Translate this page into:
Unilateral areolar leiomyoma with sebaceous hyperplasia
Corresponding author: Dr. Yoshiyuki Nakamura, Department of Dermatology, University of Tsukuba, Tsukuba, Ibaraki, Japan, ynakamura-tuk@umin.ac.jp
-
Received: ,
Accepted: ,
How to cite this article: Oya K, Nakamura Y, Fujisawa Y. Unilateral areolar leiomyoma with sebaceous hyperplasia. Indian J Dermatol Venereol Leprol 2022;88:536-40.
Sir,
Leiomyoma frequently develops in the uterus, but its occurrence in the areola is rare. Similarly, sebaceous hyperplasia, usually located on the nose and forehead, also rarely occurs in the areola. However, cases where both leiomyoma and sebaceous hyperplasia developed in the same areolar lesion have not been reported. Here, we report such a case in the unilateral areola.
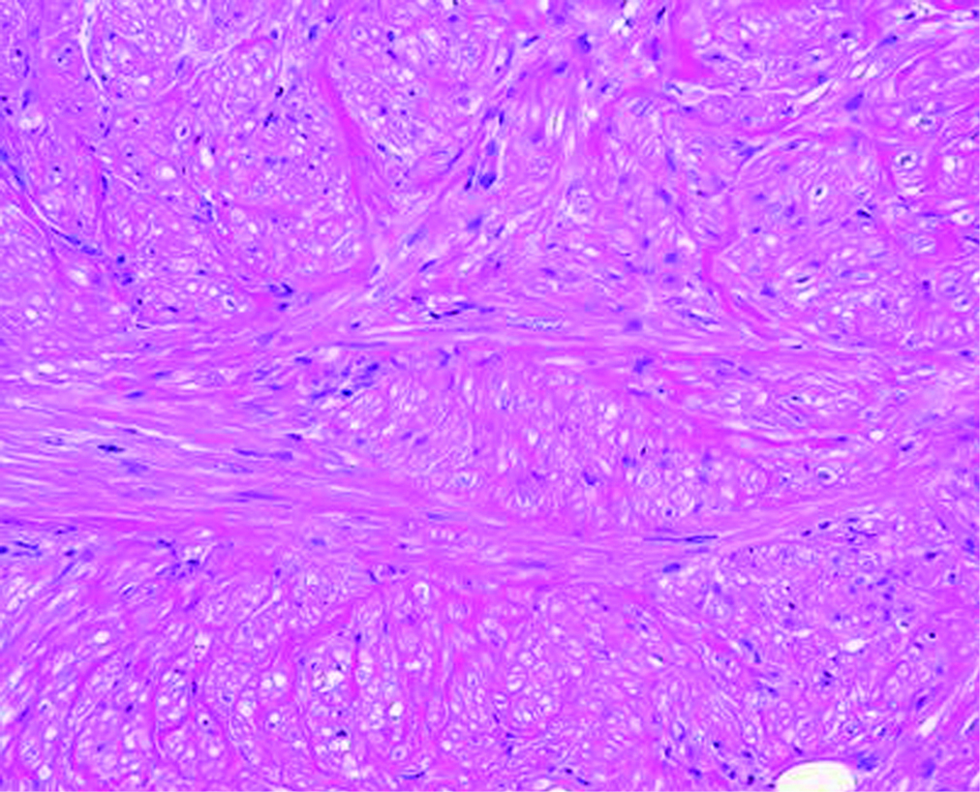
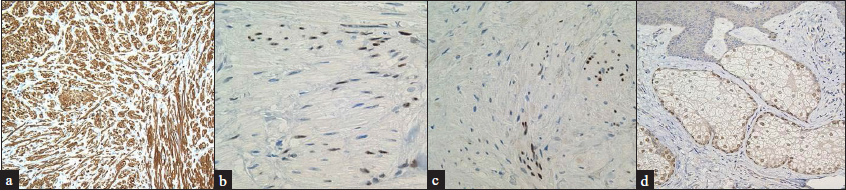
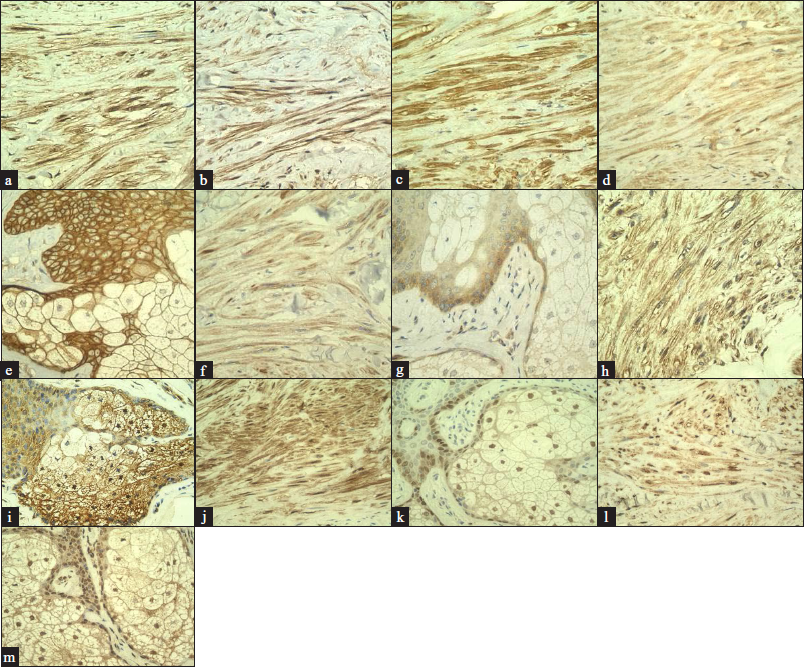
A 41-year-old man noticed a nodule on his left areola one year before his initial visit to our hospital. On physical examination, a 1-cm, yellowish nodule was found on the upper part of the left areola [Figures 1a and b]. Polarized light dermatoscopy (Heine Delta 20 plus; Heine Optotechnik, Herrsching, Germany) revealed white reticular lines with yellowish globular structures [Figure 1c] and a biopsy was performed. Histopathology of the lesion showed numerous, mature sebaceous glands whose ducts directly led to the epidermis [Figures 1d and e]. In addition, moderate epidermal hyperplasia with elongated rete ridges was also observed [Figures 1d and e] and, in the dermis, tumour nests composed of α-smooth muscle actin-positive spindle-shaped cells with intermingled collagen were seen [Figures 1d, f and Figure 2a]. These results led to a diagnosis of areolar leiomyoma with sebaceous hyperplasia. Additional immunohistochemical studies revealed that the leiomyoma was positive for estrogen and progesterone receptors but the proliferated sebocytes were negative [Figures 2b and c]. In contrast, the sebocytes were positive for androgen receptors but the leiomyoma was negative [Figure 2d]. Epidermal growth factor, insulin-like growth factor-1 and fibroblast growth factor-2 were highly expressed in the leiomyoma [Figures 3a-c and 4a-d]. Epidermal growth factor receptor, insulin-like growth factor-1 receptor β and fibroblast growth factor receptor 2, a receptor for fibroblast growth factor-2, were expressed in the leiomyoma, the sebocytes and the adjacent keratinocytes [Figures 3d-i and 4e-h]. In addition, phosphorylated extracellular signal-regulated kinase 1/2 and phosphorylated Akt were positive in the leiomyoma, the sebocytes and the adjacent keratinocytes [Figures 3j-m and 4a, e, i and j]. Although the patient refused resection of the whole lesion, it has remained stable for more than one year.
