Translate this page into:
Verrucous growth on the glans penis: A clinical conundrum!
Corresponding author: Dr. Anshuman Dash, Department of Dermatology and Sexually Transmitted Diseases, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. dranshu.derma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dash A, Srivastava P, Khunger N, Sharma S. Verrucous growth on the glans penis: A clinical conundrum! Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1790_2024
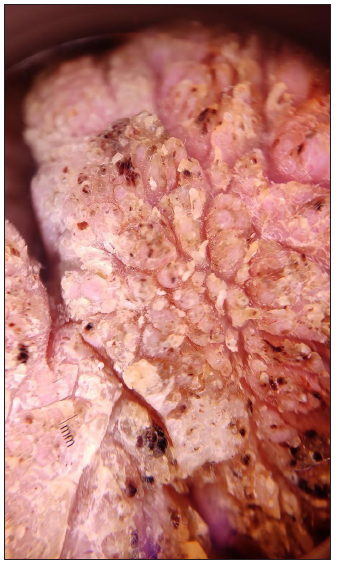
A 42-year-old uncircumcised man presented with a slow-growing exophytic growth involving glans and prepuce for 10 years associated with progressive difficulty in voiding and intercourse. On cutaneous examination, a diffuse verrucous growth with haemorrhagic dots and crusting was noted over the glans and under-surface of the prepuce. There was associated paraphimosis, stricture, and compartmentalisation of the meatal opening [Figure 1]. Regional lymph nodes were not palpable. Dermoscopy revealed multiple knob-like structures interspersed with areas of keratosis, haemorrhagic foci, and crusts [Figure 2]. Serology for HIV and syphilis were negative. Consequently, two biopsy specimens were obtained from different sites. The histopathological examination (HPE) demonstrated marked hyperkeratosis, focal parakeratosis, and acanthosis with papillomatosis. Moderate peri-vascular lympho-histiocytic infiltrate was present in the papillary dermis [Figures 3a and 3b]. No koilocytic change or dysplasia was observed even on repeated biopsies from different areas. Polymerase chain reaction (PCR) analysis from urethral swab and a tissue sample was negative for Human Papillomavirus.

- Verrucous growth with haemorrhagic dots and crusting present over glans and the under-surface of the prepuce.
- Dermoscopic image showing multiple knob-like structures with areas of keratosis, crusting, and haemorrhagic dots. (Dermlite DL3N, dry, contact, 10x).
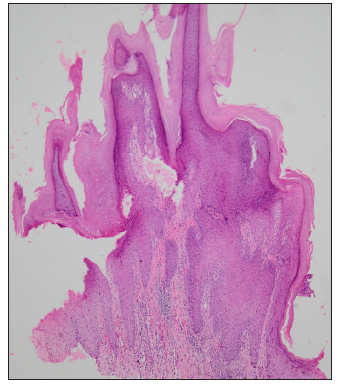
- Microphotograph showing marked hyperkeratosis, focal parakeratosis, and acanthosis with papillomatosis. (Haematoxylin & eosin, 40x).
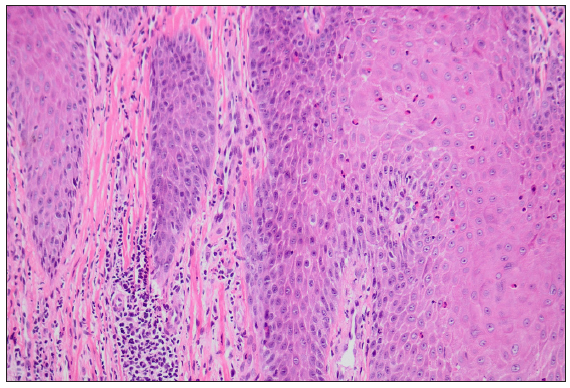
- Higher magnification showing epidermal keratinocytes with mild eosinophilic exocytosis and lymphohistiocytic inflammation in the papillary dermis. (Haematoxylin & eosin, 200x).
Question
What is your diagnosis?
Answer
Diagnosis: Pseudoepitheliomatous Keratotic and Micaceous Balanitis (PKMB)
Discussion
PKMB is a rare non-venereal dermatosis that is considered a premalignant condition by some authors. The clinical manifestations may vary as it evolves through distinct stages, including the initial plaque stage, late tumour stage, verrucous stage, and ultimately transformation into invasive squamous cell carcinoma (SCC).1 The characteristic presentation includes a well-defined thick hyperkeratotic plaque on the glans with adherent micaceous scaling. The condition, is usually asymptomatic, but may be associated with a burning sensation, fissuring or maceration. Rarely, extensive involvement of the peri-meatal skin, as in our case, may result in multiple streams on micturition, presenting an appearance of a watering-can penis.2 Initially, it was considered a benign entity, but later reports have established its progression into verrucous carcinoma.3
Histopathology is diagnostic in most cases showing acanthosis, hyperkeratosis, and pseudoepitheliomatous hyperplasia with no cytological atypia or koilocytes.1 The atypia may become evident upon malignant transformation. The close differentials of PKMB include Buschke-Lowenstein tumour and verrucous squamous cell carcinoma [Table 1].
