and vitiligo.
Histopathology
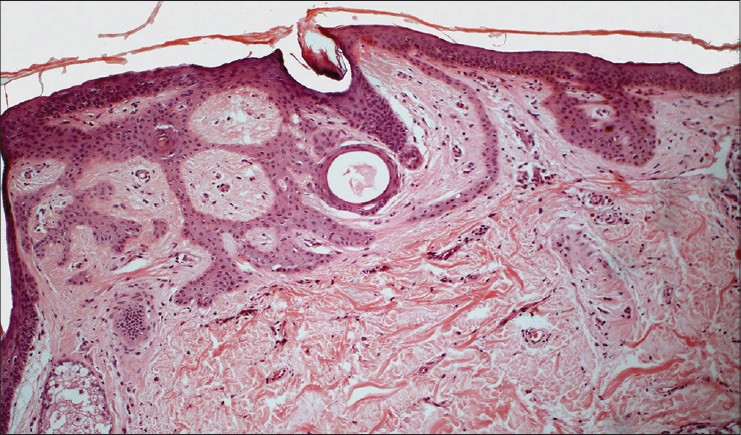
Skin biopsy from all three cases showed similar features. Horizontal plate like proliferation of pale keratinocytes was present with multiple thin connections to the epidermis [Figure - 2]a-c. The Orcein stain demonstrated a rich elastic fiber network surrounding the tumor [Figure - 3]a and b. Masson-Fontana stain demonstrated a loss of melanin pigment from the tumor plates whereas the melanin pigment was preserved in the intervening epidermis [Figure - 4]. In one of the cases (case 2), small horn cysts and tiny squamous eddies were observed [Figure - 5].
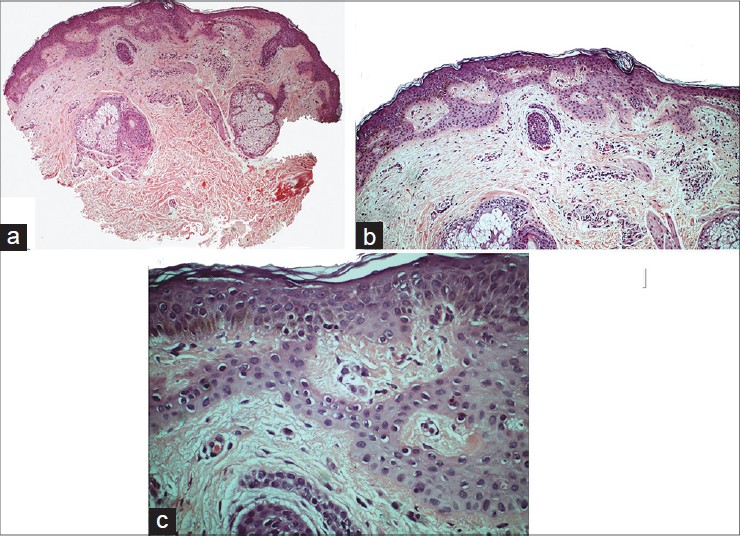 |
| Figure 2: (a) Horizontal proliferation extending from the undersurface of epidermis (H and E, ×40). (b) Plate-like anastmosing cords with multiple thin connections to epidermis (H and E, ×100). (c) Cytologically bland keratnocytes comprising the plates have pale eosinophilic cytoplasm (H and E, ×400) |
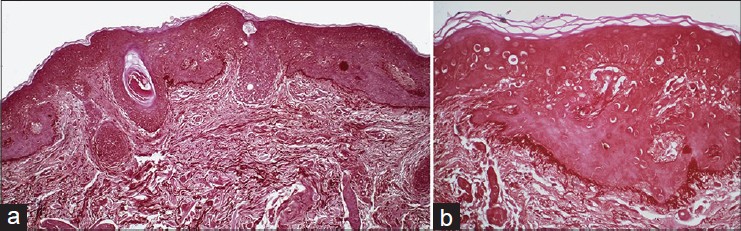 |
| Figure 3: (a) Peritumoral condensation of the elastic fibers with normal intervening epidermis (Orcein, ×100). (b) Brush like condensation of elastic fibers at the lower edge of tumor lobules, and the overlying uninvolved epidermis without the accentuated fiber network (Orcein, ×400) |
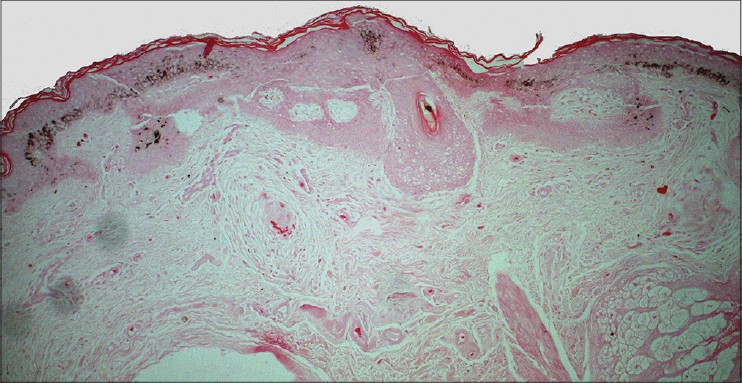 |
| Figure 4: Absence of melanin pigment from the lower edge of the tumor plates with preserved pigment in intervening epidermis (Masson-Fontana, ×100) |
 |
| Figure 5: Small horn cyst and a tiny squamous eddy seen in case 2 (H and E, ×100) |
Follow-up
In case 1, no further follow up after initial diagnosis is available. In case 2, topical retinoids were tried for 3-4 months with no satisfactory response. In case 3, the patient′s concern for vitiligo was relieved and she declined any further treatment.
Discussion
Typically, tumor of follicular infundibulum presents as a solitary lesion in the form of a keratotic papule or nodule usually on the head and neck or trunk of elderly and middle-aged individuals. Buttock and extremities are rarely reported as sites of involvement. [1],[2],[4] Clinically, most cases are diagnosed as either basal cell carcinoma or seborrhoeic keratosis. [2],[3]
