Translate this page into:
Xanthoma disseminatum: A red herring xanthomatosis
2 Department of Pathology, Dr. R. P. Govt. Medical College, Kangra (Tanda), Himachal Pradesh, India
Correspondence Address:
Vikram K Mahajan
Department of Dermatology, Venereology and Leprosy, Dr. R. P. Govt. Medical College, Kangra (Tanda)-176 001, Himachal Pradesh
India
| How to cite this article: Mahajan VK, Sharma AL, Chauhan PS, Mehta KS, Sharma V, Sharma S. Xanthoma disseminatum: A red herring xanthomatosis. Indian J Dermatol Venereol Leprol 2013;79:253-254 |
Sir,
Xanthoma disseminatum (XD) is a rare nonfamilial cutaneous non-Langerhans cell histiocytosis that manifests clinically as discrete reddish-brown or reddish-yellow, xanthoma-like papules and nodules involving the face, body flexures, oropharyngeal, laryngeal, conjunctival, and corneal mucosae in a normolipemic and euthyroid patient. Depending upon its evolution and prognosis, it is grouped in three forms: (1) A self-healing form with spontaneous resolution; (2) A persistent form (commonest) in which lesions may never resolve; and (3) A very rare progressive form with organ dysfunction and central nervous system involvement. [1] Laboratory parameters and radiological features are usually nonspecific unless associated with intracranial involvement. [1] Its diagnosis is clinicopathological and positive immunohistochemical staining for the non-Langerhans cell surface markers CD 68 and factor XIIIa. Differentiation from dyslipidemic xanthomas is important in view of morbidity and mortality it causes and for treatment. We describe a classic case of XD for documentation of this uncommon dermatosis.
An 18-year-old boy of non-consanguineous parentage developed multiple, discrete, grouped, orange-brown, globoid and smooth-surfaced papulonodular lesions over neck, axillae, antecubital and popliteal fossae, inguinofemoral, perioral and peri nostril areas, anterior nares, and lid margins [Figure - 1]. The lesions had started as asymptomatic flesh pink to brown papules over antecubital fosse 2 months back and were progressive. His other siblings were reportedly healthy. Systemic examinations including oropharyngeal, ophthalmic, and otorhinolaryngological workup, and laboratory investigations including blood counts, serum biochemistry, thyroid function tests, lipidprofile, urinalysis, ECG, chest X-ray, and ultrasonographic studies were essentially normal. Histological examination of a skin lesion showed diffuse histiocytic proliferation, dermal infiltration of Touton giant cells, foreign body giant cells associated with scattered lymphocytes, neutrophils, plasma cells,and occasional foam cells, the features suggestive of XD [Figure - 2]a-c. Immunohistochemical studiesrevealed positive staining for the surface markers CD68 [Figure - 2]d and were negative for S-100, CD1a. He was put on treatment with azathioprine, 50 mg twice/day and prednisolone, 40 mg on alternate days. After 3 months of this treatment, new lesions stopped appearing and there was softening of the existing lesions. At last contact, he had stopped treatment for affordability concerns.
 |
| Figure 1: Discrete and grouped reddish-brown, smooth-surfaced, globoid papules and nodules of xanthoma disseminatum over (a) antecubital fossa, (b) axillary fold, (c) neck fold, (d) popliteal fossae and (e) over lid margins, and perioral and peri nostril lesions (inset) |
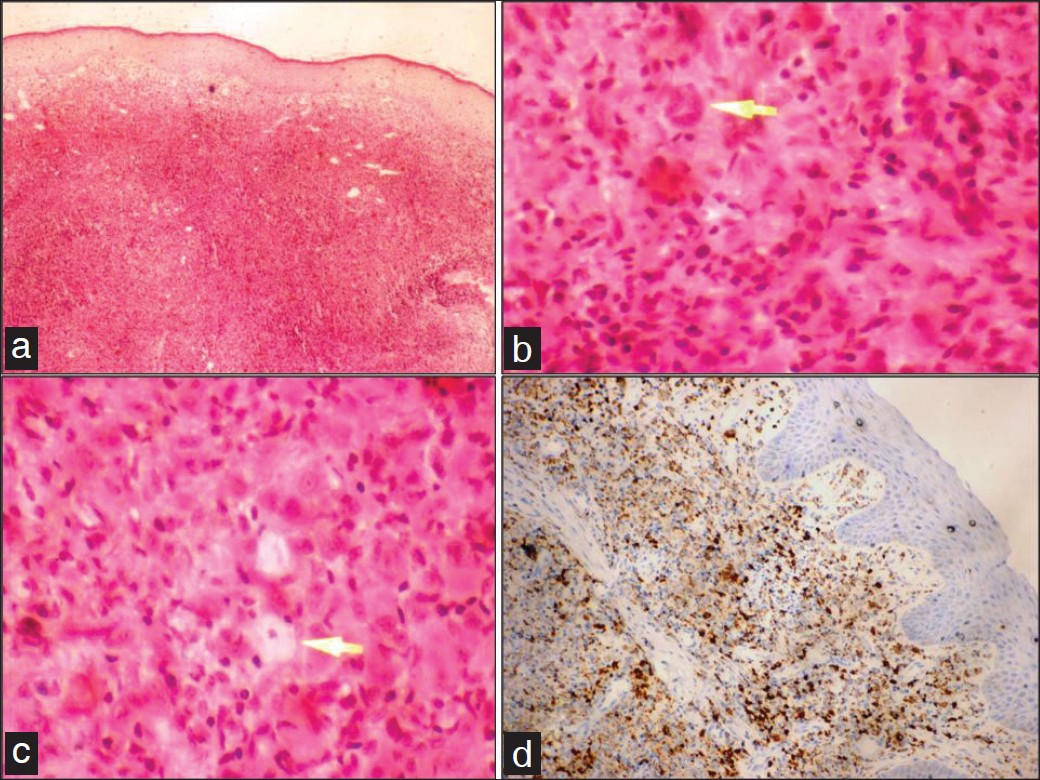 |
| Figure 2: (a) Thin and flattened epidermis with loss of rete pegs. Diffuse histiocytic proliferation, dermal infiltration of lymphocytes, neutrophils, and plasma cells (H and E, ×4), Arrows indicate a (b) touton giant cell and (c) foam cell (H and E, ×40). (d) A positive immunohistochemical staining for CD 68 surface markers |
