Translate this page into:
Viva questions from the IJDVL
2 Department of Dermatology, K J Somaiya Medical College and Research Centre, Mumbai, Maharashtra, India
Correspondence Address:
Vishalakshi Viswanath
Department of Dermatology, Rajiv Gandhi Medical College, Thane, Maharashtra
India
| How to cite this article: Viswanath V, Vasani R. Viva questions from the IJDVL. Indian J Dermatol Venereol Leprol 2016;82:360-366 |
Focus Topic
What are the nail findings in [Figure - 1]?
 |
| Figure 1: Describe the nail findings and spot the diagnosis |
Distal onycholysis with salmon patch is seen suggesting a diagnosis of nail psoriasis.
What is the significance of nail psoriasis?
Nail psoriasis when associated with distal interphalangeal involvement is indicative of more severe arthritis. The close anatomical link between nail unit and distal interphalangeal joint is possibly responsible. Inflammation of the extensor tendon entheses, which are the attachment points of ligaments and tendon joint capsules to bone, can extend to the nail unit and can result in psoriatic nail changes.
There is a positive association between nail involvement and duration of skin lesions and its severity and the severity of skin and joint involvement. However, nail psoriasis occurs in 40% of people with mild psoriasis as well.
Nail involvement can severely affect the quality of life of a patient.
What is the percentage of patients of psoriasis and psoriatic arthritis who show nail involvement?
Nail involvement in psoriasis occurs in 50% of patients. About 70–80% of patients with psoriatic arthritis show nail psoriasis.
What are the clinical manifestations of nail psoriasis?
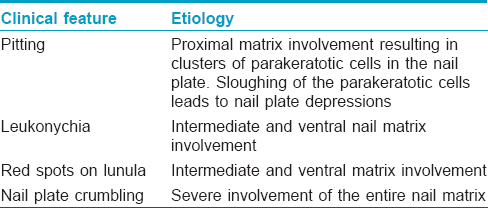
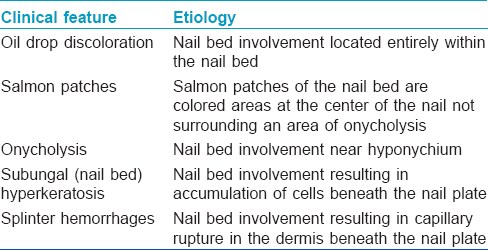
The clinical manifestations depend on the part of the nail affected. Clinical manifestations due to nail matrix involvement and nail bed involvement are outlined in [Table - 1] and [Table - 2]. Other manifestations include onychorrhexis and Beau's lines.
What is the most common sign of nail psoriasis?
Pitting is the most common manifestation of nail psoriasis. The pitting in psoriasis is irregular indepth and distribution on the nail plate versus the regular shallow pits seen in alopecia areata which can give a Scotch plaid appearance.
What is the clinical characteristic of onycholysis in psoriasis?
Onycholysis in psoriatic nails occurs with a characteristic erythematous border or a yellow-pink band at the proximal margin which indicates psoriatic involvement of the nail bed and can be seen clinically and better appreciated through a dermatoscope.
Enumerate various scoring systems for nail psoriasis and describe nail psoriasis severity index
Various scoring systems for assessing severity of nail psoriasis include nail psoriasis severity index, modified nail psoriasis severity index, target nail psoriasis severity index, psoriasis nail severity score, Baran's scoring system and Nijmegen nail psoriasis activity index.
Nail psoriasis severity index is an objective and reproducible tool for estimating nail involvement and which therefore can be used to determine efficacy of therapeutic interventions. Each nail is divided into four quadrants which are evaluated for the presence of any manifestation of psoriasis in the nail matrix (pitting, leukonychia, nail plate crumbling) and nail bed (oil drop discoloration, onycholysis, subungual hyperkeratosis, splinter hemorrhages). If any sign is present in all four quadrants, the nail is given a score of 4 through a score of 0 if there are no signs in any quadrant. Each nail is assigned a nail matrix and nail bed score of 0–4 which are combined to yield a total score of 0–8 for each nail. All nails may be evaluated with the total nail psoriasis severity index score being the sum of the scores up to 80 if only finger nails are considered or up to 160 if toe nails are included. A modified version of nail psoriasis severity index has also been validated and used for assessment of a single target nail. The modified nail psoriasis severity index assigns a severity score of 0–3 for each quadrant of the target nail.
