Translate this page into:
Viva questions from the IJDVL
2 Department of Dermatology, K J Somaiya Medical College and Research Centre, Sion, Mumbai, Maharashtra, India
Correspondence Address:
Vishalakshi Viswanath
Department of Dermatology, Rajiv Gandhi Medical College, Thane, Maharashtra
India
| How to cite this article: Viswanath V, Vasani R. Viva questions from the IJDVL. Indian J Dermatol Venereol Leprol 2015;81:657-662 |
Targeted Phototherapy
What is targeted phototherapy?
Targeted phototherapy, focused phototherapy or microphototherapy involves the application of light energy directly focused on a targeted lesion through special delivery mechanisms such as fiber optic cables. Targeted phototherapy includes:
- Excimer laser
- Intense pulsed light
- Light-based targeted phototherapy
- Photodynamic therapy
- Low level laser and light emitting diode therapy.
What is the mechanism of action of targeted phototherapy devices?
Most targeted phototherapy devices (laser or non-laser type) emit radiation in the ultraviolet B range with peak emission in the narrow band wavelength (around 308–311 nm) while some nonlaser systems emit ultraviolet A radiation also. The 308 nm xenon chloride laser uses noble gas with halogen as the lasing material.
Ultraviolet B radiation induces alteration of cytokine production, local immunosuppression, stimulation of melanocyte stimulating hormone, increased melanocyte proliferation and melanogenesis. In targeted phototherapy, all these effects are induced in a more aggressive fashion because of delivery of super-erythemogenic doses of radiation.
What are the indications of targeted phototherapy?
Common indications of targeted phototherapy include:
- Stable vitiligo – localized vitiligo that is resistant to the other modalities of treatment
- Psoriasis – localized resistant lesions on the hands and knees, scalp psoriasis
- Other indications – oral lichen planus, atopic dermatitis, mycosis fungoides, lymphomatoid papulosis, hypopigmented striae and scars.
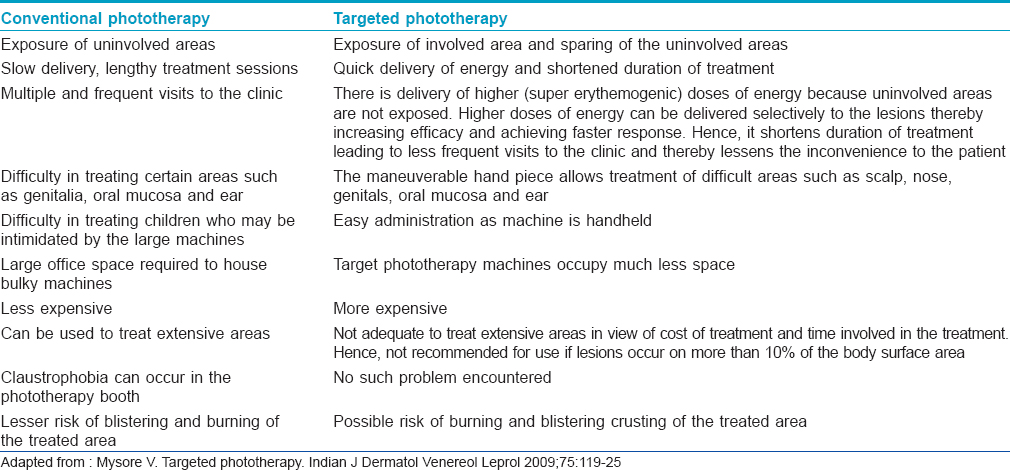
What are the differences between targeted phototherapy and conventional phototherapy?
The salient differences between conventional and targeted phototherapy have been outlined in [Table - 1].
Toxic Epidermal Necrolysis
What are the common drugs causing Steven–Johnson syndrome/toxic epidermal necrolysis?
Steven–Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) can be caused by any drug, but the high-risk drugs are carbamazepine, phenytoin, allopurinol, lamotrigine, oxicam and other nonsteroidal anti-inflammatory drugs, sulfonamide antibiotics and nevirapine.
