Translate this page into:
Unilateral chilblains affecting the lower limb with post-polio residual paralysis: An example of immunocompromised cutaneous district
Corresponding author: Dr. Vishal Gupta, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. doctor.vishalgupta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhatia R, Arava S, Gupta V. Unilateral chilblains affecting the lower limb with post-polio residual paralysis: An example of immunocompromised cutaneous district. Indian J Dermatol Venereol Leprol 2021;87:558-9.
Sir,
Chilblains or perniosis is an idiopathic cold-sensitive inflammatory disorder characterized by bilateral symmetrical involvement of acral sites. Here, we report a case of unilateral chilblains involving only the lower limb affected by post-polio residual paralysis, as an example of immunocompromised cutaneous district.
A 28-year-old male presented to us with swelling and itching of the toes on the right foot, along with bluish-red discoloration for the past ten days. He used to notice similar lesions during every winter season for the past four years which would subside spontaneously during summers. There was no history of similar symptoms affecting the left foot. His medical history was significant for post-polio residual paralysis affecting the right lower limb since childhood. He was also diagnosed with myasthenia gravis and was being treated with oral prednisolone and pyridostigmine since one year. His family history was not contributory. On examination, right foot toes were edematous and showed erythrocyanotic discoloration with overlying retiform purpuric macules. The toes were mildly tender and cold on palpation. The left foot appeared unaffected [Figure 1]. Routine laboratory investigations including a complete blood count and serum biochemistry were within normal limits. An arterial and venous Doppler study was unremarkable. A punch biopsy from one of the purpuric macules showed a subepidermal split with full-thickness necrosis of the overlying epidermis [Figure 2a]. There was a mild perivascular and peri-eccrine lymphocytic infiltrate in superficial and deep dermis with fibrin thrombi within the lumen of blood vessels at all levels of the dermis [Figure 2b]. Serological investigations for antinuclear antibodies, antiphospholipid antibodies and cryoglobulins were negative. With a diagnosis of chilblains, the patient was prescribed mometasone furoate 0.1% cream once a day, antihistamines and cold protection with good improvement in the next few days.

- Toes of the right foot are swollen and show erythrocyanotic discoloration with overlying retiform purpura. Note the orthosis supporting right foot and leg. Toes of the left foot are unaffected
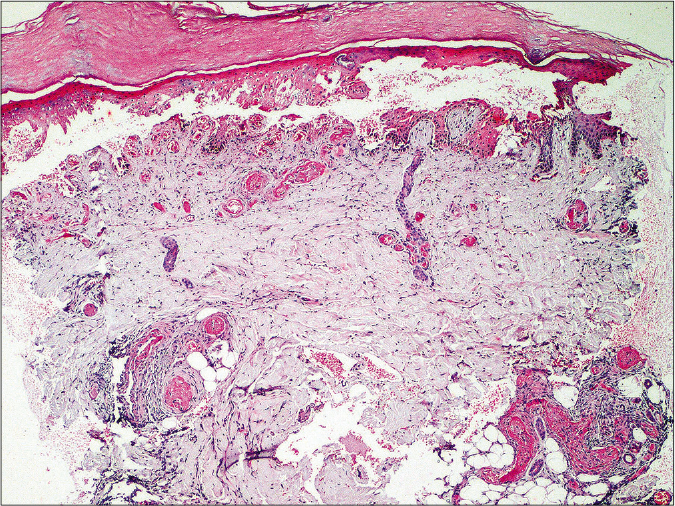
- Histopathology shows a subepidermal split with necrosis of overlying epidermis. Dermis shows mild perivascular and peri-eccrine lymphocytic infiltrate, and fibrin thrombi in the lumen of blood vessels in superficial and deep dermis (H and E, 40×)
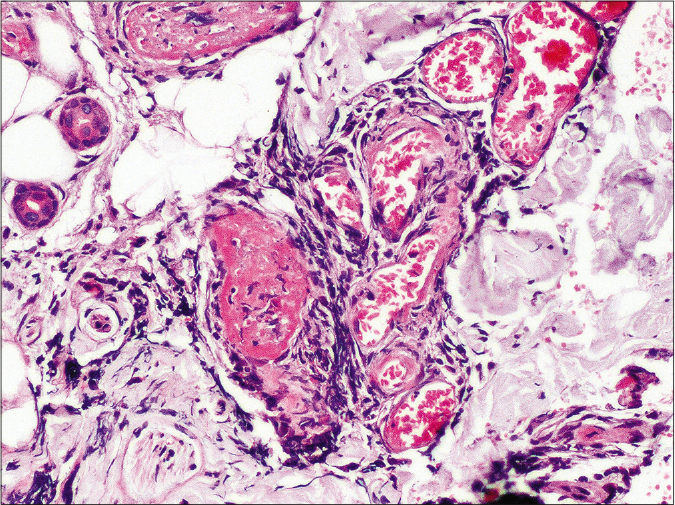
- Higher magnification showing fibrin thrombi occluding the blood vessel wall lumen in deep dermis and a perivascular cuffing by lymphocytes (H and E, 400×)
