Translate this page into:
When the eye does not see, the bone can grieve: An unusual presentation of secondary syphilis
2 Department of Clinical and Experimental Medicine, Unit of Infectious Disease, University of Messina, Messina, Italy
3 Department of Human Pathology of Adult and Developmental Age “Gaetano Barresi”, University of Messina, Messina, Italy
4 Department of Biomedical, Dental Sciences and Morphological and Functional Images, Eye Clinic, University of Messina, Messina, Italy
Correspondence Address:
Mario Vaccaro
Via C. Valeria, Gazzi. 98125 Messina
Italy
| How to cite this article: Vaccaro M, Marafioti I, Nunnari G, Pellican� GF, Vaccaro F, Trombetta CJ, Cannav� SP. When the eye does not see, the bone can grieve: An unusual presentation of secondary syphilis. Indian J Dermatol Venereol Leprol 2020;86:184-186 |
Sir,
We would like to report the case of a man with skin lesions of uncertain diagnosis that impressed us with its peculiar presentation and for the diagnostic illusions it caused.
A 56-year-old man was referred to our dermatology department for evaluation of skin lesions which had been previously diagnosed as chronic eczema and palmoplantar psoriasis by another dermatologist. He was applying an ultra-high-potency corticosteroid ointment for the same and since one month, was also taking cyclosporine tablets, without any result. For about 6 months prior to this, the patient had been experiencing photophobia, blurred vision and excessive tearing that affected only his left eye. He was diagnosed with pan-uveitis [Figure - 1] and was on treatment with systemic corticosteroids and peribulbar injections of triamcinolone acetonide. He also complained of a chronic and dull articular pain affecting the lower limbs (hips, knees, and ankles), which was occasionally treated with non-steroidal anti-inflammatory drugs with poor improvement. He was sent to our department for a dermatological evaluation to detect any possible correlation between the cutaneous lesions and the aforesaid symptoms.
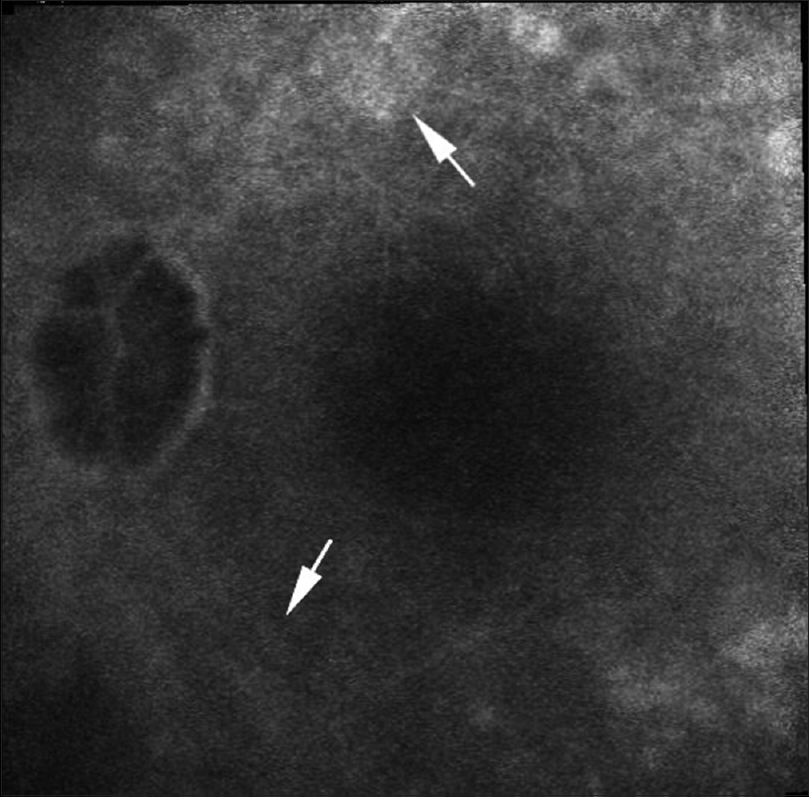 |
| Figure 1: Fluorangiography showed panuveitis - presence of diffuse hypofluorescent areas due to screen effect and presence of vitreous and retinal exudation, increased vascular permeability due to barrier break and areas of atrophy |
Our physical examination revealed symmetrically distributed erythematous, desquamative lesions on both palms [Figure - 2]a and marked (sometimes roundish and circinate) hyperkeratosis [Figure - 2]b with rhagadiform aspects on the plantar regions. Itching was inconstant. Simultaneous involvement of eye and joints led us to consider Behçet's disease, but the patient did not report any apthous or herpetiform ulcers affecting mouth or genital region, which are the main diagnostic criterion for this condition.[2]