What are the infections that can cause toxic epidermal necrolysis?
Mycoplasma and cytomegalovirus infections can cause toxic epidermal necrolysis.
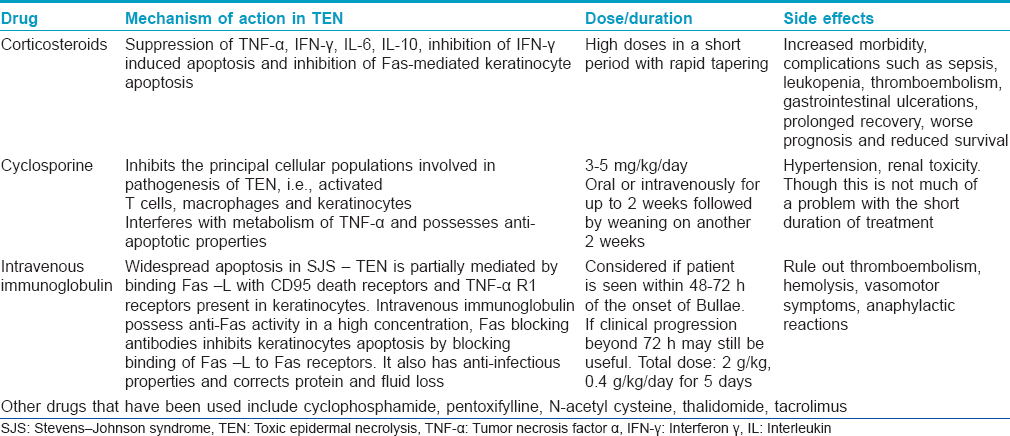
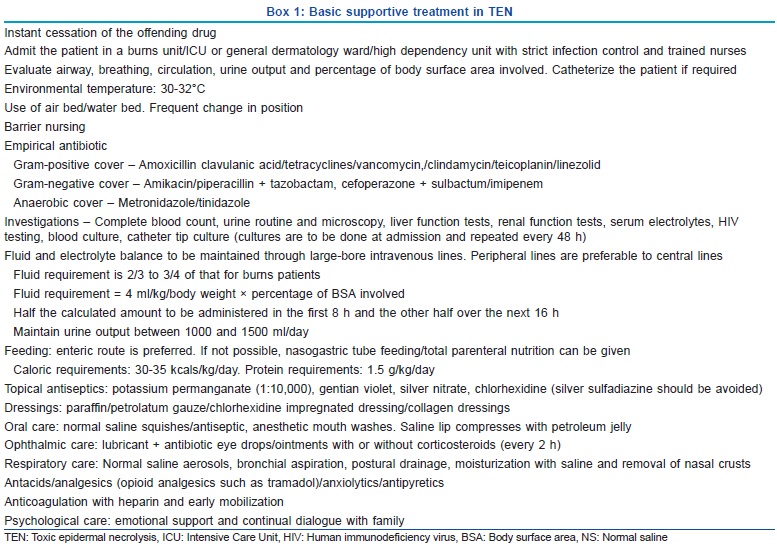
Briefly outline the management of toxic epidermal necrolysis
Management of toxic epidermal necrolysis involves basic supportive treatment along with the use of specific drugs. These have been outlined in Box 1 and [Table - 2].
What are signs of sepsis in cases of toxic epidermal necrolysis?
- General deterioration of the patient
- Hypothermia
- Fever/shivering
- Diminishing level of consciousness
- Falling urine output
- Deterioration of respiration
- Loss of diabetic control
- Failure of gastric emptying
- Sudden change in the condition.
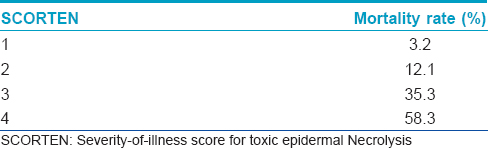
What is SCORTEN (severity-of-illness score for toxic epidermal necrolysis)?
