Translate this page into:
Pulmonary and cutaneous sarcoidosis in a treated case of renal tuberculosis
2 Department of Tuberculosis and Respiratory Medicine, Geetanjali Medical College, Udaipur, Rajasthan, India
Correspondence Address:
Lalit K Gupta
A-3, Sai Villa, Opposite Head Post Office, Madhuvan, Udaipur- 313 001, Rajasthan
India
| How to cite this article: Gupta LK, Luhadia S K, Khare A K, Garg A, Mittal A, Kuldeep C M. Pulmonary and cutaneous sarcoidosis in a treated case of renal tuberculosis. Indian J Dermatol Venereol Leprol 2012;78:229 |
Sir,
Tuberculosis and sarcoidosis are chronic diseases which can occur in the same patient rarely. It has been suggested that infective agents including Mycobacteria, Propionibacteria, fungi such as Candida, and parasites such as Schistosoma, are likely triggers in a genetically predisposed individual and that this initial event leads to the sarcoidal granulomatous response. [1] The histological similarity between sarcoidosis and tuberculosis featuring epitheloid cell granuloma as a typical common finding, has stimulated the search for an association between sarcoidosis and mycobacteria. We, herein, report a case who developed sarcoidosis after successful treatment of renal tuberculosis.
A 65-year-old female presented with a 4-year history of multiple, progressive, asymptomatic dull erythematous plaques over face [Figure - 1]a and forearm [Figure - 1]b. Fresh papulo-nodular lesions on the face, trunk and thighs started to appear for the last 1 year. This was accompanied by progressive breathlessness, cough with expectoration, heaviness in chest, joint pains and intermittent low-grade fever. She was diabetic and hypertensive taking metformin, glimepride and ACE inhibitor, ramipril. She received antitubercular treatment (ATT) 4 years ago for renal tuberculosis; the diagnosis of which was made based on stricture affecting right ureter and caseating granulomas in iliac lymph node biopsy. With ATT her renal symptoms improved while cutaneous lesions had remained unchanged. Routine investigations on blood, urine and stool including blood biochemistry were normal except raised ESR (66 mm/1 st hr). Mantoux test was negative. Serum calcium and ACE levels were normal. Chest X-ray showed bilateral hilar lymphadenopathy, interstitial infiltrate and pleural thickening. CT thorax showed areas of fibrosis with honeycombing in both lower lobes, pleural thickening, pretracheal, subcarinal and right hilar lymphadenopathy. Ground glass haziness was also seen in bilateral lung fields. X-rays of hands and feet were normal. Pulmonary function test showed restrictive lung changes. Histopathological examination of the facial lesion showed small oval and round sarcoidal granulomas in upper dermis consisting of epitheloid cells and langhans giant cells [Figure - 2]a and b. The findings were consistent with sarcoidosis. The patient was started on 60 mg oral prednisolone in consultation with the chest physician. The patient′s pulmonary complaints and cutaneous lesions showed remarkable improvement in 2-weeks time. There was complete resolution of skin lesions [Figure - 3]a, b and systemic symptoms in 2 months. Prednisolone was gradually tapered off over 6 months. There has been no recurrence of cutaneous and systemic symptoms for the last 6 months.