Smooth muscle hamartoma should be considered for the differential diagnosis of dermal lesions such as the lesion of the present case. This disease generally presents as variably sized papules, patches, and plaques. Histologically, this disease comprises variably oriented, discrete, and well-defined bundles of smooth muscle cells. These clinicopathologic findings differ from those of the present case, which presented clinically as a nodule and with histologic findings of smooth muscle cell proliferation with intermingled collagen, findings consistent with leiomyoma. Cutaneous leiomyomas are categorized into pilar, angio- and genital leiomyomas and areolar leiomyoma is a rare variant of genital leiomyoma. They may show overlying epidermal hyperplasia as frequently seen in pilar leiomyoma although the mechanism of this remains elusive.
Some growth factors such as epidermal growth factor, insulin-like growth factor and fibroblast growth factor may play crucial roles for sebocyte proliferation.1 In addition, some dermal tumours, such as dermatofibroma, are thought to induce epithelial hyperplasia through growth factor secretion.2 Uterine leiomyoma has also been reported to produce some growth factors, which may promote the growth of the tumour cells in an autocrine manner.3 Moreover, endometrial hyperplasia adjacent to uterine leiomyoma is often seen.4 This may be due to the hyperestrogenic status. However, given that growth factors play important roles in endometrial proliferation, growth factors produced from uterine leiomyoma might also contribute to endometrial hyperplasia via paracrine action.5 In the present case, tumour cells of the leiomyoma showed high expression levels of epidermal growth factor, insulin-like growth factor-1 and fibroblast growth factor-2. These receptors were also expressed in the leiomyoma. In addition, phosphorylated extracellular signal-regulated kinase 1/2 and phosphorylated Akt, representative markers of the activated downstream signalling pathways of the growth factor receptors, were positive in the leiomyoma, suggesting that growth factors from the leiomyoma might have promoted the growth of the leiomyoma itself in an autocrine manner identical to uterine leiomyoma. Moreover, in the present case, the sebocytes and the adjacent keratinocytes expressed epidermal growth factor receptor, insulin-like growth factor-1 receptor β and fibroblast growth factor receptor 2 while also being positive for phosphorylated extracellular signal-regulated kinase 1/2 and phosphorylated Akt, suggesting that the sebaceous hyperplasia with moderate acanthosis might have developed due to the growth factors produced by the underlying leiomyoma.