 |
| Figure 2: (a) Erythematous desquamative lesions on both palms. (b) Marked hyperkeratosis resembling fissures on the plantar regions |
The other most important differential diagnosis that we considered was blenorragic keratoderma associated with reactive arthritis, which, similar to psoriasis, may be characterized by palmoplantar hyperkeratosis and polymorphic skin lesions (papules, vesicles, pustules and crusts) as well as onycholysis and perionyxis. As the patient did not give history of gastrointestinal or genitourinary infections and the serological and microbiological examination on urethral swab for Chlamydia, Ureaplasma, Neisseria, Salmonella, and Shigella was negative, we ruled out reactive arthritis.
At this point, as the circular hyperkeratosis on the plantar area could be attributable to Biett's collarette typical of syphilis, we considered the differential diagnosis of syphilis. The patient did not recall ulcerations on oral and anogenital area or other body sites (suggestive of primary syphilis) in previous months, but he reported multiple episodes of unprotected sexual contact. We performed Treponema pallidum serology that showed positive VDRL 1:512 titre and TPHA 1:1024 titre, high titers of anti-cardiolipin IgG and IgM, and anti-T. pallidum IgG (>48; index negative for <9 – positive for >11), while IgM was normal (6; index negative for <9 – positive for >11). This made us diagnose the case as secondary syphilis. Panuveitis was an important extracutaneous manifestation of this stage of disease.[3]
A magnetic resonance imaging of the most affected joints showed bone edema and periosteal reaction with periarticular tissue involvement [Figure - 3], compatible with luetic (syphilitic) arthropathy.
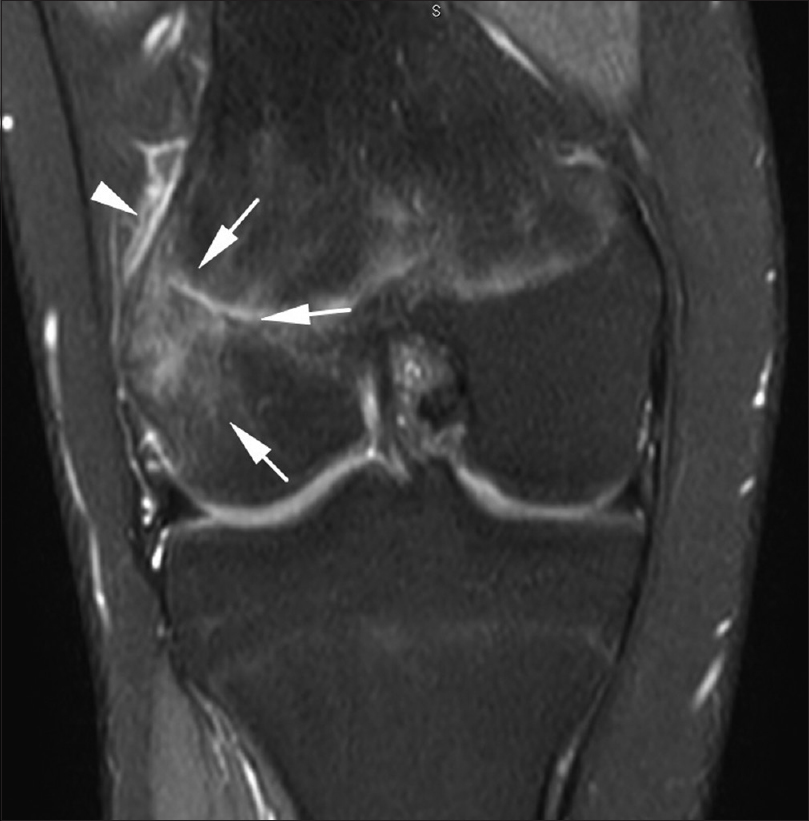 |
| Figure 3: Magnetic resonance imaging of the knee showed bone edema (arrows) and periosteal reaction (arrow tip) with involvement of periarticular tissues |
Luetic arthropathy was first described in 1886, but radiographic alterations in early acquired syphilis were noted in 1932. Although articular pain could be misinterpreted as an additional illness, luetic etiology was confirmed by several authors, mainly during the tertiary stage. It is possible (although unusual) also in secondary syphilis, frequently affecting limb and skull (especially frontal bone), causing headache. Histological examination of bone and surrounding tissues often reveals plasma cells and lymphocytic infiltrate, while presence of spirochetes are uncommon.[4]