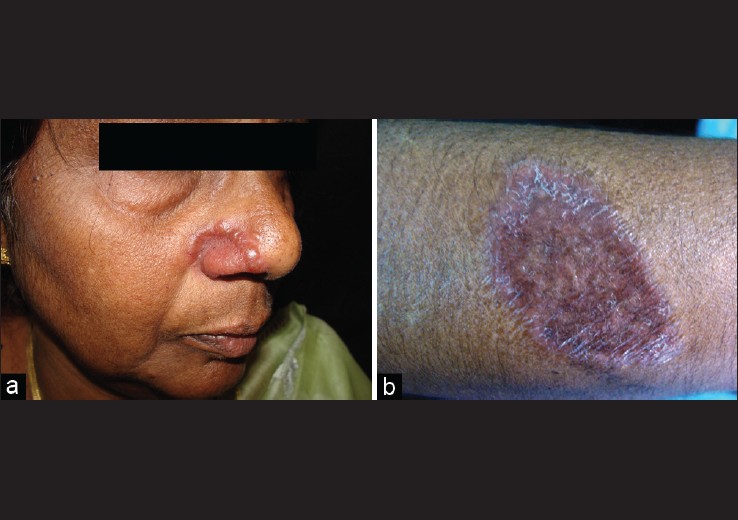 |
| Figure 1: (a) Shiny, erythematous annular plaque over right ala nasi. (b) Hyperpigmented, scaly annular plaque over right forearm |
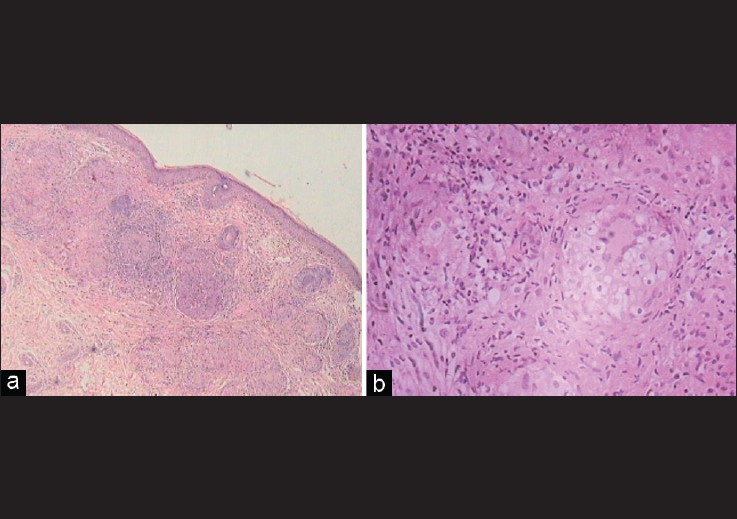 |
| Figure 2: (a) Skin biopsy showing oval and round sarcoidal granulomas in upper dermis (H and E, × 10). (b) Higher magnification showing collection of epitheloid cells with giant cells and few surrounding lymphocytes. (H and E, × 40) |
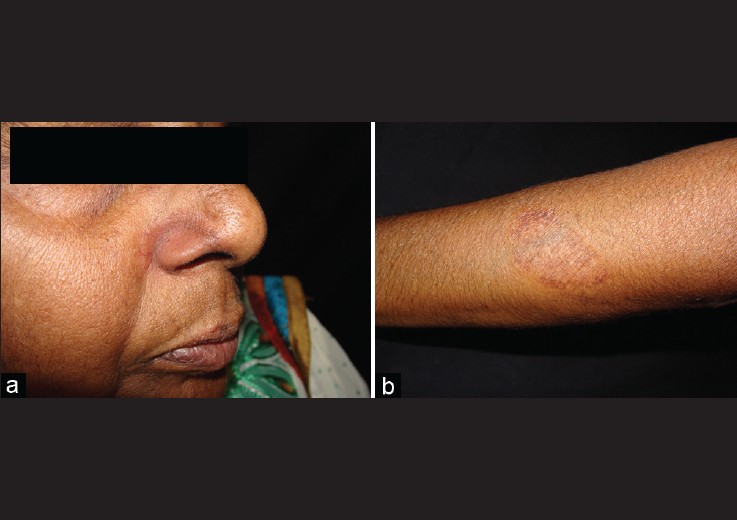 |
| Figure 3: (a, b) Post-treatment resolution of skin lesion |
Ever since the first description of sarcoidosis, there has always been a belief that the disease in some way could be related to tuberculosis. Some studies [1],[2],[3],[4],[5] lend support to this observation. Ning et al., [5] showed the presence of mycobacterial DNA by PCR analysis in 16 of 20 patients with cutaneous lesions of sarcoidosis. The isolation of genetic material from mycobacteria in granulomas of sarcoidosis suggests that the granulomas were initiated by mycobacteria but whether the organisms are viable is still debatable. Another pertinent question about the association of both the diseases is whether the ATT drugs alter the natural course of sarcoidosis or not. A study conducted by Gupta et al., [3] showed that the anti-tuberculosis therapy does not influence the outcome of sarcoidosis in the patient. This was observed in our patient also who had received ATT for renal tuberculosis but still developed new skin lesions and systemic symptoms of sarcoidosis.
Sarcoidosis is a great mimicker which can share a marked similarity with tuberculosis, particularly in a country like India where tuberculosis is common. This was seen in our patient also who was initially diagnosed as tuberculosis and was treated with ATT without any significant benefit to the skin lesions. Appearance of pulmonary symptoms, negative Mantoux test, sarcoidal histology of skin lesions, hilar lymphadenopathy, ground glass appearance of CT thorax, and response to prednisolone were strong pointers in favor of sarcoidosis in our patient. The purpose of presenting this case is to highlight the possible association of sarcoidosis and tuberculosis.
| 1. |
Gazauli M, Ikonomopoulos J, Koundourakis A, Bartos M, Pavlik I, Overduin P, et al. Characterization of mycobacterium tuberculosis complex isolates from Greek patients with sarcoidosis by spoligotyping. J Clin Microbiol 2005;43:4858-61.
[Google Scholar]
|
| 2. |
Ning L, Bajoghli A, Kubba A, Bhavan J. Identification of mycobacterial DNA in cutaneous lesions of sarcoidosis. J Cut Pathol 1999;26:271-8.
[Google Scholar]
|
| 3. |
Gupta D, Agrawal R, Aggarwal AN, Jindal SK. Molecular evidence for the role of mycobacteria in sarcoidosis: A meta-analysis. Eur Respir J 2007;30:508-16.
[Google Scholar]
|
| 4. |
Mise K, Goic-Barisic I, Puizina-Ivic N, Barisic I, Tonkic M, Peric I. A rare case of pulmonary tuberculosis with simultaneous pulmonary and skin sarcoidosis: A case report. Cases J 2010;3:24-31.
[Google Scholar]
|
| 5. |
Hatzakis K, Siafakas NM, Bouros D. Miliary sarcoidosis following miliary tuberculosis. Respiration 2000;67:219-22.
[Google Scholar]
|
Fulltext Views
2,310
PDF downloads
4,089