| Differentials | Clinical presentation | Histopathology | Dermoscopy |
|---|---|---|---|
| PKMB | Well-defined thick hyperkeratotic plaque with micaceous scaling on glans | Hyperkeratosis, acanthosis, pseudoepitheliomatous hyperplasia without koilocytes or atypia | Knob-like structures with areas of haemorrhage and crusting |
| Buschke-Lowenstein tumour/giant condyloma acuminata | Slow-growing keratotic plaque that transforms into a cauliflower-shaped exophytic tumour | Papillomatosis with fibrovascular cores and prominent koilocytosis | Knob-like structures of varying lengths with haemorrhage |
| Verrucous carcinoma of the penis | Slow-growing, non- metastasising warty plaque on the glans | Prominent hyperkeratosis, broad, blunt rete ridges, pushing margins well-differentiated tumour cells with keratinisation and basal cell atypia. May or may not show infiltration of tumour cells into the dermis. | Yellowish-white structureless areas, white clods and circles, polymorphous vessels (looped or glomerular) |
Buschke-Lowenstein (BL) tumour, also known as giant condyloma acuminata, is a slow-growing anogenital tumour with a propensity for local invasion. It starts as a keratotic plaque on the glans or foreskin and gradually transforms over the years into a large verrucous or cauliflower-shaped tumour. Human Papillomavirus (HPV) types 6 and 11 are the most commonly implicated. Dermoscopy reveals multiple finger/knob-like projections of varying lengths fusing at their bases and dilated linear vessels haemorrhaging at their tips.4 HPE demonstrates papillomatosis with fibrovascular cores and prominent koilocytosis.5 In this case, PCR analysis was negative for HPV and HPE failed to demonstrate koilocytes, thereby ruling out BL tumour.
Verrucous carcinoma (VC) is a low-grade, well-differentiated squamous cell carcinoma. It usually presents as a slow-growing warty plaque on anogenital mucosa and has a predilection for local invasion. Dermoscopy is conspicuous demonstrating keratinisation with white to yellow structureless areas, white clods, and circles in addition to polymorphous vessels (looped or glomerular).6 HPE is diagnostic, showing prominent hyperkeratosis, broad and blunted rete ridges with thin fibrovascular cores, pushing margins, well-differentiated tumour cells, and foci of keratinisation interspersed with basal cell atypia.7 Both atypia and focal keratinisation were absent in our case, even on repeated biopsies. PKMB is a rare entity and should always be considered as a differential for verrucous penile growths. In the absence of malignant changes, the treatment is typically conservative, with options like topical 5-Fluorouracil (5-FU), cryotherapy and radiotherapy.2 Local excision becomes necessary when cellular atypia or frank malignant changes are evident. In our case, initial application of 5-FU for 3-4 months yielded minimal improvement. Subsequently, owing to increasing difficulties in micturition, a partial penectomy was performed. It is crucial to follow-up on all PKMB cases, regardless of their treatment statuses, to monitor for recurrence or malignant transformation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Pseudoepitheliomatous, keratotic and micaceous balanitis. Case report and review of the literature. Urol Int. 1996;56:125-8.
- [CrossRef] [PubMed] [Google Scholar]
- ‘Watering-can penis’ in pseudoepitheliomatous, keratotic and micaceous balanitis. Acta Derm Venereol. 2004;84:329-30.
- [CrossRef] [PubMed] [Google Scholar]
- Is pseudoepitheliomatous, micaceous and keratotic balanitis synonymous with verrucous carcinoma? Br J Dermatol. 1987;117:641-6.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of dermoscopy in anogenital warts: A descriptive study of 30 cases. JEADV Clin Pract [Internet] 2024 [cited 2025 Jan 4]; Available from: http://dx.doi.org/10.1002/jvc2.545. Last accessed: 2025 Jan 7
- [CrossRef] [Google Scholar]
- Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum. 1994;37:950-7.
- [CrossRef] [PubMed] [Google Scholar]
- Two cases of squamous cell carcinoma of the penis - A dermoscopic view. Dermatol Pract Concept. 2020;11:e2020097.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous verrucous carcinoma: A clinicopathological study of 21 cases with long-term clinical follow-up. Front Oncol. 2022;12:953932.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