The eruptive form is much less frequent in comparison to the solitary variant. In the two largest series available in the literature the eruptive variant constituted 6% [4] and 7.7%, [1] respectively, of all cases. Similar to the solitary variant, eruptive tumor of follicular infundibulum also occurs usually on the head and neck or trunk. [1] Uncommonly, it occurs on the buttocks and extremities. [3],[5] In two isolated case reports, the lesions also involved vulva and intertriginous areas, respectively. [3] Classically, it presents as symmetrically distributed hypopigmented, pale pink to flesh colored and less commonly erythematous, either flat macular, depressed lesions, or papules. The macular and depressed lesions have angulated or irregular borders. [2],[5],[6] The papular lesions are slightly elevated to rounded vegetative lesions with hemorrhagic crusting. [5] Rare morphologies reported are pigmented maculo-papular lesions and scaly reticulated patches. The number of lesions varies from fewer than 20 to more than 100. [3] The lesions tend to be asymptomatic, however, in some cases pruritus after sun exposure has been described. [3],[5] Also, sun exposure better delineates the hypopigmented lesions because of a sharper contrast with adjacent tanned skin. [3],[6] The hypopigmented macular lesions mimic vitiligo, pityriasis alba, pityriasis versicolor, post-inflammatory hypopigmentation, idiopathic guttate hypomelanosis, and tuberculoid leprosy. [1],[3] Differential diagnoses documented in various reports for depressed and papular lesions include acne scars, atrophic lichen planus, focal dermal atrophy, actinic porokeratosis, discoid lupus erythematosus, lichen planus, basal cell carcinoma, nevi, actinic keratosis, inverted follicular keratosis, prurigo nodularis, and trichoepithelioma. [1],[5] Differential diagnosis of lichen sclerosus et atrophicus and viral warts were suspected, respectively, in two of our cases.