In conclusion, we describe a case where both leiomyoma and sebaceous hyperplasia were observed in the unilateral areola. Although the exact pathogenesis of the rare association in the present case remains unknown, we speculate that the leiomyoma-produced growth factors including epidermal growth factor, insulin-like growth factor-1 and fibroblast growth factor-2 may have been involved in the growth of the leiomyoma itself in an autocrine manner and of the overlying sebocytes and keratinocytes by paracrine action.

- A 1 cm nodule (black arrow) was observed on the left areola

- The white arrowhead and black arrow indicate the left nipple and nodule, respectively

- White reticular lines with yellowish globules (polarized, ×10)
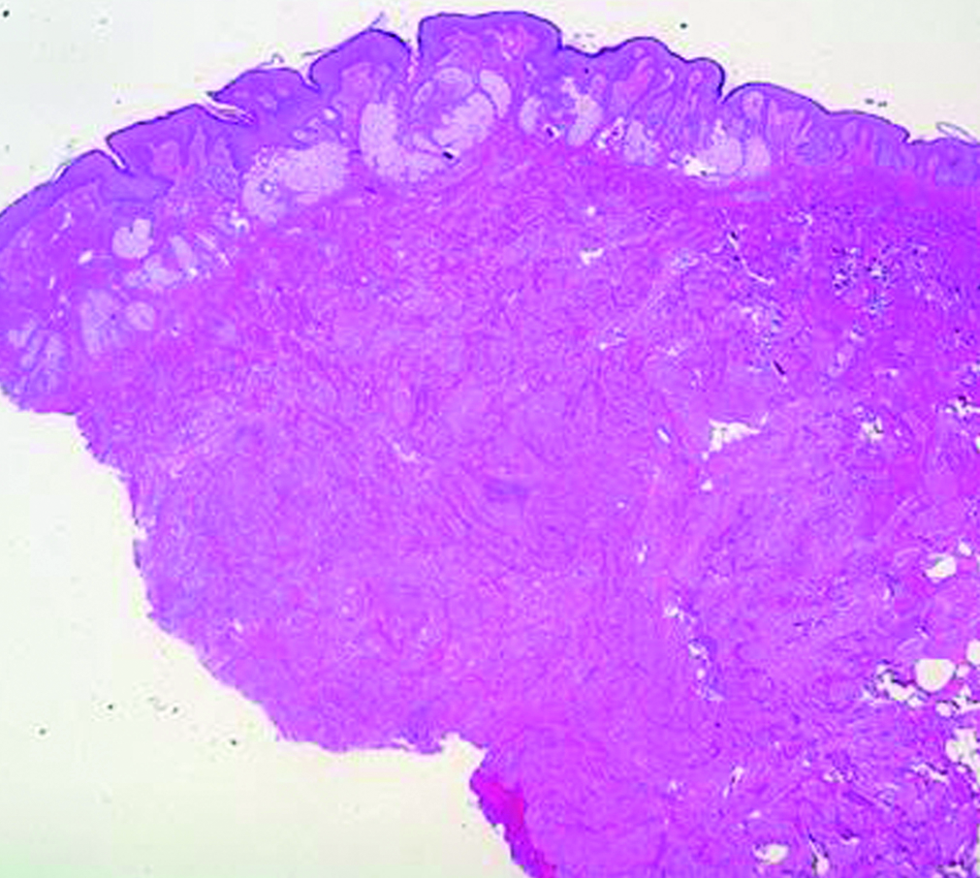
- Large numbers of mature sebaceous glands and dermal tumour nests visible in the dermis. (Hematoxylin and eosin, ×20)

- The proliferated sebaceous glands leading directly to the epidermis. Moderate acanthosis with elongated rete ridges are also visible (Haematoxylin and eosin, ×100)
- The dermal tumour cells with a spindle-shaped morphology (Haematoxylin and eosin, ×200)
- The dermal tumour cells showing positive staining for (a) α-smooth muscle actin (×200), (b) estrogen receptors (×400) and (c) progesterone receptors (×400); (d) Proliferated sebocytes testing positive for androgen receptors (×200)
- High expression in the leiomyoma displayed by (a) epidermal growth factor (×400), (b) insulin-like growth factor-1 (×400) and (c) fibroblast growth factor-2 (×400); (d) Epidermal growth factor receptor showing expression in the leiomyoma (×400), (e) Epidermal growth factor receptor showing expression in the sebocytes with the adjacent keratinocytes (×400), (f) Insulin-like growth factor-1 receptor β showing expression in the leiomyoma (×400), (g) Insulin-like growth factor-1 receptor β showing expression in the sebocytes with the adjacent keratinocytes (×400), (h) Fibroblast growth factor receptor 2 showing expression in the leiomyoma (×400), (i) Fibroblast