Translate this page into:
Familial atrophia maculosa varioliformis cutis: First case report from the Indian subcontinent with pedigree analysis
2 Department of Pathology, Muzaffarnagar Medical College, Muzaffarnagar, India
3 Department of Medicine, Muzaffarnagar Medical College, Muzaffarnagar, India
Correspondence Address:
Tarang Goyal
105 Somdutt Vihar, Meerut - 250 004, Uttar Pradesh
India
| How to cite this article: Goyal T, Varshney A, Bakshi S K. Familial atrophia maculosa varioliformis cutis: First case report from the Indian subcontinent with pedigree analysis. Indian J Dermatol Venereol Leprol 2012;78:182-185 |
Abstract
Familial atrophia maculosa varioliformis cutis is a very rare disorder with less than 28 cases being reported in the literature worldwide and remains a mystery both as far as genetics and the virtue of its pathogenesis is concerned. We present a case of mother and son, both having this disorder with presentations unique in terms of sites involved and try to draw a five generations pedigree chart for the same. We further support its inheritance pattern as autosomal dominant. Also, we propose oral isotretinoin as an effective treatment modality for the same.Introduction
One of the rare disorders in dermatology is familial atrophia maculosa varioliformis cutis (F-AMVC) with cases reported being countable on fingers. First described by Heidingsfeld [1] in 1918, most of the reported cases have been sporadic but some [2],[3],[4] authors report it to be of familial occurrence.
Case Report
We report two cases, mother and son with F-AMVC, these being the first cases to be reported from the Indian subcontinent.
First case is a female, 38 years of age presenting with asymptomatic, slightly pigmented, round, scar-mark like atrophic lesions present on face, neck, upper chest, back, forearms and arms since last 18 years with gradual increase in the number of lesions. On inspection, there were bilateral, multiple, discrete, both skin-colored and hyperpigmented, atrophic varioliform scar lesions on the above sites [Figure - 1] and [Figure - 2]. These lesions were sharply demarcated and varied from 0.2 to 1 cm in greatest diameter. There was no history of any preceding trauma, chicken pox or papular lesions in these areas. On face, predominance of lesions was reported around the angles of mouth, nose, forehead and cheeks. There was no erythema, scaling or herniation in these lesions. The lesions first started on face, followed by neck, chest, back and forearms.
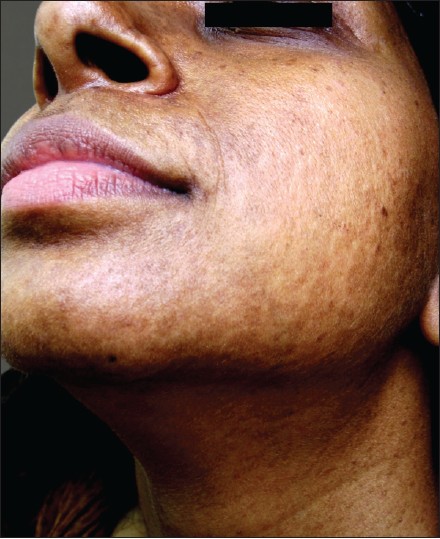 |
| Figure 1: Well-defined, slightly pigmented varioliform pit like lesions on face of proband |
 |
| Figure 2: The same lesions present on the back of the patient showing extensive involvement |
There is a history of similar lesions in her father and his sisters and according to him, his mother and grandmother also had similar lesions.
There was a slight aggravation of lesions in summer months as new lesions progressed more in size in these months, although progression was there in winters also; but no erythema or photosensitivity was reported. Biopsy was done and the histopathology of the lesions revealed slight epidermal dells, epidermal atrophy, loss of rete pegs with relatively decreased elastic tissue by H and E staining [Figure - 3]. With Verhoeff-van Gieson stain for elastin, there were multiple small areas of diminished and fragmented elastic tissue, the collagen was found to be normal [Figure - 4]. She was put on a trial dose of oral Isotretinoin at an initial dose of 40 mg/day for a period of 3 months followed by tapering the dose to 30 mg/day for next 1 month and surprisingly the lesions started clearing within few months. Presently she is on the same treatment with gradual tapering of the doses and proper follow-up in terms of monitoring of any history of depressive symptoms, headache, total and differential leucocyte counts, lipid profile and liver function tests.
