Translate this page into:
Various techniques for marking patch test sites
Corresponding author: Dr. Neel Prabha, Department of Dermatology, All India Institute of Medical Sciences, Raipur, Chhattisgarh, India. ripuneel@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prabha N, Yadav H. Various techniques for marking patch test sites. Indian J Dermatol Venereol Leprol 2023;89:622–5.
Abstract
Patch test helps in identifying the allergen causing allergic contact dermatitis. Proper identification of the site of individual patch test allergen is very important for identifying the positive allergen. In this article, various techniques for markings patch test sites are discussed.
Keywords
Patch test
marking
Patch test helps in identifying the allergen causing allergic contact dermatitis. It is one of the commonest procedures performed in the dermatology outpatient department. The first reading of the patch test is taken at 48 hours and subsequent readings at 72 hours or 96 hours are obligatory. For some allergens like corticosteroids and aminoglycoside antibiotics, a reading between 120 and 240 hours is necessary.1
Proper identification of the site of individual patch test allergen is very important for identifying the positive allergen. For this, various techniques for markings patch test sites are available, which will be discussed in this article.
Techniques for marking patch test sites
These can be divided into:
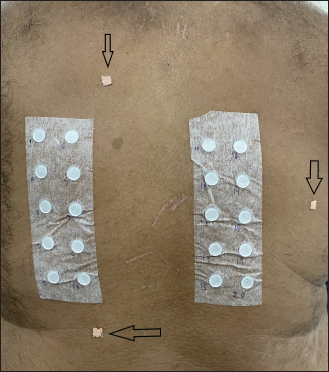
Marking pen, ink or dyes [Figures 1a-c]
Patch test mapping
Reading plates
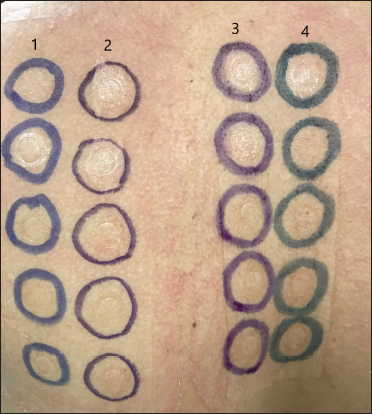
- Markings with permanent pen (1), surgical marker (2), gentian violet (3), triple dye (4) after removing patch
- Markings on 2nd day (72 hours of patch test application) showing faded permanent pen markings
- Markings on 3rd day (96 hours of patch test application) showing almost complete fading of permanent pen markings
Table 1 shows comparison between techniques for marking patch test sites.
| Method | Advantage | Disadvantage |
|---|---|---|
| Marking pen, ink or dyes | Readily available | Messy, stains clothing and skin, marking fades quickly, risk of allergic contact dermatitis to ink |
| Marking using patch test mapping. | Transparent sheet readily available, no risk of staining of skin or clothing, delayed reading can be recorded, and transparent sheet can be reused | No particular disadvantage |
| Reading plates | Less messy as there is no need to mark individual chamber | Available with a few patch test chambers only |
Marking pen, ink or dyes
Permanent surgical markers or fluorescent highlighter are recommended for marking patch test sites.2 After removal of the patch, outlining of the entire panel and the individual chamber is done with these markers.
A permanent surgical marker is readily available and is commonly used in clinical practice. However, there are certain drawbacks to permanent surgical marker.
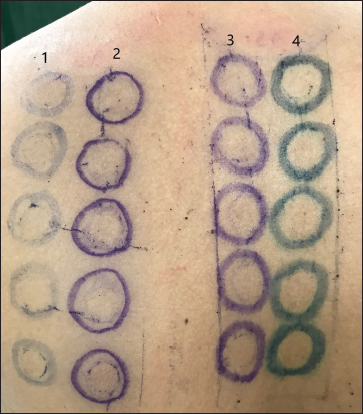
It is messy and stains clothing [Figure 2].
Skin moisture causes difficulty in marking.
The marking fades quickly. Fading will cause difficulty in locating the exact site of allergens leading to difficulty in interpreting late readings.
The marker does not last long. Petrolatum, tape adhesive residue and sebum damage their tip, increasing the overall cost.3
There is a risk of allergic contact dermatitis to making pen ink.4,5
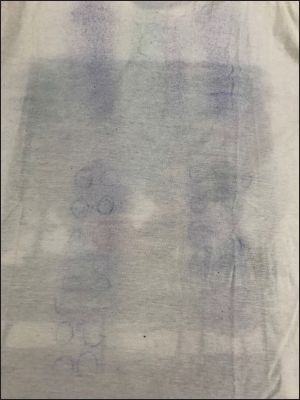
- Staining of cloth by marker ink
A fluorescent skin marker can also be used for marking.2,6 Wood lamp is needed to localize the markings. This technique has many advantages over permanent skin markers. In this technique, markings are not visible by the naked eye, less messy, do not stain clothing, and do not fade quickly; fluorescence persists for weeks even after bathing and is helpful for patients with darker skin tones. The problem with this is that it is not readily available, and Wood lamp is required for reading.