"SCORTEN” (severity-of-illness score for toxic epidermal necrolysis) is a validated mathematical tool for prognostication of Steven–Johnson syndrome/toxic epidermal necrolysis patients. It should be computed within 24 h after admission and again on the third day. The index identifies the following seven independent risk factors for death.
- Age above 40 years
- Presence of malignancy
- Tachycardia (heart rate above 120 beats/min)
- Initial percentage of epidermal detachment above 10%
- Blood urea nitrogen above 28 mg/dl
- Serum glucose above 252 mg/dl
- Bicarbonate level <20 mmol/L.
Each parameter is given a score of one and the total score is calculated by summing up the number of abnormal parameters. [Table - 3] shows the mortality rate according to SCORTEN score. The most common causes of death are sepsis, pulmonary failure and multiple organ failure.
Icthyosis Bullosa of Siemens
What is mauserung phenomenon?
A distinctive feature of ichthyosis bullosa of Siemens which is not present in other forms of ichthyosis is called mauserung phenomenon (mauserung in German means “moulting” and was first described by Dr. H W Siemens). These are small patches of bare apparently normal skin (due to regeneration of the epidermis) in the middle of areas of hyperkeratosis. It is frequently seen at hyperkeratotic flexures and acral sites, especially on the dorsa of the hands and feet.
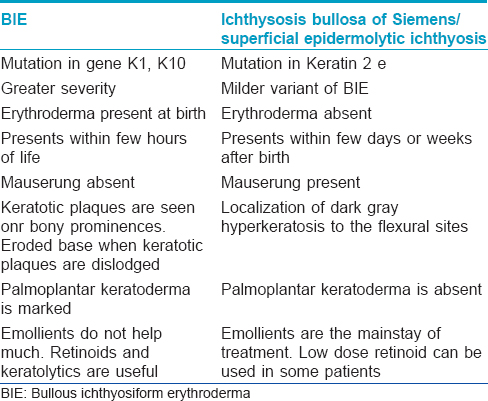
Enumerate the differences between bullous ichthyosiform erythroderma and ichthyosis bullosa of Siemens
The salient differences have been outlined in [Table - 4].
What is keratinopathic ichthyosis?
The term epidermolytic hyperkeratosis describes the characteristic light microscopic observation of intracellular vacuolization, clumping of tonofilaments and formation of small intraepidermal blisters and is commonly seen in ichthyosis due to keratin mutations. Therefore, the term epidermolytic hyperkeratosis is used (by some) as synonymous with bullous ichthyosis, ichthyosis exfoliativa, bullous congenital ichthyosiform erythroderma (of Brocq), ichthyosis bullosa of Siemens. To simplify the nomenclature, Vinzenz et al. proposed the umbrella term of “keratinopathic ichthyosis."
Ochronosis
Enumerate the various types of ochronosis
Exogenous ochronosis is commonly due to topical hydroquinone use; other causative agents include phenol, resorcinol, mercury, picric acid, benzene and systemic antimalarial-like quinine. These agents inhibit homogentisic acid oxidase in the skin resulting in local accumulation of homogentisic acid which then polymerizes into the ochronotic pigment.
Endogenous ochronosis or alkaptonuria is an inborn error of metabolism. It is an autosomal recessive disease caused by a deficiency of homogentisic acid oxidase resulting in the accumulation of homogentisic acid in various tissues such as cartilage, tendons, ligaments or sclerae and is associated with dark urine.
Idiopathic ochronosis is characterized by the absence of use of any drug, features of alkaptonuria are absent and laboratory tests of blood and urine are negative.
