Translate this page into:
Unilateral erythematous nodule over eyelid
Corresponding author: Dr Anupama Bains, Department of Dermatology, AIIMS Jodhpur, Rajasthan, India. whiteangel2387@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ansari F, Agrawal A, Bains A, Elhence P. Unilateral erythematous nodule over eyelid. Indian J Dermatol Venereol Leprol 2023;89:928
A 60-year-old woman from West Rajasthan presented with the complaint of an insidious onset of gradually progressive reddish swelling on the left upper eyelid for 1.5 months, which was associated with heaviness and mild pain. She denied history of insect bite, ocular symptoms, fever or any other systemic complaints. On examination, a single, well-defined, soft, non-tender, erythematous nodulo-plaque of 2 × 2 cm size was present on the left upper eyelid with overlying whitish scales and no discharge [Figure 1]. Rest of the cutaneous and systemic examination was normal. Ophthalmological evaluation was unremarkable. Ultrasonography showed a hypoechoic lesion in the subcutaneous plane. Slit skin smear for Mycobacterium leprae was negative. Punch biopsy revealed mild focal spongiosis and follicular plugging in epidermis. Grenz zone was noted. Entire dermis and subcutis showed diffuse infiltrate of epithelioid histiocytes admixed with plasma cells and lymphocytes. Histiocytes were studded with small intra-cytoplasmic, basophilic inclusion bodies which were highlighted by Giemsa stain [Figures 2a and 2b].

- Solitary mildly erythematous scaly nodulo-plaque on the left upper eyelid.
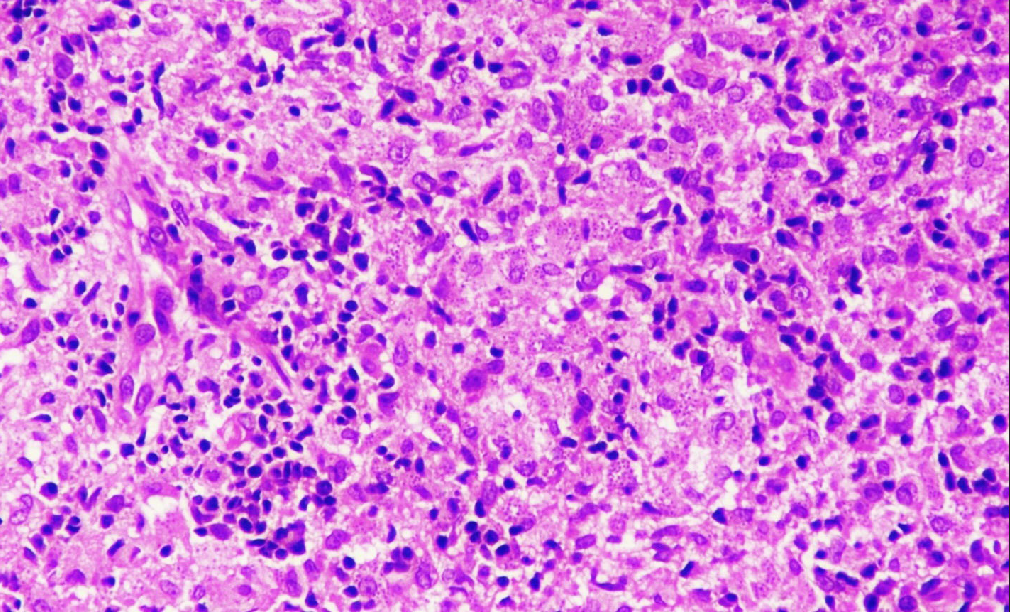
- Entire dermis and subcutis show diffuse infiltrate of epithelioid histiocytes admixed with plasma cells and lymphocytes. Histiocytes are studded with small intra-cytoplasmic, basophilic inclusion bodies (H&E 100×)
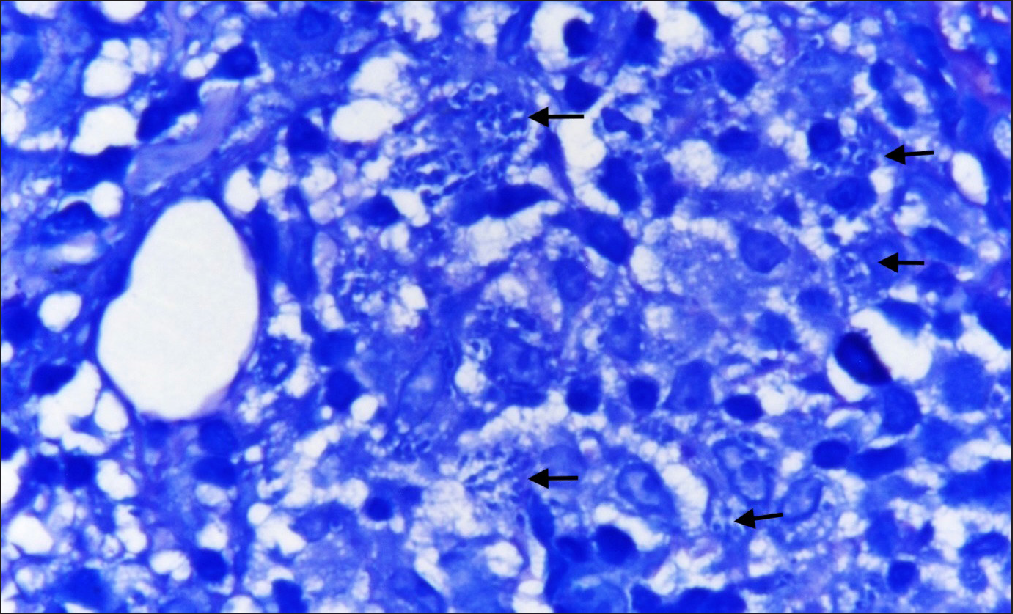
- Arrows point towards intra-cellular inclusion bodies (Giemsa stain 400×)
Question
What is your Diagnosis?
Diagnosis
Localized Cutaneous Leishmaniasis
Discussion
Leishmaniasis is caused by protozoans of genus Leishmania and transmitted by sandflies. Leishmaniasis has mainly four clinical forms; cutaneous (diffuse or localized), mucosal, visceral and post-kala-azar dermal leishmaniasis. Other rare forms include leishmania recidivans and lupoid leishmaniasis. Cutaneous leishmaniasis is characterized by the development of single or multiple localized lesions on the exposed areas of skin after an incubation period of 3–8 weeks.1
