Translate this page into:
Warty mucosal lesions: Oral condyloma lata of secondary syphilis
2 Department of Dermatology, The Second Xiangya Hospital, Central South University, Changsha, Hunan 410011, China
Correspondence Address:
Hai Long
Department of Dermatology, The Second Xiangya Hospital, Central South University, 139 Middle Renmin Road, Changsha, Hunan 410011
China
| How to cite this article: Liu Z, Wang L, Zhang G, Long H. Warty mucosal lesions: Oral condyloma lata of secondary syphilis. Indian J Dermatol Venereol Leprol 2017;83:277 |
Sir,
We would like to report a 24-year-old Chinese man who presented with a four month history of painless, greyish-white oral lesions [Figure 1a]. It began as a single, approximately 2 mm, papular lesion over the center of the palate, and gradually increased in size. The patient paid no special attention to it until the last fifteen days, when he felt a foreign body sensation while swallowing food. He noticed several additional lesions on both sides of the soft palate. He was afebrile and in good health. He reported multiple episodes of unprotected receptive oral sex with a male partner in the last six months before the onset of the lesions but no history of oral ulceration or skin rash.
 |
| Figure 1a: Oral condyloma lata. Well-demarcated, greyish-white mucosal plaques on the palate |
Physical examination revealed three groups of well demarcated, broad, lobulated, greyish-white, verrucous plaques on the soft palate, and a smaller plaque measuring 12 mm × 10 mm at the center of the palate [Figure 1a]. There was no tenderness. There were no other oral or skin lesions. There was no hair loss or lymphadenopathy. The systemic examination was within normal limits. Laboratory test results showed a white cell count of 10,170/mm [3] with 68.7% neutrophils. Gram stained smears and a potassium hydroxide mount from the oral lesions were negative. Testing for human papilloma virus was negative by visual inspection with acetic acid and polymerase chain reaction analysis. The rapid plasma reagin test was positive (titer, 1:8), as was the treponema pallidum particle agglutination assay. A serologic test for human immunodeficiency virus infection was negative.
On the basis of clinical and laboratory findings, secondary syphilis with oral condyloma lata was diagnosed. We treated the patient with intramuscular benzathine penicillin G, 2.4 million units, once weekly, for three weeks.[1] The lesions disappeared within two weeks of treatment [Figure 1b]. The rapid plasma reagin test showed a titer of 1:1 three months later. The patient was advised to have this checked again at six months and one year after treatment.
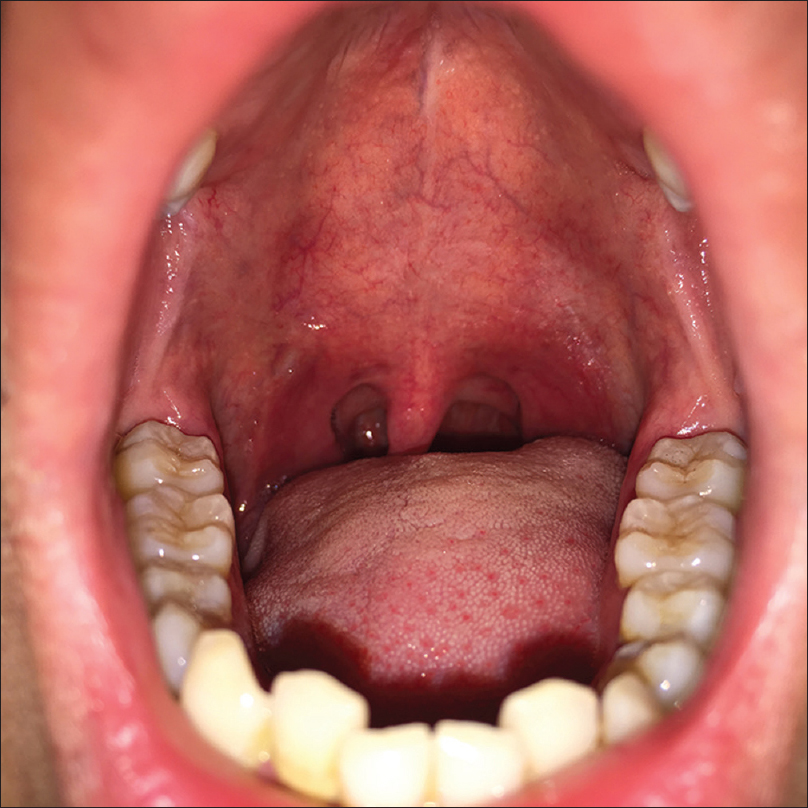 |
| Figure 1b: Oral condyloma lata. Resolution after two weeks of treatment |
Condyloma lata is one of the characteristic mucosal signs of secondary syphilis. Lesions in the oral cavity are rarely reported. Typically, they are grey or white, moist, verrucous papules or plaques commonly located in the anogenital area. However, they occasionally occur at atypical locations which are warm, moist or intertriginous, such as the umbilicus, axilla, inframammary folds and toe web spaces. Condyloma lata in the oral cavity is extremely rare, and we were able to find only one previous report in English.[2] The clinical photographs of two recent reports with oral warty plaques due to secondary syphilis were highly indicative of oral condyloma lata, although the authors did not specifically use this term.[3],[4] Differential diagnoses for these warty oral masses include condyloma accuminata, oral lichen planus, oral leukoplakia, Bowen's disease, squamous cell carcinoma and oral candidiasis.
Syphilis has had a worldwide resurgence and remains a challenging public health problem. It can be treated easily if recognized early. The challenge lies in recognizing important diagnostic clues, including the characteristic skin rashes and mucosal lesions. Oral mucous patches, leukoplakia-like plaques, maculopapular or ulcerative lesions are commonly seen in secondary syphilis.[5] However, solitary oral involvement such as in our case is rare, and can lead to misdiagnosis. A high index of suspicion of syphilis must be maintained when evaluating oral lesions, especially with a history of unprotected sexual contact.
Acknowledgment
We thank Dr. Yaping Li from the Department of Dermatology, The Second Xiangya Hospital of Central South University for helpful discussion of the case. We also thank the patient for providing permission to publish his information.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Wang Q, Zhang G, editors. Guidelines for Diagnosis and Treatment of Sexually Transmitted Diseases. Shanghai: Shanghai Scientific and Technical Publishers; 2007.
[Google Scholar]
|
| 2. |
de Swaan B, Tjiam KH, Vuzevski VD, Van Joost T, Stolz E. Solitary oral condylomata lata in a patient with secondary syphilis. Sex Transm Dis 1985;12:238-40.
[Google Scholar]
|
| 3. |
Ulmer A, Fierlbeck G. Images in clinical medicine. Oral manifestations of secondary syphilis. N Engl J Med 2002;347:1677.
[Google Scholar]
|
| 4. |
Ramírez-Amador V, Anaya-Saavedra G, Crabtree-Ramírez B, Esquivel-Pedraza L, Saeb-Lima M, Sierra-Madero J. Clinical spectrum of oral secondary syphilis in HIV-infected patients. J Sex Transm Dis 2013;2013:892427.
[Google Scholar]
|
| 5. |
Swanson J, Welch J. The great imitator strikes again: Syphilis presenting as “tongue changing colors”. Case Rep Emerg Med 2016;2016:1607583.
[Google Scholar]
|
Fulltext Views
11,821
PDF downloads
2,744





