Translate this page into:
Viva questions from the IJDVL
2 Department of Dermatology, K J Somaiya Medical College and Research Centre, Mumbai, Maharashtra, India
Correspondence Address:
Vishalakshi Viswanath
Department of Dermatology, Rajiv Gandhi Medical College, Thane, Maharashtra
India
| How to cite this article: Viswanath V, Vasani R. Viva questions from the IJDVL. Indian J Dermatol Venereol Leprol 2016;82:745-751 |
Focus Topic - keloid
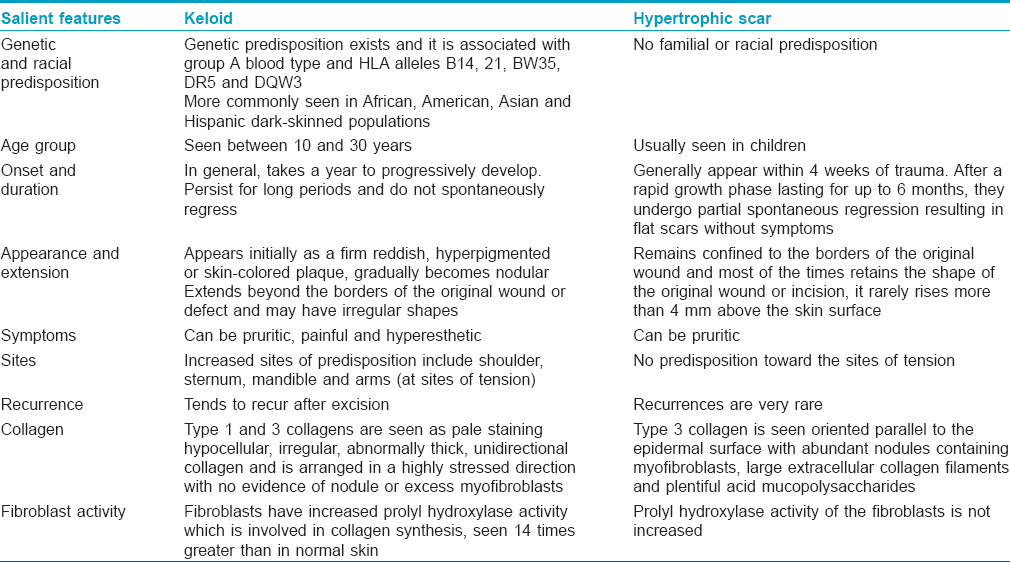
What are the differences between a keloid and hypertrophic scar?
The differences between keloid and hypertrophic scar have been outlined in [Table - 1].
What are the syndromes associated with the tendency to develop keloids?
- Rubinstein–Taybi syndrome
- Goeminne syndrome
- Ehler–Danlos syndrome
- Dubois syndrome
- Pachydermoperiostosis
- Progeria
- Osteopoikilosis.
What are the risk factors for keloid formation?
The risk factors for keloid formation include the following:
- African, American, Asian or Hispanic ethnicity
- Family history of keloidal tendency
- In darkly pigmented skin, risk increases by 15–20 fold
- Wound healing by secondary intention
- Prolonged healing time >3 weeks
- Wounds subjected to prolonged inflammation whether foreign body related/infection/burn/inadequate wound closure
- Chronic inflammation: earring site, sites of repeated trauma
- Wounds on anterior chest, shoulders, flexor surfaces of extremities, anterior neck and wounds that cross the skin tension lines are more susceptible to abnormal scar formation
- Deep wounds like those from burns or surgical scars
- Scars from acne, vaccination or chicken pox.
What are the preventive measures that can be taken in cases with a keloidal tendency?
The preventive measures which can be undertaken in persons who are prone to develop keloids include the following:
- Withhold non-essential cosmetic surgery/piercing
- Closing all wounds with minimal tension by making incision along Langer's lines
- Use of pressure garments up to 4–6 months post-injury
- During surgeries, aim for primary closure, adequate debridement of contaminated wounds good homeostasis and gentle handling of tissues.