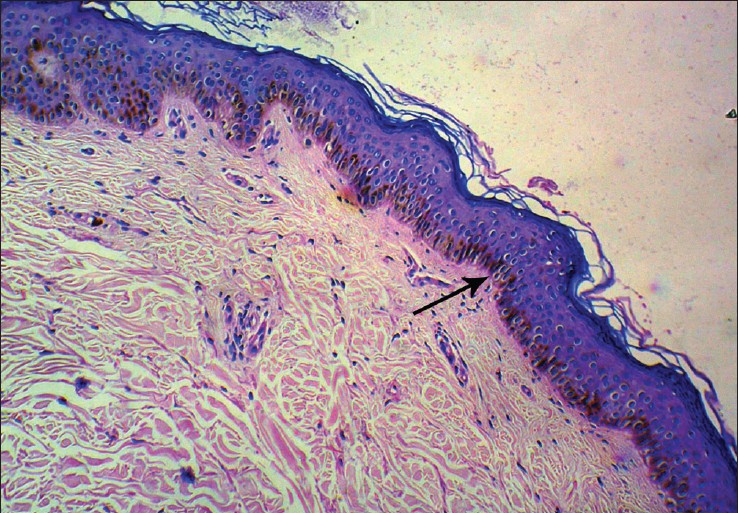 |
| Figure 3: Slide showing slight epidermal dells with epidermal atrophy, loss of rete pegs and slightly decreased elastin tissue. (H and E, ×40) |
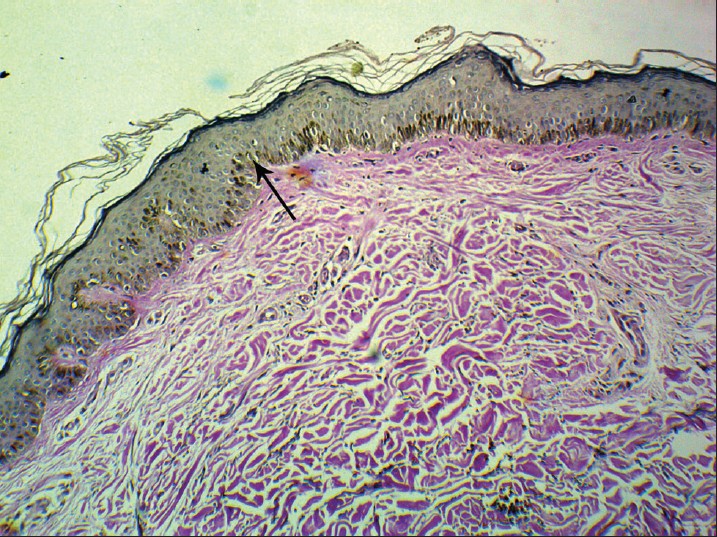 |
| Figure 4: Verhoeff-van Gieson stain for elastin showing multiple small areas of diminished and fragmented elastic tissue. (Verhoeff-van Gieson, ×40) |
The second case is a male child, aged 14 years, with lesions on face since last 3 years with a very gradual and slow onset [Figure - 5]. The lesions were totally asymptomatic in nature. Biopsy was not done as the parents did not consent for the same. But keeping in mind the type, distribution and mother′s lesions the diagnosis of F-AMVC was made and the child was put on oral Isotretinoin on a dose of 15 mg/kg (weight of the child 34 kg) followed by tapering. A survey of all the family members of proband was done and a family chart drawn to reach to any conclusion regarding the inheritance pattern [Figure - 6].
 |
| Figure 5: Child of proband showing atrophia maculosa varioliformis cutis lesions on cheek region |
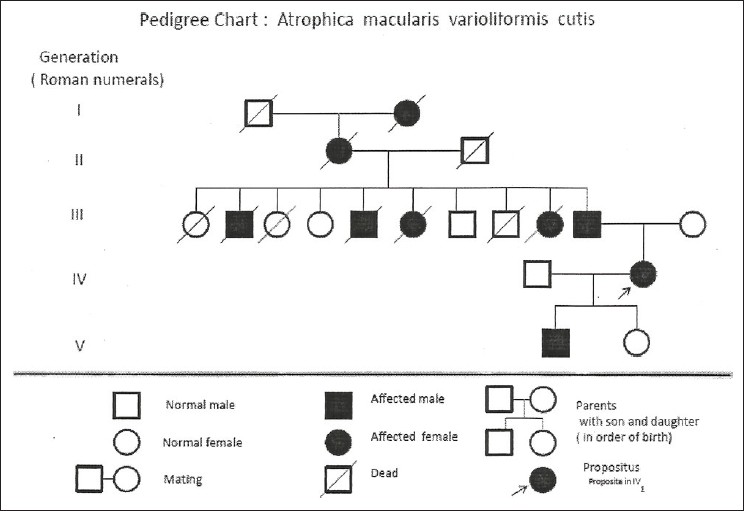 |
| Figure 6: Pedigree chart of family showing disease across five generations of the disease |
Discussion
The etiology and molecular basis of F-AMVC remains unclear even though it is suggested that it is a congenital disorder (OMIM 601341). Association of disorders as pachydermodactyly, [5] extrahepatic biliary atresia [6] and keratosis pilaris atrophicans has been reported in literature but these can be chance associations also.