Eye involvement in secondary syphilis suggests that the infection may be progressing toward tertiary stage. For this reason, we performed a lumbar puncture to analyze cerebrospinal fluid (CSF). CSF examination did not reveal either cellular or protein abnormalities, and both VDRL and TPHA were negative. Nevertheless, as ocular involvement justifies the use of the therapeutic scheme of tertiary syphilis, even in the treatment of secondary stage, the patient was given intramuscular benzathine benzylpenicillin 2.4 million units once a week for 3 consecutive weeks.[5]
During the follow-up period, for overall patient's safety, we also performed HIV serology that was negative.
After 6 months, the patient experienced complete healing and we could observe reduction in arthralgias, only partial improvement of the eyesight (due to postinflammatory sequelae), and gradual disappearance of skin manifestations. A fourfold reduction in VDRL (1:128) and TPHA (1:256) was seen.
In our case, as often happens, syphilis did not manifest itself in a classical way -- not only the joint involvement, but also the absence of the most common signs (maculopapular rash, condylomata lata, mucosal changes, and related lymphadenopathy). This reminds us that secondary syphilis can have many faces and may have unusual presentations, mimicking several diseases. Multi-organ pathogenicity of T. pallidum can lead to misinterpretation of systemic symptoms, and, for this reason, a high index of clinical suspicion is necessary to rule out similar clinical presentations. Syphilis should be considered in a case of macular, papular, or palmoplantar eruptions with unusual clinical features, not responding to therapy. A prompt and correct treatment is essential to prevent possible permanent consequences.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Guarneri F, Barbuzza O, Vaccaro M, Galtieri G. Allergic contact dermatitis and asthma caused by limonene in a labourer handling citrus fruits. Contact Dermatitis 2008;58:315-6.
[Google Scholar]
|
| 2. |
Davatchi F, Assaad-Khalil S, Calamia K T, Crook J E, Sadeghi-Abdollahi B, Schirmer M,et al. The international criteria for behçet's disease (ICBD): A collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol 2014;28:338-47.
[Google Scholar]
|
| 3. |
Woolston SL, Dhanireddy S, Marrazzo J. Ocular syphilis: A clinical review. Curr Infect Dis Rep 2016;18:36.
[Google Scholar]
|
| 4. |
Park KH, Lee MS, Hong IK, Sung JY, Choi SH, Park SO, et al. Bone involvement in secondary syphilis: A case report and systematic review of the literature. Sex Transm Dis 2014;41:532-7.
[Google Scholar]
|
| 5. |
Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64:34-51.
[Google Scholar]
|
Fulltext Views
5,191
PDF downloads
3,082