Different species of Leishmania lead to different clinical features. Clinical forms of localized cutaneous leishmaniasis are papular, nodular, ulcerative plaque, infiltrative and impetigo-like.1 Face along with upper and lower extremities are the most commonly involved sites but ocular involvement is very rare. The eyelids, conjunctiva and inner parts of the eyes may be affected in patients having ocular involvement. Of these, eyelid leishmaniasis is very uncommon and is seen in only 2–5% of cases.2 There are only two published case reports of eyelid leishmaniasis from India.2,3
Regular movements of eyelids prevent sandfly bite in this area, leading to rarity of this disease on the eyelid. The differential diagnoses considered in this case were chalazion, lupus vulgaris, sarcoidosis, pseudo-lymphoma and basal cell carcinoma. Table 1 enumerates the clinical and histopathological differences among these entities.4–7 Lateral eyelid involvement is usually self-limiting and heals by scarring but medial eyelid involvement leads to contiguous spread to the conjunctiva, sclera and cornea with development of interstitial keratitis.3 Eyelid cutaneous leishmaniasis can lead to complications like palpebral scar, trichiasis, conjunctival scar, scleral perforation, corneal opacity, secondary glaucoma, epidermoid carcinoma and squamous cell carcinoma.1
| Disease | Clinical features | Histopathological features |
|---|---|---|
| Chalazion4 | Solitary, palpable, usually non-tender, non-fluctuant, non-erythematous nodule on the upper eyelid. | Chronic granulomatous reaction with numerous lipid-filled, touton-type giant cells. |
| Lupus vulgaris5 | Solitary well-defined plaque with central scarring and infiltration and scaling at margins. | Tubercular granulomas with scanty or absent central caseation surrounded by epithelioid histiocytes and multinucleated giant cells that are present in the superficial dermis with prominent peripheral lymphocytes. |
| Sarcoidosis6 | Solitary or multiple round or oval infiltrated plaques, brownish red in colour with little epidermal change. | Dense, non-caseating naked granulomas composed of epithelioid histiocytes in the dermis which may extend into subcutaneous fat. |
| Pseudolymphoma7 | Solitary or multiple smooth erythematous to bluish nodules typically located on the head, face or neck. | Predominantly intradermal dense lymphocytic infiltrates (nodular or diffuse) consisting of small to medium-sized lymphocytes without significant nuclear atypia which may extend to the subcutis. |
| Basal cell carcinoma8 | Usually present as a small papule which later forms a nodule which may be associated with ulcer and pigmentation. | Classic palisading tumour. The various histological types of BCC include nodular (40–50%), infiltrative (15–25%), ulcerative, morphea-like, sclerosing, mixed, basosquamous and pigmented. |