growth factor receptor 2 showing expression in the sebocytes with the adjacent keratinocytes (×400), (j) Positive staining of phosphorylated extracellular signal-regulated kinase 1/2 in the leiomyoma (×400), (k) Positive staining of phosphorylated extracellular signal-regulated kinase 1/2 in the sebocytes with adjacent keratinocytes (×400), (l) Positive staining of phosphorylated Akt in the leiomyoma (×400), (m) Positive staining of phosphorylated Akt in the sebocytes with adjacent keratinocytes (×400).
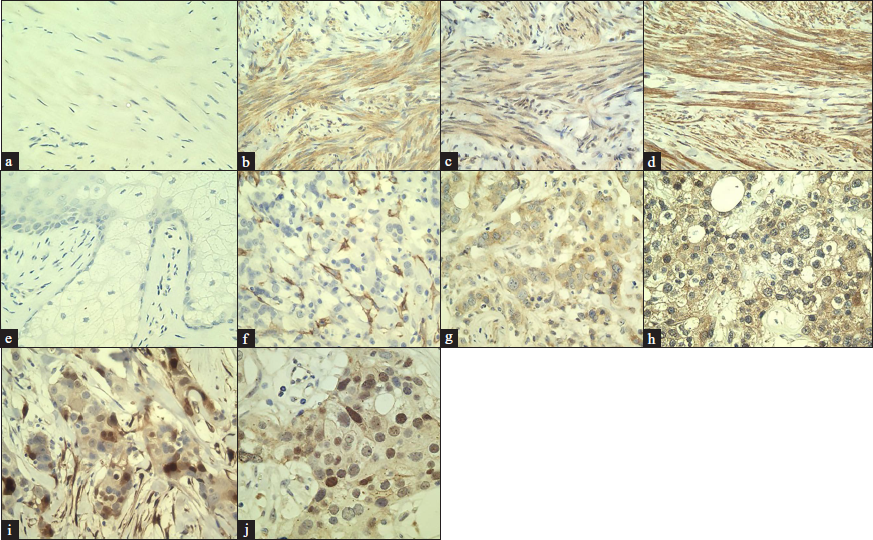
- (a) Negative control staining in the leiomyoma using rabbit IgG isotype control antibody (×400); Positive control staining using a uterine leiomyoma sample for: (b) epidermal growth factor (×400), (c) insulin-like growth factor-1 (×400), (d) fibroblast growth factor-2 (×400), (e) Negative control staining in the sebocytes with adjacent keratinocytes using rabbit IgG isotype control antibody (×400); Positive control staining using a breast cancer sample for: (f) epidermal growth factor receptor (×400), (g) insulin-like growth factor-1 receptor β (×400), (h) fibroblast growth factor receptor 2 (×400), (i) phosphorylated extracellular signal-regulated kinase 1/2 (×400) and (j) phosphorylated Akt (×400)
Declaration of patient consent
Patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Homeostasis of the sebaceous gland and mechanisms of acne pathogenesis. Br J Dermatol. 2019;181:677-90.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelial induction in dermatofibroma: A role for the epidermal growth factor (EGF) receptor. Am J Dermatopathol. 1997;19:35-40.
- [CrossRef] [PubMed] [Google Scholar]
- Interactions of cytokines, growth factors, and the extracellular matrix in the cellular biology of uterine leiomyomata. Fertil Steril. 2002;78:1-12.
- [CrossRef] [PubMed] [Google Scholar]
- Developmental reprogramming of IGF signaling and susceptibility to endometrial hyperplasia in the rat. Lab Invest. 2008;88:615-26.
- [CrossRef] [PubMed] [Google Scholar]