There are several examples of preferential localization of cutaneous disorders on previously damaged skin in dermatology literature. Wolf’s isotopic response is a well-recognized example of such a phenomenon. Herpes zoster scars, chronic lymphedema, vaccination sites and areas affected by other injuries such as burns, radiation, tattoos, or trauma are known to be susceptible sites for a variety of inflammatory dermatoses, infections and tumors. This has been explained by the concept of “immunocompromised cutaneous district” put forth by Ruocco et al. which refers to a regional alteration in the immune response making an area more vulnerable (locus minoris resistentiae) than the rest of the body for development of cutaneous disorders.1
Our case of unilateral chilblains affecting the post-polio paralytic limb is also an example of immunocompromised cutaneous district. Other examples of post-polio limb as an immunocompromised district in the literature include development of papillomatosis cutis (a benign verrucous epidermal hyperplasia)2 and being spared from psoriasis.3 Although not completely understood how a paralytic limb may become more vulnerable to inflammatory dermatoses, it is postulated that paralysis may result in a sectoral immune alteration from abnormal trafficking of inflammatory cells due to impaired lymphatic drainage.1 Increased vasoreactivity has also been reported in the post-polio limbs, though accompanied by a diminished T-cell response.4 Poliomyelitis primarily affects motor neurons, but there is some evidence to suggest that sensory and sympathetic nerves may also be damaged.4,5 The dysregulated release of immune related peptides from damaged nerve endings in the paretic limb may further contribute to the altered immune milieu.1
Diagnosis of chilblains in our patient was made based on the typical history and clinical morphology, a supportive histopathology and the absence of an underlying connective tissue disease or vasculopathy. We came across only four reports of unilateral chilblains in the literature, all of which involved a previously damaged extremity -a foot affected with polio post-operatively, paralysed leg following lumbar compression, following radiation and surgery, and a hand injured after severe dog bite.6-8 We report this case of unilateral chilblains as dermatologists may be perplexed by such an atypical presentation. Involvement of the paralytic or injured limb can explain the unilaterality of chilblains.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The immunocompromised district: A unifying concept for lymphoedematous, herpes-infected and otherwise damaged sites. J Eur Acad Dermatol Venereol. 2009;23:1364-73.
- [CrossRef] [PubMed] [Google Scholar]
- Papillomatosis cutis arising on an immuno-compromised district due to paraplegia. Br J Dermatol. 2010;163:646-8.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis sparing the lower limb with postpoliomyelitis residual paralysis. Br J Dermatol. 2014;171:429-31.
- [CrossRef] [PubMed] [Google Scholar]
- Lateralization of cutaneous inflammatory responses in patients with unilateral paresis after poliomyelitis. J Neuroimmunol. 1996;67:1-6.
- [CrossRef] [Google Scholar]
- Sensory physiology assessed by evoked potentials in survivors of poliomyelitis. Muscle Nerve. 2008;38:1266-71.
- [CrossRef] [PubMed] [Google Scholar]
- Localized recurrent postoperative pernio associated with leukocytoclastic vasculitis. J Am Acad Dermatol. 1991;24:811-3.
- [CrossRef] [Google Scholar]
- Posttraumatic unilateral perniosis: A case report. JAAD Case Rep. 2019;5:909-11.
- [CrossRef] [PubMed] [Google Scholar]
- Two cases of unilateral chilblains associated with monoparesis. Ann Dermatol Venereol. 2019;146:557-62.
- [CrossRef] [PubMed] [Google Scholar]