It is best to perform bed-side diagnostic test by taking a smear of the material from the lesion and staining it with Wright or Giemsa stain which may reveal the presence of Leishman-Donovan (LD) bodies. Histopathological examination of the lesion may also reveal LD bodies in early cases. Culture of the material in Novy-MacNeal-Nicolle medium may also be done for the confirmation of the diagnosis.3
Other modalities which can be used for diagnosis include leishmania intradermal skin test (Montenegro test), detection of anti-leishmania antibodies through agglutination or fluorescent antibody tests and polymerase chain reaction (PCR)-based methods including real-time PCR, DNA sequencing and through species-specific primers (DNA probes).9
Treatment modalities for cutaneous leishmaniasis include systemic or intralesional pentavalent antimony compounds, cryotherapy, topical paromomycin, local heat, excision, curettage, electrodessication, carbon dioxide laser, oral itraconazole, ketoconazole, miltefosine, etc.10 In the present case, she was started on oral itraconazole 200 mg twice daily. The lesion size reduced significantly after 2 months of treatment [Figure 3]. Itraconazole was continued further at the same dose for another 4 months which led to complete resolution of the lesion.

- Decrease in erythema and size of the lesion after 2 months of treatment.
This case report highlights an unusual presentation of cutaneous leishmaniasis which clinicians need to be aware of.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There is no conflict of interest.
References
- Cutaneous leishmaniasis of the eyelids: a case series with molecular identification and literature review. Korean J Parasitol. 2016;54:787-92.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lid leishmaniasis: an atypical presentation of cutaneous leishmaniasis. Int J Health Sci Res. 2017;7:391-4.
- [Google Scholar]
- Cutaneous leishmaniasis of the eyelid: an uncommon presentation of a common entity. Indian J Paediatr Dermatol. 2017;18:116-8.
- [Google Scholar]
- Accuracy of the clinical diagnosis of chalazion. Eye (Lond). 2004;18:135-138.
- [CrossRef] [PubMed] [Google Scholar]
- Lupus vulgaris: an atypical presentation. Indian J Dermatol Venereol Leprol. 2010;76:180-181.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous sarcoidosis: clinical profile of 23 Indian patients. Indian J Dermatol Venereol Leprol. 2007;73:16-21.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous pseudolymphoma-a review on the spectrum and a proposal for a new classification. J Cutan Pathol.. 2020;47:76-97.
- [CrossRef] [PubMed] [Google Scholar]
- Laboratory diagnosis of cutaneous and visceral leishmaniasis: current and future methods. Microorganisms. 2020;8:1632.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous leishmaniasis: successful treatment with itraconazole. Int J Dermatol. 2006;45:46-9.
- [CrossRef] [PubMed] [Google Scholar]