What are the treatment modalities for nail psoriasis?
The treatment of nail psoriasis can be decided depending on the severity of nail psoriasis.
Mild cases of nail psoriasis
When nail psoriasis is limited to one or two nails and is not associated with significant symptoms or functional impairment.
- First-line therapy: Monotherapy with topical corticosteroid or topical vitamin D analog or combination treatment with topical corticosteroid and vitamin D analog
- Second-line therapy: Topical tacrolimus or topical tazarotene.
Moderate to severe nail psoriasis
When there is marked nail dystrophy involving >2 nails or nail psoriasis is associated with significant symptoms or functional impairment.
- First-line therapy: Systemic treatment with biologic agent, adalimumab, etanercept, infliximab, certolizumab pegol and golimumab have demonstrated moderate to high efficacy
- Second-line therapy: Methotrexate, apremilast, topical medications, intralesional corticosteroids, pulsed-dye laser therapy
- Additional therapies: Topical cyclosporine, oral acitretin/cyclosporine, phototherapy.
Pure Neuritic Hansen Disease
When should one suspect pure neuritic Hansen?
In endemic countries such as India, the presence of “mononeuritis” or “mononeuritis multiplex” along with tender enlarged nerves should always raise a suspicion of the diagnosis.
What are the patterns of nerve involvement and clinical features of pure neuritic leprosy?
Upper limbs (ulnar nerve most common) are more commonly involved as compared to the lower limbs (lateral popliteal nerve > posterior tibial nerve > sural nerve).
Mononeuritis is the most common presentation. Involvement of multiple unrelated and distal nerve trunks can also occur as mononeuritis multiplex.
The clinical presentation can be as follows:
- Sudden appearance of numbness with or without ulcers/fissuring
- Deformity or muscle weakness in a limb
- Nerve pain associated with neuritis
- Sudden increase in neuritis associated with increase in nerve function impairment as a part of type 1 reaction.
What are the histopathological changes in cases of pure neuritic leprosy occurring in the nerve and skin?
- Nerves: The histological spectrum that can be seen in the nerves affected by pure neuritic leprosy varies from tuberculoid to lepromatous with moderate to heavy load of acid fast bacilli within the nerves, even when the skin smears are negative
- Skin: Although clinically the skin looks normal, histopathology may show a varied presentation from non-specific inflammation in the dermis with perineural inflammation to epithelioid/macrophage granulomas.
What are the complications of pure neuritic leprosy?
The complications of pure neuritic leprosy are as follows:
- Nerve abscess: Usually, a cold abscess that is relatively painless or with only mild nerve pain may develop. The size of the abscess does not indicate the extent of resulting nerve function impairment and even a small intraneural abscess can lead to significant nerve function impairment depending on its location within the nerve
- Segmental necrotizing granulomatous neuritis: This manifests as single or multiple nodules of varying sizes along the course of a thickened peripheral nerve. Nerve biopsy shows a thickened nerve with multiple foci of caseous necrosis bordered by epithelioid cells and lymphocytes
- Disability and deformity: There is early occurrence of World Health Organization grade 1 disability and further progression to grade 2 disability.
What are the investigations that can be done in pure neuritic leprosy?
- Bedside tests: Semmes-Weinstein monofilament testing, voluntary muscle testing
- Nerve biopsy: It is the gold standard. Common sites of nerve biopsy are as follows:
- Superficial sensory radial nerve branch at the wrist
- Ulnar cutaneous nerve near the ulnar border of base of hand
- Sural nerve near the ankle
The nerve biopsy is further subjected to hematoxylin and eosin and Fite-Faraco staining.
- Fine needle aspiration cytology: It is a safe, less invasive procedure. Aspiration is carried out by a 22-gauge needle inserted along the length of the nerve. Negative aspirate does not rule out leprosy and can be attempted on the nerve before deciding on a nerve biopsy
- Polymerase chain reaction: It is a valuable tool in diagnosing leprosy in difficult situations such as pure neural cases, paucibacillary cases, and patients with atypical clinical presentation having histological features compatible with leprosy
- Nerve conduction studies: The electromyographic pattern of leprosy neuropathy described in the literature is impairment of conduction of nerve impulse and decreased amplitude of sensory motor potentials. However, the results can be nonspecific
- Neural imaging: Magnetic resonance imaging and high-resolution ultrasound are useful imaging modalities for diagnosis of pure neuritic leprosy, of which high-resolution ultrasound is an efficient, user-friendly, economical and widely applied modality. It provides information on the exact location of the nerve enlargement and neuritis can be detected by color Doppler which shows increased blood flow signals of endoneurial and perineural tissue. It is of great value in clinical situations where thickening is equivocal when there is motor/sensory deficit with apparently normal nerves or to confirm fibrosis, abscess or calcification in the nerve trunk.