Histopathological diagnostic criteria for tumor of follicular infundibulum listed by Ackerman are: (1) a distinctive silhouette with a horizontal proliferation of keratinocytes, (2) characteristic neoplastic epithelial cells with small monomorphic nuclei and abundant pink cytoplasm, and (3) thin columns of cells and also bulkier aggregations, all of which are interconnected. The well developed lesions may show peripheral palisading. [2],[3],[6] Two other distinctive features are glycogen in the cells stained by PAS stain and a network of elastic fibers at the periphery of the tumor highlighted by Orcein staining. [3] Kossard et al. and Alomari et al., in their series of cases, have found that in some tumors, the plate like proliferation is prominent at the edges, whereas in the center it may be lost with tumor replacing the whole epidermis. [1],[6]
A characteristic feature described for eruptive tumor of follicular infundiblum is the decrease of melanin in lesional epithelium in comparison to inter-lesional epidermis which accounts for the clinical hypopigmentation. Apart from this feature, the histopathology of solitary and eruptive variants is similar. [1],[2],[3],[6]
Additional histopathological features, which may be observed, include rudimentary follicular germinative structure formation, multiple connections to outer sheath of adjacent follicles, milia-like cyst, horn cyst, squamous eddies, glandular and ductal structures, sebaceous differentiation, thickened eosinophilic cuticle, and cornoid lamellae like structures. A rare desmoplastic variant has been described. [3]
The histopathological differential diagnoses include basal cell carcinoma, clear cell seborrhoeic keratosis, fibroepithelioma of Pinkus, eccrine syringofibroadenoma and acanthomatous superficial sebaceous hamartoma. Superficial basal cell carcinoma exhibits a plate-like growth similar to tumor of follicular infundibulum. Basal cell carcinoma demonstrates peripheral palisading with stromal retraction, mucin in the stroma, cytological atypia with frequent mitosis and apoptotic cells and lacks the pale cells and peritumoral elastic fibers distinctive of tumor of follicular infundibulum. Clear cell seborrhoeic keratosis has a broader interconnecting rete pattern without peritumoral elastic fiber condensation and shows pseudo-horn cysts. Fibroepithelioma of Pinkus demonstrates complex interconnecting strands of basaloid cells with atypia and mitotic figures and a fibromyxoid stroma. Syringofibroadenoma displays thin anastmosing cords with ductal differentiation and a fibro-vascular stroma. Acanthomatous superficial sebaceous adenoma is characterized by plate-like proliferation of basaloid cells with varying degrees of sebaceous differentiation as opposed to the pale cells of tumor of follicular infundibulum. [3],[4]
The etiology of tumor of follicular infundibum is unclear. One hypothesis describes its origin from follicular infundibulum whereas another group proposes that the tumor is of isthmic origin and believes the name, tumor of follicular infundibulum is a misnomer. [4]
The various treatment options, which have been tried with limited success are topical keratolytics, topical steroids, long-term etretinate, cryotherapy, curettage, and excision. [5] A single case of transformation of two of the tumors of follicular infundibulum to basal cell carcinoma in a patient with over one hundred lesions of eruptive tumor of follicular infundibulum has been documented. [7]
Conclusion
Eruptive tumor of follicular infundibulum is a rare cause of macular hypopigmentation, however, it might be under diagnosed. First, because of the small size and paucity of lesions in some patients, it remains unnoticed. Second, perhaps, due to its low prevalence, it is often clinically not suspected. Therefore skin biopsy is the key to correct diagnosis.
| 1. |
Alomari A, Subtil A, Owen CE, McNiff JM. Solitary and multiple tumors of follicular infundibulum: A review of 168 cases with emphasis on staining patterns and clinical variants. J Cutan Pathol 2013;40:532-7.
[Google Scholar]
|
| 2. |
Cribier B, Grosshans E. Tumor of the follicular infundibulum: A clinicopathologic study. J Am Acad Dermatol 1995;33:979-84.
[Google Scholar]
|
| 3. |
Kolivras A, Moulonguet I, Ruben BS, Sass U, Cappelletti L, André J. Eruptive tumors of the follicular infundibulum presenting as hypopigmented macules on the buttocks of two Black African males. J Cutan Pathol 2012;39:444-8.
[Google Scholar]
|
| 4. |
Abbas O, Mahalingam M. Tumor of the follicular infundibulum: An epidermal reaction pattern? Am J Dermatopathol 2009;31:626-33.
[Google Scholar]
|
| 5. |
Kolenik SA 3 rd , Bolognia JL, Castiglione FM Jr, Longley BJ. Multiple tumors of the follicular infundibulum. Int J Dermatol 1996;35:282-4.
[Google Scholar]
|
| 6. |
Kossard S, Finley AG, Poyzer K, Kocsard E. Eruptive infundibulomas. A distinctive presentation of the tumor of follicular infundibulum. J Am Acad Dermatol 1989;21:361-6.
[Google Scholar]
|
| 7. |
Schnitzler L, Civatte J, Robin F, Demay C. Multiple tumors of the follicular infundibulum with basocellular degeneration. Apropos of a case. Ann Dermatol Venereol 1987;114:551-6.
[Google Scholar]
|
Fulltext Views
5,441
PDF downloads
1,955