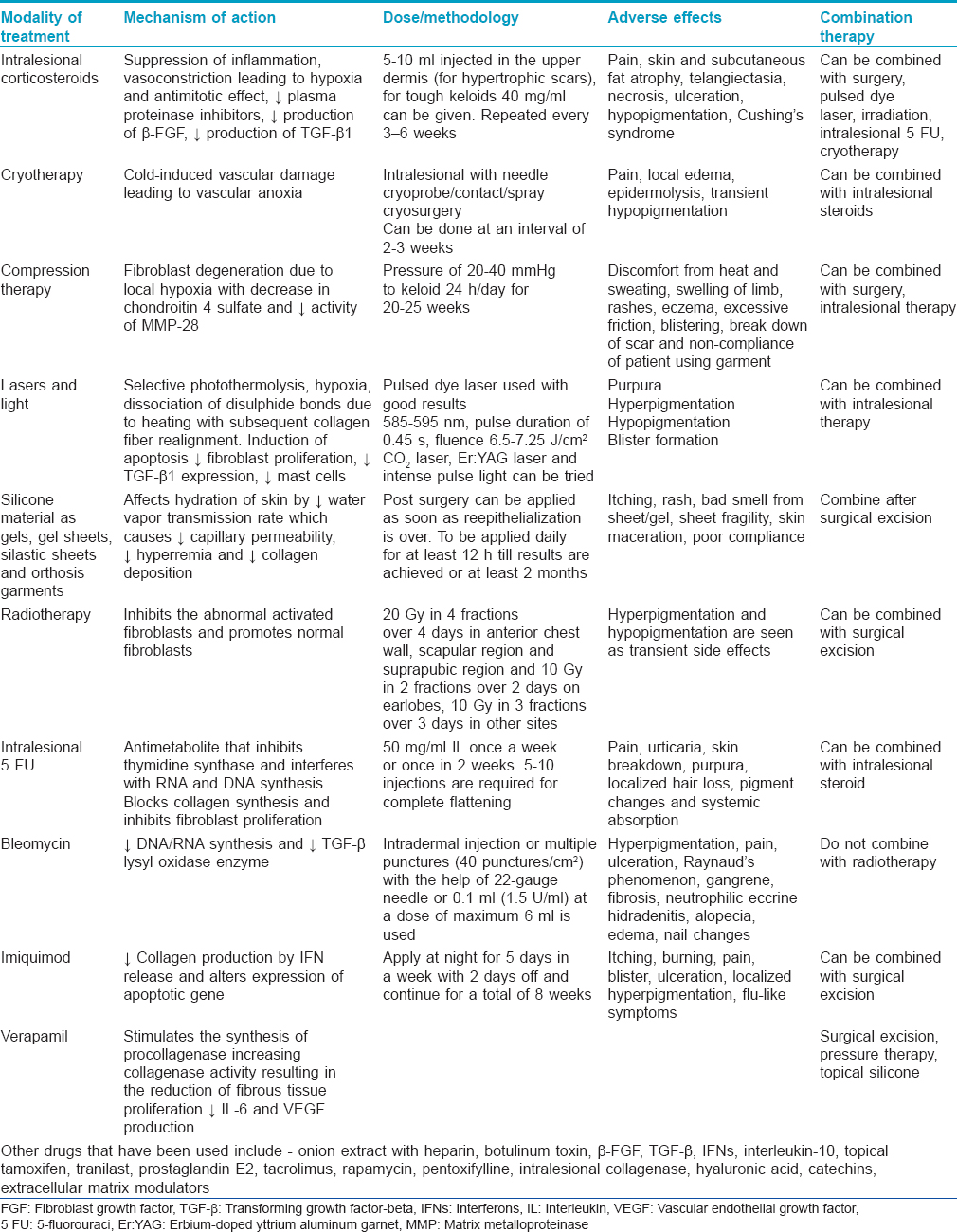
What are the treatment modalities for keloids?