Elaborate the management of pure neuritic leprosy
According to the National Leprosy Eradication Programme guidelines, when one nerve trunk is involved, it is considered paucibacillary and when more than one nerve trunk is involved, it is considered multibacillary for administration of multidrug therapy. When skin lesions start appearing in due course in some pure neuritic leprosy, change in the type of multidrug therapy may need to be considered.
Silent neuropathy needs to be treated with tapering doses of corticosteroids over months. In cases of overt neuritis, principles of treatment and corticosteroid dosage should be similar to those recommended for management of neuritis of type 1 lepra reaction.
Neuropathic pain in pure neuritic leprosy should be managed with tricyclic antidepressants and anticonvulsants.
What is the prognosis of pure neuritic leprosy?
Pure neuritic leprosy can lead to residual sensory, motor or autonomic nerve impairment. There can be development of skin lesions and progression of disease most commonly to borderline tuberculoid leprosy. Nerve thickening tends to persist for years.
Paraneoplastic Palmoplantar Keratoderma
What are the causes of acquired palmoplantar keratoderma?
Hypothyroidism, malnutrition, drugs, infections and infestations, papulosquamous disorders, eczema, aquagenic keratoderma and keratoderma climactericum are broadly the causes of acquired palmoplantar keratoderma.
When should one suspect underlying malignancy in palmoplantar keratoderma?
When there is a sudden onset of palmoplantar keratoderma in the absence of other findings, one should raise the suspicion of an underlying malignancy.
What is Bazex syndrome?
Bazex syndrome, also called acrokeratosis paraneoplastica, is an acquired palmoplantar keratoderma occurring in men more than 40 years of age, associated with neoplasia of the upper aerodigestive tract. There are three stages of this disorder. The eruption starts as erythema with psoriasiform scaling on the fingers and toes which spreads to the ear helices and nasal bridge leading to violaceous erythema and pityriasiform scaling. Next, the eruption spreads to palms and soles producing keratoderma with a violaceous color and giving the skin an edematous appearance with a honeycomb pattern. Finally, if the neoplasm has not been treated, the rash extends to the legs, knees, thighs, arms and scalp.
What are tripe palms?
It is a distinctive form of palmar keratoderma with a thickened moss-like or velvety structure characterized by exaggerated dermatoglyphics of the palmar surface of hands and fingers. These findings are thought to resemble the lining of cow stomach called “tripe.” Tripe palms can be noted with or without acanthosis nigricans. Lung and stomach malignancies are most commonly associated.
What is Howel–Evans syndrome?
This is a hereditary diffuse hyperkeratosis of palms and soles, described by Howel–Evans et al. as “tylosis” and is associated with esophageal carcinoma.
Phacomatosis Pigmentovascularis
What is phacomatosis pigmentovascularis?
Phacomatosis pigmentovascularis is a rare group of syndromes characterized by the coexistence of a vascular nevus and a pigmentary nevus with or without extracutaneous systemic involvement.
Enumerate the classification systems and salient clinical findings in various types of phacomatosis pigmentovascularis
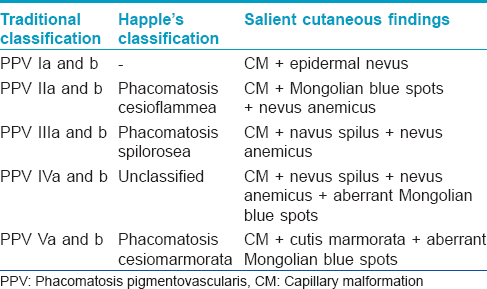
Hasegawa and Yasuhara in 1985 classified phacomatosis pigmentovascularis into four types based on the pigmentary nevus component. A fifth type was added to this traditional classification later. Phacomatosis pigmentovascularis has two subtypes (a) and (b): (a) having only cutaneous signs (b) with extracutaneous manifestations (systemic/syndromic form).
Happle in 2005 reclassified phacomatosis pigmentovascularis as three major types: (1) phacomatosis cesioflammea, (2) phacomatosis spilorosea and (3) phacomatosis cesiomarmorata.