Describe the histopathological features of ochronosis
Classical ochronosis shows the characteristic ochre or yellow-brown pigment. The pigment is present within collagen bundles which tend to fracture transversely resulting in pointed ends. Hence, these have been described as banana-shaped fibers or comma-shaped structures. Fine granules of ochronotic pigment may also be seen intracellularly in the endothelium, macrophages and secretory cells of sweat glands, as well as extracellularly, particularly in basement membranes. Collagen degeneration or granuloma formation may be occasionally seen. The ochronotic pigment does not stain with silver nitrate but shows blackish coloration with methylene blue or cresyl violet staining.
Crusted Scabies
What is crusted scabies?
Crusted scabies is a distinct clinical subtype of scabies occurring due to hyperinfestation by Sarcoptes scabiei with the mites numbering in millions. It was first described in Norway in 1848. It develops due to a Th1/Th2 imbalance, with a cytotoxic T-cell type 2 response in the skin, high levels of antibody in the blood and uncontrolled growth of the parasite.
Enumerate the underlying conditions associated with crusted scabies
Crusted scabies is associated with immunosuppressed states due to topical or systemic glucocorticoid therapy, human immunodeficiency virus infection, human T lymphotropic virus 1 infection, T-cell lymphoma and leukemia or following organ transplant. It has also been noted in physically or mentally handicapped, senile bedridden individuals or patients with neurological diseases such as Parkinson's disease, Down's syndrome and patients with poor sensory perception (due to leprosy, spinal injury, syringomyelia, etc.). It has also been associated with previously treated leprosy, substance abuse, systemic lupus erythematosus, pulmonary tuberculosis, diabetes mellitus and hepatitis B. It has also been documented as a manifestation of immune reconstitution inflammatory syndrome in human immunodeficiency virus infection.
Enumerate the differential diagnosis of crusted scabies
Clinical presentation of crusted scabies includes hyperkeratotic crusted lesions on the hands and feet with deformed nails, generalized erythematous scaly rash and lesions on the scalp. Crusted scabies can mimic psoriasis, hyperkeratotic eczema, contact dermatitis, cutaneous lymphoma, Darier's disease or lichenoid dermatosis.
Describe the dermatoscopic and reflectance mode confocal microscopic findings in scabies
Both these techniques are non-invasive methods for the diagnosis of scabies. The mite, eggs and fecal pellets can be demonstrated.
The “jet with contrail” appearance of the mite in its burrow on dermatoscopy is characteristic.
Reflectance-mode confocal microscopy is a novel non-invasive imaging technique for skin structures and lesions at a resolution comparable to that of conventional histology. With this technique, the burrows can be detected as multiple tortuous large segments in the stratum corneum and at the end of the burrows, mites can be identified. Roundish, refractile, oval particles corresponding to eggs and mite feces can also be visualized. Parakeratosis is demonstrated by the presence of highly refractile round to polygonal structures.
Cutis Verticis Gyrata
Describe the clinical features of cutis verticis gyrate
Cutis verticis gyrata is a rare condition wherein the skin on the scalp is thickened and thrown into folds forming deep furrows and convoluted ridges, resembling the gyri and sulci of the cerebral cortex.
Classify the types of cutis verticis gyrata
Cutis verticis gyrata is classified into primary and secondary types.
The primary form is characterized by an essentially normal histopathology of the skin. It is divided based on the absence or presence of underlying neurological and ophthalmological abnormalities into essential and non-essential, respectively. The abnormalities may include impaired cognition, learning difficulties, cerebral palsy, schizophrenia, microcephaly, deafness, cataracts, retinitis pigmentosa and strabismus.
