Translate this page into:
Verrucous growth on leg
2 Department of Skin and VD, SCB Medical College, Cuttack, Orissa, India
Correspondence Address:
P Mohanty
Department of Skin and VD, SCB Medical College, Cuttack, Orissa
India
| How to cite this article: Mohanty L, Mohanty P, Padhi T, Samantray S. Verrucous growth on leg. Indian J Dermatol Venereol Leprol 2006;72:399-400 |
 |
| Golden brown round structures within giant cells (H and E, 1000x) |
 |
| Golden brown round structures within giant cells (H and E, 1000x) |
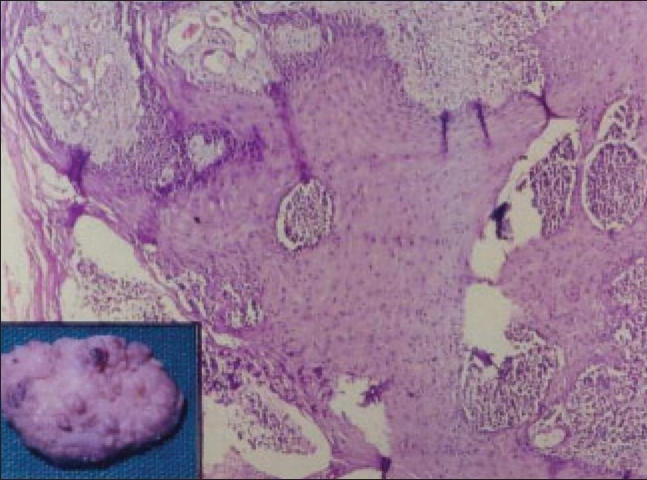 |
| Pseudoepitheliomatous hyperplasia and microabscesses in the superficial dermis (H and E, 100x) Inset - tumor-like mass with warty surface |
 |
| Pseudoepitheliomatous hyperplasia and microabscesses in the superficial dermis (H and E, 100x) Inset - tumor-like mass with warty surface |
 |
| Warty growth over dorsum of foot |
 |
| Warty growth over dorsum of foot |
A 65-year-old male presented with swelling, ulceration and a verrucous growth over the dorsum and lower one-third of the right leg of one-year duration, which was gradually increasing in size [Figure - 1]. He was treated with topical steroids and systemic antibiotics without any response. The patient did not have any other complaint and there was no other significant clinical finding. Routine hematological and biochemical investigations were within normal limits. It was subjected to surgical biopsy. The histopathological findings are shown in [Figure - 2][Figure - 3].
What is your diagnosis?
Diagnosis: Chromoblastomycosis
Histopathological findings Multiple sections stained with Hematoxyline and Eosin showed marked pseudoepitheliomatous hyperplasia and dense infiltration of polymorphs in the upper and mid-dermis forming micro-abscesses; golden brown round structures showing separation at places were observed within giant cells representing muriform cells (sclerotic bodies of pigmented fungal infection).
Discussion
Chromoblastomycosis is a chronic fungal infection caused by several genera of dematiaceous fungi, the commonest causative agent being Fonsecaea pedrosoi . It commonly occurs in tropical and subtropical countries, Caribbean regions, Africa, Australia and Japan. A number of cases have been reported from different parts of India.[1],[2] Chromoblastomycosis is commonly seen in the exposed parts of the lower extremities often following superficial trauma as it is caused by direct inoculation of the fungi.[3] Sites that may be involved less commonly are the penile shaft, vulva, ala of nose and also pleural cavity, ileocaecal region, laryngotracheal area and tonsils.[3]
There are several causative agents, however, the tissue forms of all appear identical. As the name implies, the clinical and histological appearance of the lesion closely resembles blastomycosis. A locally spreading verrucous plaque or solid nodule develops in the skin at the site of traumatic implantation. The histological response is granulomatous microabscesses and marked pseudoepitheliomatous hyperplasia which account for the verrucous tumor-like skin masses. Round thick-walled golden brown cells called muriform cells or sclerotic bodies are grouped within the superficial dermis where the fungus elicits a suppurative inflammation. These sclerotic bodies are 5-12 m in diameter and are diagnostic of chromoblastomycosis. Special stains are not necessary because of the intrinsic pigmentation. The sclerotic bodies reproduce by bipartition in one or two planes, which may rarely be observed within the lesions. The pseudoepitheliomatous hyperplasia is probably the mechanism by which the transepithelial elimination of the fungus takes place.
This condition is often clinically indistinguishable from tuberculosis verrucosa cutis because of the verrucous appearance. Squamous cell carcinoma has been reported with extensive chromoblastomycotic lesions of long duration.[4] There are also reports of the condition masquerading as palmo-plantar psoriasis and sporotrichosis.[5],[6]
Early stages of chromoblastomycosis are treated with surgical excision, electrodesiccation, cryosurgery or topical antifungals. Advanced cases may require systemic antifungals for long periods of time. Itraconazole and terbinafine are the drugs of choice.
| 1. |
Kumar K, Sarin RC. Chromoblastomycosis. Indian J Deramatol Venereol Leprol 1978;44:310-5.
[Google Scholar]
|
| 2. |
Rajendran C, Ramesh V, Mishra RS, Kandhari S, Upreti HB, Datta KK. Chromoblastomycosis in India. Int J Dermatol 1997;36: 29-33.
[Google Scholar]
|
| 3. |
Sharma NL, Sharma RC, Grover PS, Gupta ML, Sharma AK, Mahajan VK. Chromoblastomycosis in India. Int J Dermatol 1999;38:846-51.
[Google Scholar]
|
| 4. |
Boogaerts M, Maertens J. Clinical experiences with Itraconazole in systemic fungal infections. Drugs 2001;61:39-47.
[Google Scholar]
|
| 5. |
Lakshmi TS, Rao G, Shekhar VA. Chromoblastomycosis masquerading as palmo-plantar psoriasis. Indian J Dermatol Venereol Leprol 1999;65:83-4.
[Google Scholar]
|
| 6. |
Nair PS, Sarojini PA. Chromoblastomycosis resembling sporotrichosis. Indian J Dermatol Venereol Leprol 1993;59: 125-6.
[Google Scholar]
|
Fulltext Views
5,269
PDF downloads
3,506