The classification systems and salient clinical findings in various types of phacomatosis pigmentovascularis are described in [Table - 3].
What are the therapeutic and prognostic implications in phacomatosis pigmentovascularis?
Treatment and prognosis of phacomatosis pigmentovascularis depend on the organ systems affected. For cutaneous lesions, a combined laser including Q-switched alexandrite laser for pigmented lesions and pulsed-dye laser for vascular lesions seems to be appropriate. Since most cases arise sporadically without any risk in subsequent pregnancies, prenatal screening is not necessary and this helps in reassuring the patients/parents during genetic counseling.
Glutathione
What is the biological relevance of glutathione redox cycle?
Glutathione exists in two interconvertible forms, reduced glutathione and oxidized glutathione (glutathione disulfide). Glutathione is the predominant intracellular form which acts as a strong antioxidant and defends against toxic compounds and xenobiotics. In the redox cycle process, glutathione is constantly oxidized to glutathione disulfide by the enzyme glutathione peroxidase. To maintain the intracellular redox balance, glutathione is replenished through the reduction of glutathione disulfide by glutathione reductase enzyme.
What are the various mechanisms for the skin-lightening effect of glutathione?
The skin-lightening effects are due to the following mechanisms:
- Direct inactivation of tyrosinase by binding with the copper-containing active site of the enzyme
- Indirect inactivation of tyrosinase via antioxidant effect
- Switching production of eumelanin to pheomelanin
- Modulation of the depigmenting abilities of other melanocytotoxic agents.
What are the various pharmaceutical formulations of glutathione?
Glutathione is primarily available as oral formulations (pills, solutions, sublingual tablets, syrups and sprays) and parenteral formulations (intravenous and intramuscular). It has been administered by intranasal and intrabronchial routes as well.
What are routes of administration of glutathione for skin lightening and the evidence for its role in skin lightening?
The three major routes of administration used for skin lightening are topical, oral and intravenous injections.
Topical: Therapy with creams, face washes, peels and mesotherapy have been used as monotherapy or as combination therapy.
Oral: Formulations include capsules and sublingual/buccal tablets. The recommended oral dose is 20–40 mg/kg body weight/day (1–2 g glutathione/day) divided into two doses. The duration of the visible skin-lightening effect may vary from 1 month to 2 years and a maintenance dose of 500 mg/day for an indefinite duration may be needed.
Intravenous: Manufacturers of intravenous glutathione injections recommend a dose of 600–1200 mg to be injected once to twice weekly. The duration for which they should be continued is not specified. Side effects of intravenous glutathione include adverse cutaneous eruptions ranging from skin rashes to serious and potentially fatal Stevens–Johnson Syndrome and toxic epidermal necrolysis, thyroid dysfunction, renal dysfunction, severe abdominal pain and reactions due to faulty technique or inappropriate formulation.
There are no published data for intravenous glutathione and only three randomized controlled trials with short-term follow-up have so far provided evidence in favor of the skin-lightening effects of topical and oral glutathione with no significant adverse effect. The role of glutathione in specific disorders of hyperpigmentation also needs to be elucidated.
Ustekinumab in Psoriasis
Which are the biological agents used for treatment of psoriasis?
The various biological agents and their mechanism of action are as follows:
- Etanercept, infliximab, adalimumab: tumor necrosis factor alpha inhibitors
- Ustekinumab: interleukin-12/23 inhibitor
- Secukinumab: interleukin-17 inhibitor
- Itolizumab: anti-CD6 antibody.
How does ustekinumab reactivate hepatitis B virus infection?
Ustekinumab is a human monoclonal antibody against interleukin 12/23. Several mechanisms have been proposed for reactivation of hepatitis B virus in patients treated with ustekinumab.
Interleukin-12 inhibition prevents the differentiation of T helper cells, the activation of CD8 cytotoxic T cells and the production of interferon resulting in intracellular replication of the residual hepatitis B virus. Interleukin-23 inhibition suppresses the differentiation of Th17 cells affecting the ability of B cells to proliferate and produce anti-hepatitis B surface antibodies. Further, interleukin-12 inhibition also leads to an increase in the levels of regulatory T cells which may adversely affect the production of antibodies. Antigen-presenting cells, nitric oxide and transforming growth factor are also involved in the onset of hepatitis B infection.