Secondary cutis verticis gyrata may occur secondary to various diseases. These include:
- Endocrine diseases (acromegaly, myxedema, Grave's disease, diabetes mellitus)
- Hereditary disorders (pachydermoperiostosis, Turner syndrome, Noonan syndrome, Ehlers–Danlos syndrome, Beare–Stevenson syndrome, Fragile X syndrome, Klinefelter syndrome, “Michelin tire baby” syndrome, tuberous sclerosis, hyperimmunoglobulin E syndrome)
- Inflammatory cutaneous diseases (eczema, psoriasis, Darier's disease, folliculitis, impetigo, erysipelas, atopic dermatitis, acne conglobata, acanthosis nigricans)
- Infections (syphilis)
- Benign tumors/infiltrates (dermatofibroma, cerebriform intradermal nevus, neurofibroma, neurinoma, collagenoma, focal mucinosis, amyloidosis, intraventricular ependymoma, cutaneous leiomyomatosis, cutaneous neurocristic hamartoma)
- Malignant tumors (fallopian tube carcinoma, infiltrating ductal carcinoma, angiosarcoma, malignant melanoma, acute myelogenous leukemia, acute monoblastic leukemia).
Dowling–degos Disease
Describe the clinical features of Dowling–Degos disease
Dowling–Degos disease is a rare autosomal dominant genodermatosis occurring due to a loss-of-function mutation in keratin 5 gene.
It is characterized by reticulate hyperpigmentation of flexural sites such as the neck, axilla, cubital fossa and groin and hence termed as reticulate pigmented anomaly of the flexures.
The pigmentation is typically symmetrical and progressive; it may become confluent, with a brown or black lace-like pattern. Comedo-like lesions may be seen on the trunk and face and pitted acneiform scars can occur at the angles of the mouth.
Enumerate other associated conditions occurring with Dowling–Degos disease
Dowling–Degos disease may overlap with acropigmentation of Kitamura and Haber's syndrome and can occur in association with hidradenitis suppurativa. Dowling–Degos disease is a benign condition; rarely, some tumors have been reported: squamous cell carcinoma, keratoacanthoma and a recent report of metastatic amelanotic melanoma.
Describe the histological features of Dowling–Degos disease
The histological features are characteristic; a distinctive acanthosis is seen and is characterized by an irregular elongation of thin branching rete ridges, with a heavy concentration of melanin at the tips. Follicular plugging and horn cysts may be present.
Keratosis Follicularis Spinulosa Decalvans
What is the inheritance of keratosis follicularis spinulosa decalvans?
Keratosis follicularis spinulosa decalvans was first described by Siemens in 1926 and has an X-linked recessive mode of inheritance. It occurs due to a missense mutation in the membrane-bound transcription factor peptidase site 2 gene which leads to disturbed epidermal differentiation due to inhibition of cholesterol biosynthesis.
Describe the clinical features of keratosis follicularis spinulosa decalvans
A progressive cicatricial alopecia of the scalp, eyebrows and eyelashes starts in late childhood and remits by adolescence. It begins as follicular papules on the affected areas; there may be pustular flares and further progression to scarring alopecia. Focal plantar keratoderma may be present. Ocular abnormalities include photophobia, corneal opacities and blepharitis may occur. Oral manifestations include absent or conoid teeth, dental caries and enamel hypoplasia. Thickened dystrophic nails and high cuticles have been described.
What are the treatment modalities for keratosis follicularis spinulosa decalvans?
Topical keratolytic agents and emollients give symptomatic improvement. Antibiotics may be necessary during pustular flares of disease. Oral retinoids are effective in the early phase of the disease when active perifollicular infiltrate present. It must be continued for 6–12 months for optimum response.
Ascher Syndrome
What are the components of Ascher syndrome?
Ascher syndrome is characterized by blepharochalasis, progressive enlargement of the upper lip, and non-toxic goiter, but all the features may not be seen in every case. There may be inflammation and hypertrophy of labial salivary glands and accessory salivary glands.
Enumerate the differential diagnose of Ascher syndrome
Ascher syndrome is commonly confused with Melkersson–Rosenthal syndrome; other conditions being hereditary angioneurotic edema, early-onset dermatochalasis and acquired cutis laxa. Mounier–Kuhn syndrome can also have similar features, in addition to congenital tracheobronchomegaly.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Fulltext Views
7,274
PDF downloads
2,954