The treatment modalities for keloids have been outlined in [Table - 2].
Dermal Melanocytosis
What is dermal melanocytosis?
Dermal melanocytosis or dermal dendritic melanocytic proliferations are characterized by the presence of melanin-producing dendritic melanocytes in the dermis. Clinically, speckled or mottled, gray or blue-gray appearance is distinctive in dermal melanocytosis which is caused by Tyndall effect.
Enumerate the various types of dermal melanocytosis
Dermal melanocytosis can be of congenital and acquired types. Most cases present at birth or may manifest clinically in early childhood. Nevus of Ota, nevus of Ito, Mongolian spot and dermal melanocytic hamartoma are congenital dermal melanocytosis. Acquired dermal melanocytoses appear in adult life which has been reported very rarely and consist of nevus of Hori (acquired bilateral nevus of Ota), nevus of Sun (acquired unilateral nevus of Ota) and a rare entity, extra-facial acquired dermal melanocytosis.
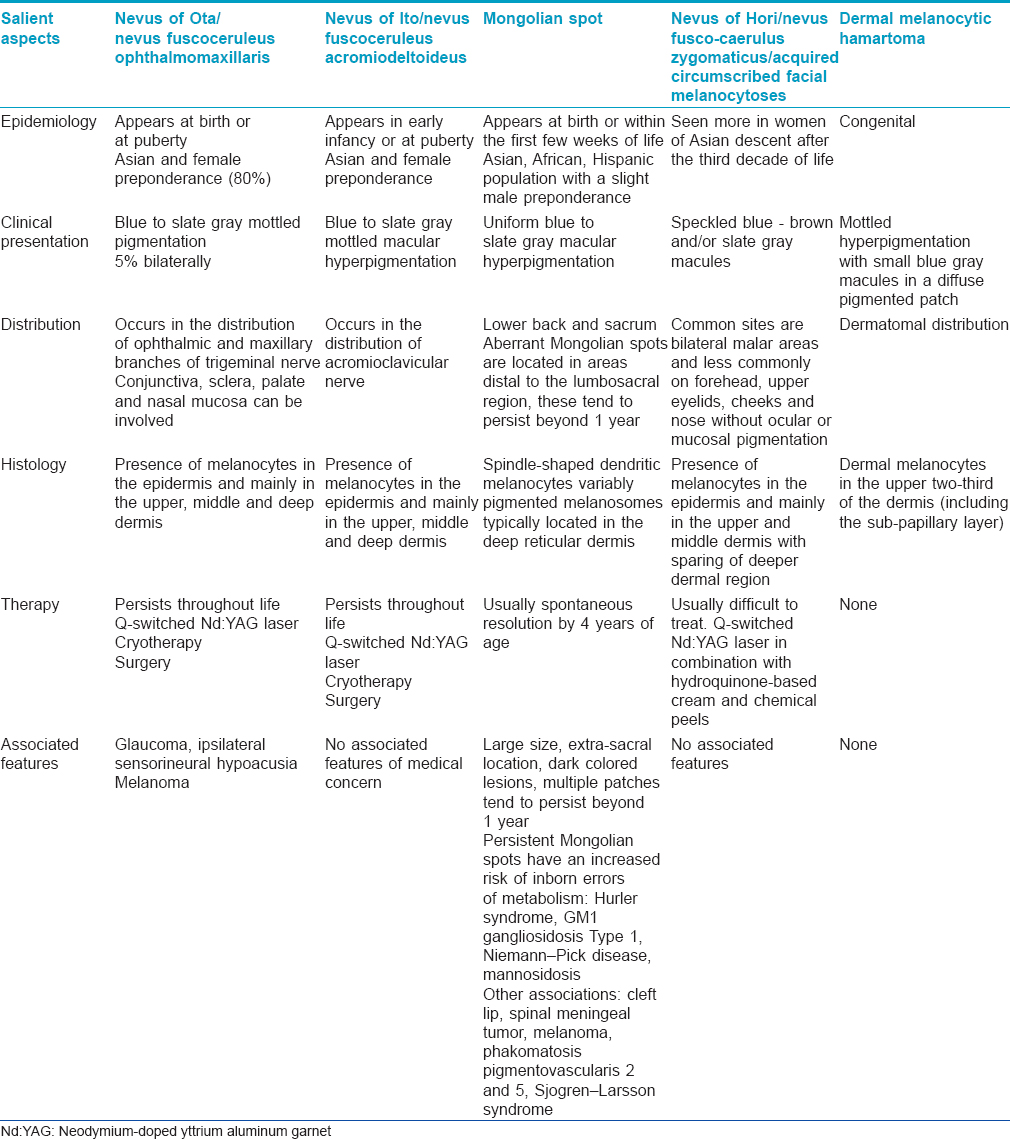
Enumerate the salient aspects which help to differentiate the various dermal melanocytosis?