Becker's Naevus
Describe classical and atypical presentations of Becker's nevus
Becker's nevus is characterized by a well-defined hyperpigmented patch with irregular margins and associated hypertrichosis usually on the upper half of trunk and upper extremities and is commonly seen in adolescent males. The most common sites are the shoulder, anterior chest or scapular region but lesions on the face, neck and distal limbs have been reported. Atypical presentation of Becker's nevus can be related to onset (congenital or late), family history, rare sites of distribution such as legs, presence of multiple lesions, bilateral distribution or a dermatomal or blaschkoid pattern of involvement.
What is the pathogenesis of Becker's nevus?
The exact pathogenesis of Becker's nevus is unknown. Various postulated mechanisms include
- Mosaicism, wherein the lesions follow a blaschkoid, checkerboard or phylloid pattern or a patch without midline separation
- Somatic mutation, where the abnormal phenotype expression occurs only in the affected segments of the body resulting in a linear or block-like configuration
- Androgen stimulation as evidenced by its peripubertal development, male preponderance, hypertrichosis, acneiform lesions within the patch and increase in androgen receptors in involved skin.
What is the histopathological feature of Becker's nevus?
Histopathology shows acanthosis, broad and fused adjacent rete ridges, variable hyperkeratosis and basal layer hyperpigmentation with associated dermal smooth muscle hyperplasia in some cases.
What is Becker's nevus syndrome?
Becker nevus syndrome includes association of Becker's nevus with one or more of the following: unilateral hypoplasia of the breast, aplasia of the ipsilateral pectoralis major muscle, ipsilateral limb shortening, localized lipoatrophy, spina bifida, scoliosis, pectus carinatum, congenital adrenal hyperplasia and an accessory scrotum.
What are the treatment options for Becker's nevus?
Treatment includes Q-switched or long pulsed ruby or neodymium-doped yttrium aluminum garnet laser or erbium-doped yttrium aluminum garnet laser for hyperpigmentation and hypertrichosis; however, response rates are poor. Cosmetic camouflage may be helpful.
Immunotherapy in Warts
What are the various immunotherapeutic approaches in treatment of warts?
Various immunotherapeutic approaches have been attempted using topical contact sensitizers, oral immunomodulators, interferons and various viral, fungal and bacterial antigens which are administered intralesionally or intradermally. Intralesional therapy with Candida and Trichophyton skin test antigens, Mycobacterium indicus pranii vaccine, and mumps, measles and rubella vaccine have been tried.
What is the mechanism of action of immunotherapeutic agents in warts?
The basis of immunotherapy is the manipulation of the immune system to achieve a human papilloma virus-targeted immune reaction. Various immunotherapeutic interventions influence the release of different cytokines such as interleukin-2, interleukin-4, interleukin-5, interleukin-8, interferon and tumor necrosis factor alpha that stimulate a strong immune response against human papillomavirus. Antigen injections are also associated with the proliferation of peripheral blood mononuclear cells; these promote Th1 cytokine responses and further activate cytotoxic T-cells and natural killer cells to eradicate human papillomavirus-infected cells.
Drug Reaction With Eosinophilia and Systemic Symptom
What is drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome and its synonyms?
Drug reaction with eosinophilia and systemic symptoms syndrome is a severe and potentially life-threatening disease presenting with skin rash, eosinophilia and systemic involvement occurring 1–8 weeks after drug introduction.
It is also known as drug hypersensitivity syndrome or as drug-induced delayed multiorgan hypersensitivity syndrome or anticonvulsant hypersensitivity syndrome.
Which are the commonly implicated drugs in DRESS?
The most frequently implicated drugs are anticonvulsants (phenytoin, carbamazepine, phenobarbital and lamotrigine), sulfonamides, minocycline, procarbazine, allopurinol, terbinafine, dapsone, abacavir, nevirapine and rarely calcium channel blockers. The pathophysiological pathways may be multifactorial involving immunological mechanisms, particularly drug detoxification pathways and sequential reactivation of viral infections.
Describe the clinical manifestations and treatment of DRESS
The clinical characteristics include fever, facial edema with infiltrated papules and generalized morbilliform or papulo-pustular rash or exfoliative dermatitis. Lymphadenopathy and hematological abnormalities such as hypereosinophilia or atypical lymphocytes may be seen. Organ involvement includes hepatitis, nephritis, pneumonitis, myocarditis, encephalitis and hypothyroidism. Systemic corticosteroids tapered gradually are the mainstay of treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Fulltext Views
7,085
PDF downloads
2,158