XD predominantly affects males between 5 and 25 years of age in 60% cases, but it has been described in both sexes and in all age groups. Skin lesions have a predilection for scalp, face, trunk, extremities, and body folds. Involvement of eyelids, when severe, hinders the blinking and obscure visual field. [1] Mucosal lesions of gums, tongue, oropharynx, larynx, epiglottis, trachea, and bronchi occur in 50% cases and often cause dysphagia or dyspnoea at times requiring tracheostomy. Severe conjunctival or corneal involvement may lead to symblepharon and pterygium formations. [2] Diabetes insipidus affects 40% cases, is transitory and milder than that seen in Langerhans cell disease, and is due to involvement of the floor of the third ventricle and infundibulum. [1] Although facial lesions are disfiguring, a significant morbidity and mortality results from vital organ involvement. Sclerosing cholangitis, defecation difficulties, invasion of the perianal area from gastrointestinal complications, respiratory mucosal involvement causing upper airway obstruction, and death from intracranial involvement have been reported. [3],[4] Its pathogenesis remains unclear; the non-neoplastic but pathological non-X histiocytic cell proliferation reaction pattern of macrophage/monocyte origin is perhaps triggered by some superantigens. [2] The accumulation of lipids within the histiocytes is perhaps secondary to increased uptake, synthesis, or decreased efflux of lipids. [2] An early lesion reveals predominantly histiocytic proliferation and the mature lesion consists of a mixture of histiocytes, foam cells, Touton giant cells, and inflammatory cells within the dermis. This histiocytic proliferation is indicative of a histiocytic disorder, Touton giant cells represent an exaggerated xanthomatoid reaction pattern, and immunohistochemical studies staining positive for the surface markers CD 68 and factor XIIIa support it being a disorder of histiocytes/macrophages, whereas negative staining for S-100, CD1a and Birbeck granules excludes Langerhans cell histiocytosis. The treatment modalities, like vasopressin, corticosteroids, antiblastic chemotherapy, radiotherapy, cryotherapy, CO 2 LASER therapy, and surgical resection, used alone or in combination, have shown variable results. [1],[2],[3] Oral prednisolone (2 mg/kg/day) and azathioprine (2 mg/kg/day) did not show significant efficacy, a combination of lipid-lowering agents or azathioprine and cyclophosphamide was reportedly useful [2] but on the contrary, combination of oral steroids, clofibrate, and chemotherapy was effective in another study. [3] Bone marrow transplantation has been used successfully in life-threatening XD. [5] Recently, 2-chlorodeoxyadenosine therapy was found useful in maintaining remission and long-term control of cutaneous lesions. [6] Our patient exhibited classic features of XD and treatment with a combination of oral prednisolone and azathioprine was somewhat useful in him before he stopped treatment.
| 1. |
Kim JY, Jung HD, Choe YS, Lee WJ, Lee SJ, Kim D W, et al. A case of xanthoma disseminatum accentuating over the eyelids. Ann Dermatol 2010;22:353-7.
[Google Scholar]
|
| 2. |
Eisendle K, Linder D, Ratzinger G, Zelger B, Philipp W, Piza H, et al. Inflammation and lipid accumulation in xanthoma disseminatum: Therapeutic considerations. J Am Acad Dermatol 2008;58:S47-9.
[Google Scholar]
|
| 3. |
Kang TW, Kim SC. A case of xanthoma disseminatum presenting as pedunculating nodules and plaques. Korean J Dermatol 2007;45:290-3.
[Google Scholar]
|
| 4. |
Zak IT, Altinok D, Neilsen SS, Kish KK. Xanthoma disseminatum of the central nervous system and cranium. AJNR Am J Neuroradiol 2006;27:919-21.
[Google Scholar]
|
| 5. |
Savaºan S, Smith L, Scheer C, Dansey R, Abella E. Successful bone marrow transplantation for life threatening xanthogranuloma disseminatum in neurofibromatosis type-1. Pediatr Transplant 2005;9:534-6.
[Google Scholar]
|
| 6. |
Khezri F, Gibson LE, Tefferi A. Xanthoma disseminatum: Effective therapy with 2-chlorodeoxyadenosine in a case series. Arch Dermatol 2011;147:459-64.
[Google Scholar]
|
Fulltext Views
4,687
PDF downloads
1,997