The differentiating features of dermal melanocytosis have been outlined in [Table - 3].
Nevoid Hyperkeratosis of Nipple and Areola
What is nevoid hyperkeratosis of the nipple and areola?
Hyperkeratosis of the nipple and/or areola is defined as excessive keratinization of the nipple and/or areola. It includes hyperpigmentation, verrucous and filiform keratotic thickening of the nipple and areola with papillomatosis and a velvety sensation to touch.
How is nevoid hyperkeratosis of the nipple and areola classified?
Nevoid hyperkeratosis of the nipple and areola has been classified as follows:
- Type 1: Occurs as an extension of epidermal nevus
- Type 2: Hyperkeratosis of the nipple associated with other dermatoses such as atopic disease, acanthosis nigricans, Darier's, seborrheic keratosis and Bowen's disease
- Type 3: No association with epidermal nevus or other dermatoses.
Alternately, it is classified into primary hyperkeratosis of nipple and/or areola which is idiopathic and secondary hyperkeratosis of the nipple and/or areola which is associated with the above-mentioned disorders.
What is the management of a case of nevoid hyperkeratosis?
Unilateral primary hyperkeratosis of the nipple and/or areola must be distinguished from an underlying breast carcinoma. Pain, bleeding, ulceration, nipple discharge or loss of normal anatomy with nipple retraction or loss of nipple should prompt immediate evaluation. Lesions recalcitrant to therapy also warrant investigation. The evaluation of these lesions should include complete bilateral breast examination with evaluation of the lymph nodes, mammography and biopsy of the involved skin.
Biopsy in a classical case of primary hyperkeratosis shows orthokeratotic hyperkeratosis, acanthosis, papillomatosis with mild dermal lymphocytic perivascular inflammation and epidermal spongiosis with microabscesses containing normal lymphocytes. In secondary hyperkeratosis, the histologic findings are related to the underlying associated skin disease.
Treatments that have been previously reported include topical lactic acid (12%), topical salicylic acid 6%, tretinoin, calcipotriol, cryotherapy, low-dose isotretinoin, shave excision, CO2 laser ablation, surgical excision with reconstruction and curettage.
Anticoagulants in Dermatology
Classify anticoagulants and enumerate the therapeutic applications in dermatology
Anticoagulants have been broadly categorized into heparins, vitamin K antagonists and direct inhibitors of thrombin and factor Xa. These can be administered orally or parenterally.
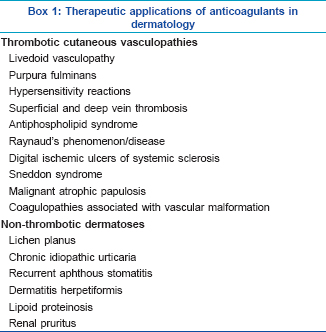
The therapeutic applications of anticoagulants in dermatology have been outlined in [Box 1].