It is characterized clinically by spontaneous occurrence of asymptomatic, punctuate or linear scar marks on the cheeks and forehead of young individuals. [7]
The age reported has been 5-37 years in literature. [8] No ethnic or racial prediliction has been reported in literature, also both sexes have been seen to be affected equally. The histopathology of the skin rash is nonspecific. Dall′Oglio et al., [9] were the only authors who demonstrated that in the papillary dermis there were compact collagen bundles, and at the ultrastructural level fibroblasts exhibit hyperplasia of the rough endoplasmic reticulum and elastin appeared in the form of numerous small, fragmented clumps.
The differentials include atrophoderma vermiculatum, anetoderma, ulerythema, acne, trauma and dermatitis artefacta.
Multiple symmetrical, inflammatory papules around hair follicles leading to pitted, atrophic depressed scars in reticulate or honey comb pattern are characteristic Acne shows comedones, papules and scarring of various gradings.
Our cases are a unique in terms of distribution of lesions as there is extensive distribution on face, upper back, neck and forearms which has not been previously seen as per our knowledge. There is no previous case report which reports five generations of the disorder.
Qu et al., [10] have reported it previously in three generations only. Also, there have been no reports whatsoever of healing of these lesions with isotretonoin therapy [Figure - 7]. Retinoids have both direct and indirect effects on gene transcription mediated through binding to their hormone response element in the promoter region of target genes and downregulation of genes not containing hormone response element in their promoter region. The retinoid receptor complex probably antagonises various proinflammatory and proliferative response as activator protein 1 (AP-1) or nuclear factor interleukin 6 (NF-IL-6). The pleomorphic effects of retinoids, as well as relatively selective targeting of skin structures, explain their broad potential benefit for patients with skin benefits and FDA unapproved clinical usages in a vast number of dermatological disorders is a striking evidence for the same. [11] Although we cannot assess for sure what would be the recurrence outcome of the lesions once the dosages are gradually tapered and stopped altogether, still it seems a good therapeutic option at present.
 |
| Figure 7: Post-isotretinoin treatment of patient showing significant improvement of lesions |
| 1. |
Heidingsfeld ML. Atrophia maculosa varioliformis cutis. J Cutan Dis 1918;36:285-8.
[Google Scholar]
|
| 2. |
Criado PR, Pegas JR, Tebecherani A, Souza AC, Sueto M, Pires MC. Atrophia maculosa varioliformis cutis: A case with extrafacial involvement and familial facial lesions. J Eur Acad Dermatol Venereol 2005;19:764-6.
[Google Scholar]
|
| 3. |
Gordon PM, Doherty VR. Familial atrophia maculosa varioliformis cutis. Br J Dermatol 1996;134:982-3.
[Google Scholar]
|
| 4. |
Kalayciyan A, Kotogyan A, Demirkesen C, Tüzün Y. Familial atrophia maculosa varioliformis cutis. Int J Dermatol 2003;42:530-2.
[Google Scholar]
|
| 5. |
Callot V, Wechsler J, Hovnanian A, Revuz J. Pachydermodactyly and atrophia maculosa varioliformis cutis. Dermatology 1995;190:56-8.
[Google Scholar]
|
| 6. |
Venencie PY, Foldès C, Cuny M, Samuel D, Bismuth H. Atrophia maculosa varioliformis cutis with extrahepatic biliary atresia. J Am Acad Dermatol 1989;21:309.
[Google Scholar]
|
| 7. |
Kolenik SA, Perez MI, Davidson DM, Morganroth GS, Kohn SR, Bolognia JL. Atrophia maculosa varioliformis cutis: Report of two cases and review of the literature. J Am Acad Dermatol 1994;30:837-40.
[Google Scholar]
|
| 8. |
Paradisi M, Angelo C, Conti G, Palermi G, Provini A. Atrophia maculosa varioliformis cutis: A pediatric case. Pediatr Dermatol 2001;18:478-80.
[Google Scholar]
|
| 9. |
Dall'Oglio F, Nasca MR, Taparelli F, Bacchelli B, Micali G. Familial atrophia maculosa varioliformis cutis: An ultrastructural study. Pediatr Dermatol 2001;18:230-3.
[Google Scholar]
|
| 10. |
Qu T, Wang B, Fang K. Familial atrophia maculosa varioliformis cutis: Case report and pedigree analysis. Br J Dermatol 2005;153:821-4.
[Google Scholar]
|
| 11. |
Arechalde A, Saurat JH. Retinoids: Unapproved uses or indications. Clin Dermatol 2000;18:63-76.
[Google Scholar]
|
Fulltext Views
6,160
PDF downloads
2,446





