Translate this page into:
Use of intralesional bleomycin as primary therapy in macrocystic lymphangiomas
2 Department of Radiology, Chacha Nehru Bal Chikitsalaya, Geeta Colony, Delhi, India
Correspondence Address:
Vishesh Jain
D-9, 2nd Floor, Green Park Extension, New Delhi-110 016
India
| How to cite this article: Jain V, Mohta A, Sengar M, Bansal K, Valvi K. Use of intralesional bleomycin as primary therapy in macrocystic lymphangiomas. Indian J Dermatol Venereol Leprol 2013;79:524-525 |
Sir,
We share our experience with intralesional bleomycin injection for management of lymphangiomas.
A prospective study was conducted to determine the efficacy and short term adverse effects of intralesional bleomycin sclerotherapy in children with lymphangioma. The diagnosis of lymphangioma was made on clinical examination and was supplemented with Doppler ultrasonography. Children with ultrasonographically proven, subcutaneous, macrocystic lymphangiomas with no/ minimal vascularity were included in the study. Before the procedure hemogram and baseline chest radiograph were performed. The procedure was performed after taking consent for the parents, under mild sedation (oral Triclofos) and aseptic conditions. A 20 G needle was used to perform the aspiration and attempt was always made to traverse the needle in subcutaneous plane initially and then puncture the lymphangioma in order to prevent egress of bleomycin from the puncture site at the end of the procedure. After complete aspiration of the lesion bleomycin was injected through the same needle. If the cyst could not be aspirated properly then injection under ultrasonographic guidance was performed. Bleomycin (1 mg/ml) was administered at dose of 0.6 mg/kg with a maximum dosage of 1 mg/kg or 15 mg per session. A compression dressing, if feasible, was applied after the procedure. The parents were instructed to review with the child after 2 days in the outpatient department for removal of dressing and evaluation of any adverse effects. Patient was again examined at the end of 3 weeks and need for repeat injection assessed.
Thirteen patients were included in the study. There were 8 boys and 5 girls with ages ranging from 15 days to 10 years (median 1 year). Most of the lesions were present in the cervical (n = 8) and axillary (n = 2) regions. The remaining 3 lesions were also seen at relatively uncommon sites like scapular region, shoulder and floor of the mouth. A single injection of bleomycin was effective in 8 patients [Figure - 1] and [Figure - 2] and the maximum numbers of injections needed were 3 (mean 1.5 injections per patient). Lymphangiomas of the floor of the mouth and scapular region needed 3 injections; rest all lesions required only 1-2 injections for desired response. The mean total cumulative dose of bleomycin injected was 1 mg/kg. Only two sclerotherapy sessions were performed under ultrasonographic guidance. Apart from transient local rash with fever reported after 2 injections (10%), no other adverse effects were noted.
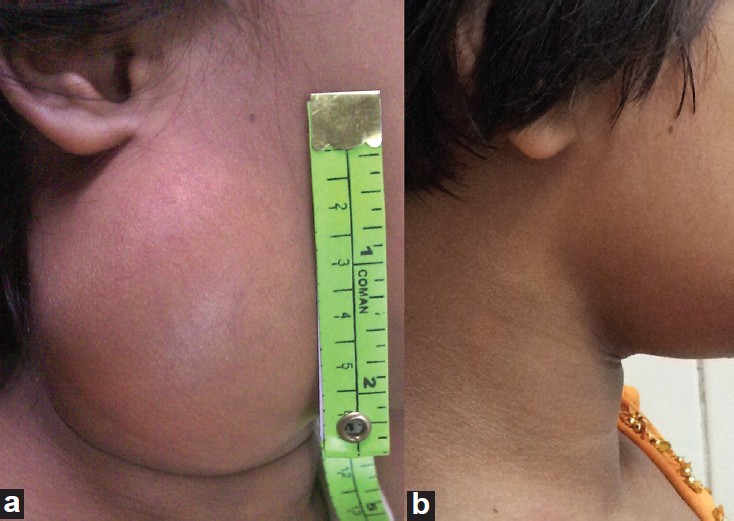 |
| Figure 1: (a) A 4 year old girl with right cervical lymphangioma (b) Follow up photograph 5 months after receiving single session of sclerotherapy |
 |
| Figure 2: (a) Coronal section of contrast enhanced computed tomography of chest showing a non-enhancing hypodense lesion in left axillary region (b) Follow up photograph 4 months after receiving two sessions of sclerotherapy |
Complete resolution was noticed in all 10 patients who had cervical or axillary lesions. In other three patients the response was near complete with and very small fibrotic or microcystic lesion. No recurrence or adverse event was noted at a mean follow up of 10 months.