Describe the dermatological adverse effects of anticoagulants?
The dermatological adverse effects of anticoagulants and their clinical manifestations include the following:
Warfarin-induced skin necrosis
It manifests as sudden onset pain which is followed by the development of well-demarcated erythema that evolves to hemorrhagic bullae, necrosis and eschar formation. Areas with abundant fat such as the breasts, abdomen, hips and buttocks are predominantly involved.
Heparin-induced thrombocytopenia
It commonly begins 5–15 days after heparin administration. Cutaneous microvascular involvement manifests as a well-demarcated, tender, purpuric rash with a characteristic retiform configuration and minimal erythema/inflammation. These may occur at the site of subcutaneous injection or at distant sites when heparin is infused intravenously and may progress to cutaneous necrosis and eschar formation.
Anticoagulant-associated cholesterol embolization syndrome
It occurs 4–8 weeks after anticoagulation therapy in patients with an underlying asymptomatic or severe atheromatous disease. Cutaneous findings include livedo reticularis (most frequent), acrocyanosis (blue/purple toe syndrome) or acral gangrene with preserved peripheral pulses. Other manifestations include nodules, infiltrated plaques and purpura.
Other cutaneous adverse reactions
Various cutaneous reactions may be observed at the injection site of heparins such as purpura, ecchymoses, necrosis and infiltrated plaques. Calcinosis cutis, hypersensitivity reactions such as urticaria, angioedema and Baboon syndrome and patch test positivity can occur. Telogen effluvium and nail changes such as reduced growth, transverse bands and subungal hematomas have also been reported.
Pagetoid Bowen's Disease Versus Extramammary Paget's Disease
Enumerate the clinical differential diagnoses for Pagetoid Bowen's disease
Pagetoid Bowen's disease is a vulvar intraepithelial neoplasia and it is a histological variant of Bowen's disease which simulates the pattern of Paget's disease.
Pagetoid Bowen's disease is commonly confused with extramammary Paget's disease both clinically and histologically. It can also mimic other common conditions such as eczema, intertrigo, pruritus vulvae, erosive lichen planus and seborrhoeic dermatitis.
Which are the sites of involvement for extramammary Paget's disease?
Vulva is the most common area involved in extramammary Paget's disease. This is followed by the perianal area which is more frequently affected in men than women. Other sites of involvement include the scrotum, penis, eyelids, ears and axilla.
Describe the histological and immunohistochemistry features which differentiate pagetoid Bowen's disease from extramammary Paget's disease
Histologically, extramammary Paget's disease is characterized by a collection of large cells with abundant pale cytoplasm and atypical round-to-oval nuclei (Paget's cell) and these are sharply demarcated from the surrounding keratinocytes. These cells can be arranged in nests and are located primarily within the lower levels of the epidermis and often demonstrate extension into cutaneous adnexal structures.
Histologically, pagetoid Bowen's disease demonstrates either single or groups of atypical keratinocytes which are present at all levels of the epidermis. Additional histological features include intercellular bridges between nested pagetoid cells, atypical cells and multinucleated cells between the nests of cells.
Immunohistochemistry markers
- p63 is a useful immunohistochemistry marker for the differentiation of pagetoid Bowen's disease and extramammary Paget's disease; it shows a strong positivity in pagetoid Bowen's disease
- Syndecan-1 immunoreactivity is seen on the cell membrane in pagetoid Bowen's disease whereas in extramammary Paget's disease, cytoplasmic syndecan-1 immunoreactivity is seen
- CAM 5.2, carcinoembryonic antigen, gross cystic disease fluid protein 15 and c-erb B2 staining are strongly positive in extramammary Paget's disease and negative in pagetoid Bowen's disease
- Overlap between pagetoid Bowen's disease and extramammary Paget's disease is seen for the following markers: cytokeratin 5/6/7/19 and keratin 903.