Dye solutions like gentian violet, Castellani paint and similar other dyes have also been proposed for markings the patch test sites.7 These are efficacious, readily available and economical for marking patch test sites compared to commercially available markers. Some commercially available markers have gentian violet and silver nitrate for prolonged skin staining.8 Skin moisture does not cause difficulty in marking with dyes. The main drawback is the staining of skin and clothing. For white-skinned individuals a concentrated solution of dihydroxyacetone in a mixture of water, alcohol and acetone can be used for marking. It does not stain clothing.7
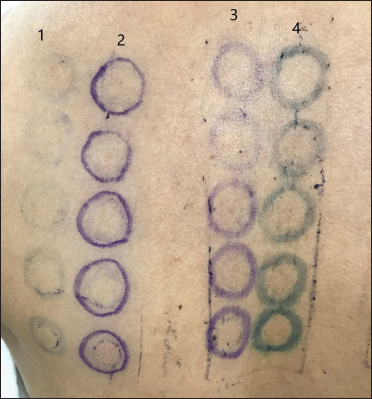
Marking using patch test mapping [Figures 3a-d]
In this technique, transparent plastic non-adherent sheets or commercially available patchMap are used.3,9 Immediately after applying the patch test, the transparent sheet is placed over the patient’s back, covering the patch panel. Outlining of panel and chambers is done over these sheets with an erasable pen. For alignment, certain landmarks like permanent skin lesions (moles, scars) are also marked. In case of the non-availability of these landmarks, artificial landmarks outside the patch (preferably at the periphery of the transparent sheet) are created and marked. When the patch is removed for reading, the sheet is applied to the patient’s back, according to marks of permanent or artificial landmarks. This helps in the identification of positive test sites. These sheets can be stored for delayed readings. This method has several advantages over other marking methods.3 There is no risk of staining of skin or clothing, and the patient can wash their back after the first reading, no risk of allergic reaction to inks, delayed reading can be recorded and inexpensive.
- In case of the non-availability of moles/scars, create artificial landmark by sticking adhesive elastic tape (arrow) outside the patch
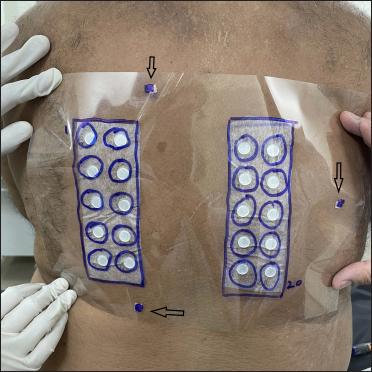
- Marking on A4 size overhead projector transparency sheet, just after patch application. Artificial landmarks are also marked (arrow)

- One positive reaction (arrow) after 30 minutes of patch removal; note that marking is not done on the patient’s skin
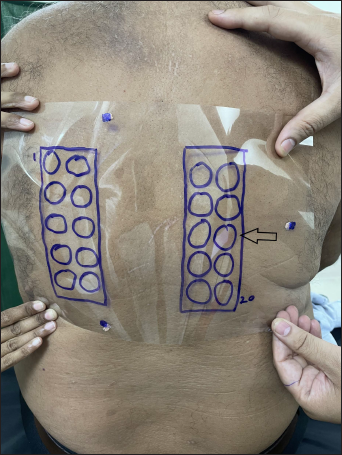
- Marked overhead projector transparency sheet is applied to the patient’s back, according to marks of artificial landmarks. This helped in the identification of positive test site
Reading plates
Reading plates identify the individual chamber sites without marking each site.10 These are plastic templates, that match the shape of the patch, and the holes in it match the individual chamber. In some reading plates pictures of grades of positivity are also provided for easy reading.
Conclusion
Identifying the exact site of individual allergens is very important while interpreting the patch test results. For this, various techniques of patch test markings have been described. All methods have some advantages or disadvantages. A permanent surgical marker is commonly used in clinical practice. However, it is messy and fades quickly. Patch map is a clean, patient-friendly and durable method.
Declaration of patient consent
Patient’s consent not required as identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- European Society of Contact Dermatitis guideline for diagnostic patch testing-Recommendations on best practice. Contact Dermatitis. 2015;73:195-221.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic Contact Dermatitis In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology (4th ed.). China: Elsevier; 2018. p. :242-261.
- [Google Scholar]
- Marking patch tests sites: Description of a practical, clean, durable and inexpensive method. Contact Dermatitis. 2003;49:284-6.
- [CrossRef] [PubMed] [Google Scholar]
- Contact allergy to 2-hydroxy-5-tert-butyl benzylalcohol and 2,6-bis(hydroxymethyl)—4-tert-butylphenol, components of a phenolic resin used in marking pens. Contact Dermatitis. 1994;31:154-6.
- [CrossRef] [PubMed] [Google Scholar]
- Allergy to patch test marking ink. Contact Dermatitis. 1994;30:182-3.
- [CrossRef] [PubMed] [Google Scholar]
- Procedure pearl: Patch testing, a light in the dark. Dermatitis. 2007;18:57-8.
- [CrossRef] [PubMed] [Google Scholar]
- Practical aspects of patch testing In: Rietschel RL, Fowler JF Jr, eds. Fisher’s Contact Dermatitis (6th ed.). Hamilton, Ontario: BC Decker Inc; 2008. p. :11-29.
- [Google Scholar]
- Patch test clinic start-up: From basics to pearls. Dermatitis. 2020;31:287-96.
- [CrossRef] [PubMed] [Google Scholar]
- Using a nonadherent transparent scribing sheet: Tip for allergen location in pediatric contact dermatitis testing. Pediatr Dermatol. 2014;31:410-1.
- [CrossRef] [PubMed] [Google Scholar]
- Patch testing tools of the trade: Techniques for marking and identifying patch application sites. J Dermatol Nurses Assoc. 2015;7:104-6.
- [Google Scholar]