Lymphangiomas are frequently seen vascular malformations and usually present in the head and neck region, as also seen in our study. Surgery has usually been the preferred treatment for lymphangiomas but due to ramifications and infiltrations of surrounding structures, the excision becomes difficult especially if vessels or nerves are surrounded. Therefore incomplete excision and inadvertent nerve injuries are not uncommon after surgical management. [1] Sclerotherapy is now being increasingly used to manage lymphangiomas.
Vast experience has been reported with OK-432 and bleomycin. Both these drugs have been proven to be efficacious and safe in majority of patients. Due to limited availability of OK-432, bleomycin is an appropriate choice of sclerosant. Intralesional bleomycin was used by Yura et al., [2] in treating 8 cystic hygroma patients in 1977. Since then multiple studies have reported favorable results of bleomycin sclerotherapy in management of children with lymphangiomas.
The dose of bleomycin usually recommended for sclerotherapy is 0.3-0.6 mg/kg, [3] but doses as high as 1 mg/kg have been given for intralesional sclerotherapy without major side effects. [4] We preferred to use of dosage of 0.6 mg/kg but have on 2 occasions administered higher doses for injection for large lesions without any adverse effects.
During the initial part of the study two sessions were performed under ultrasonographic guidance. During both these procedures the site marked by the radiologist was same as what we had determined clinically. Subsequently we injected all our patients without ultrasonographic guidance without any failure or complication.
Minor adverse effects like erythema and low grade fever are common but self-limiting. However, the major concerns with bleomycin use are the potential risks of interstitial pneumonia and pulmonary fibrosis. These complications have been associated with intravenous bleomycin administration exceeding the total cumulative dose of 400 mg. [5] Cumulative doses of bleomycin in management of lymphangiomas is much less and therefore these complications are unlikely.
We recommend intralesional bleomycin injection as a primary treatment in management of macrocystic lymphangiomas while reserving surgical excision for lesion where sclerotherapy fails.
| 1. |
Kennedy TL, Whitaker M, Pellitteri P, Wood WE. Cystic hygroma/lymphangioma: A rational approach to management. Laryngoscope 2001;111:1929-37.
[Google Scholar]
|
| 2. |
Yura J, Hashimoto T, Tsuruga N, Shibata K. Bleomycin treatment for cystic hygroma in children. Nihon Geka Hokan 1977;46:607-14.
[Google Scholar]
|
| 3. |
Wiegand S, Eivazi B, Zimmermann AP, Sesterhenn AM, Werner JA. Sclerotherapy of lymphangiomas of the head and neck. Head Neck 2011;33:1649-55.
[Google Scholar]
|
| 4. |
Mathur NN, Rana I, Bothra R, Dhawan R, Kathuria G, Pradhan T. Bleomycin sclerotherapy in congenital lymphatic and vascular malformations of head and neck. Int J Pediatr Otorhinolaryngol 2005;69:75-80.
[Google Scholar]
|
| 5. |
Orford J, Barker A, Thonell S, King P, Murphy J. Bleomycin therapy for cystic hygroma. J Pediatr Surg 1995;30:1282-7.
[Google Scholar]
|
Fulltext Views
4,896
PDF downloads
1,990