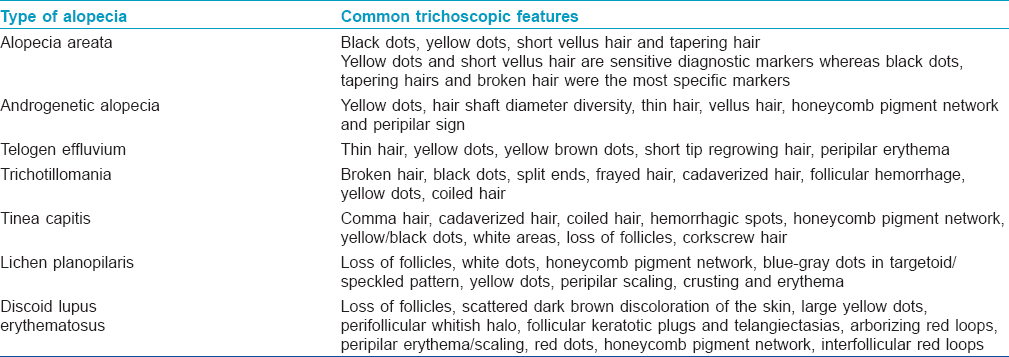
Trichoscopy in Alopecia
Describe the various trichoscopic patterns in different types of alopecia
The various trichoscopic patterns have been described in [Table - 4].
Patch Testing in Hair Dyes
Which is the most important allergen in hair dyes?
Para-phenylenediamine is one of the most important antigens responsible for allergic contact dermatitis to hair dye. It is an effective dye ingredient that, when mixed with other ingredients, enables black or other color dyes to dye hair permanently.
What are the ingredients in permanent hair dyes?
The common ingredients include para-phenylenediamine, aminophenols, henna, toluene-2,5-diamine sulfate, pyrogallol, resorcinol, ferrous sulfate, oxidizers such as hydrogen peroxide and sodium perborate and other ingredients such as tartaric acid, glycerin, naphthol and cresols.
Which are the chemicals which can cross react with para-phenylenediamine?
Hair dye intermediate chemicals such as aminophenols and toluene-2,5-diamine sulfate can cross react with para-phenylenediamine.
Why does a patient experience an allergic reaction despite using hypoallergenic hair dye products?
Although many hair dye products available in the market are advertised as hypoallergenic, para-phenylenediamine-free, non-allergenic or herbal, they may contain either small amounts of para-phenylenediamine or other substances that cross react with para-phenylenediamine. Hence, allergic reactions can occur in a significant number of patients despite claimed safety. Patients with hair dye contact dermatitis must always choose their hair dye by checking the contents and undergoing sensitivity testing.
Scleromyxedema
What are the types of lichen myxedematous?
Lichen myxedematosus is a form of idiopathic cutaneous mucinosis occurring in the absence of thyroid disease and characterized by abnormal dermal mucin deposition and fibrosis. The two types are a generalized papular and sclerodermoid form (scleromyxedema of Arndt–Gottron) with a monoclonal gammopathy and systemic manifestations and a localized papular form without systemic features.
Enumerate the salient clinical features and differential diagnosis in scleromyxedema
Scleromyxedema is characterized by widespread eruption of small, waxy papules on the upper limbs, thighs, trunk and head and neck region; the papules may be arranged in a linear pattern. There may be a diffuse sclerodermoid or hardened skin giving rise to leonine facies. The differential diagnosis includes systemic sclerosis, scleredema and nephrogenic systemic fibrosis.
What is the characteristic histological feature in scleromyxedema?
The characteristic feature is deposition of mucinous material (Alcian blue positive) between thick collagen bundles and abundant proliferation of fibroblasts in the upper and mid-reticular dermis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Fulltext Views
9,711
PDF downloads
3,822





