Translate this page into:
Terra firma-forme dermatosis
2 Department of Pathology, Acibadem University School of Medicine, Istanbul, Turkey
Correspondence Address:
Emel Erkek
Acibadem Maslak Hospital, B�y�kdere Caddesi 40, Maslak 34457, Istanbul
Turkey
| How to cite this article: Erkek E, Sahin S, �etin ED, Sezer E. Terra firma-forme dermatosis. Indian J Dermatol Venereol Leprol 2012;78:358-360 |
Abstract
Terra firma-forme dermatosis is characterized by 'dirty' brown-grey cutaneous patches and plaques that can simply be eradicated by forceful swabbing with alcohol pads. The pathogenesis has been attributed to abnormal and delayed keratinization. Although affected patients present with typical lesions, the disorder is not well-known by dermatologists. In this report, we describe two patients with terra firma-forme dermatosis in the setting of xerosis cutis and atopic dermatitis. From a clinical point of view, we lay emphasis on its unique expression and diagnosis/treatment. From a histological perspective, we highlight its resemblance to dermatosis neglecta and speculate on the role of 'neglect' in a patient with seemingly adequate hygiene. The role of urea containing emollients in the development of this disorder remains to be determined.Introduction
Terra firma-forme dermatosis (TFFD) is a bizarre, acquired and idiopathic dermatosis. [1] The disorder was initially reported as a distinct entity by Duncan et al., [2] in 1987. The Latin phrase terra-firma means ′dry land′ and denotes a cutaneous discoloration resembling ′dirt′ (hence the alternative name Duncan′s Dirty Dermatosis). [3],[4]
Case Reports
Case 1
A 30-year-old woman presented with a 6-months history of persistent scaly pigmented patches on the armpits and torso. Subjective complaints were intense pruritus and cosmetic embarrassment. Her medical history was notable for xerosis cutis since childhood. She had been instructed by several doctors to avoid frequent bathing and to keep away from abrasive sponges and scrubs. She was bathing with tepid water without cleansers twice a week and promptly applying 10% urea containing emollients on moist skin.
Dermatological examination revealed brown-grey patches on both sides of the abdomen and axillae. There were islands of normal skin within the patches [Figure - 1]a. Initial tentative clinical diagnoses were terra firma-forme dermatosis, pomade crust, confluent and reticulated papillomatosis and acanthosis nigricans.
 |
| Figure 1: (a) Brown-grey pigmented patches on the abdomen with islands of normal skin in between. (b) Remarkable response to wiping of pigmented patches with a gauze pad saturated with alcohol |
Histopathological examination displayed prominent lamellar hyperkeratosis with whorls, keratotic plugging of follicular orifices, keratin globules in the stratum corneum, papillomatosis and sharp invaginations between the papilla, increased melanin pigment in the basal layer and minimal lymphocytic liquefaction [Figure - 2]a. Focal findings were noted in dermis; i.e., edema in the papillary dermis, pigment-laden macrophages, perivascular lymphocytic infiltration and erythrocyte extravasation. A Fontana-Masson stain showed focally increased melanin pigment in the basal layer of the epidermis [Figure - 2]b.
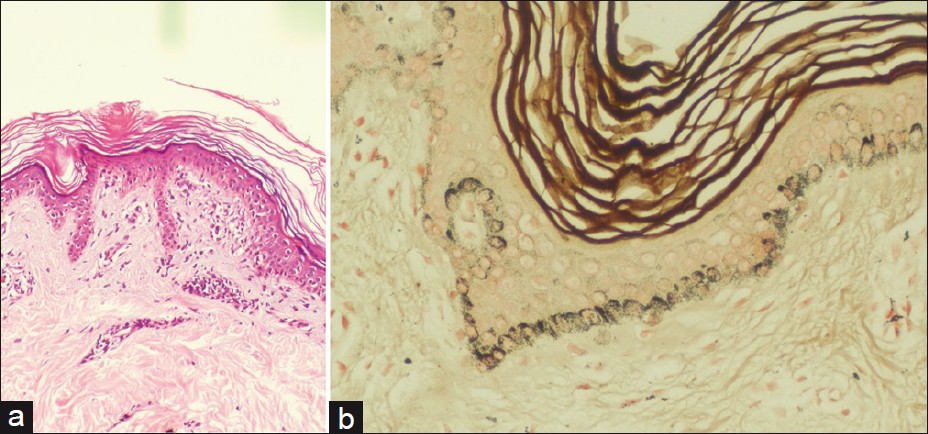 |
| Figure 2: Histopathological findings of the skin biopsy samples in Case 1: (a) Prominent lamellar hyperkeratosis with whorls, keratin globules in the stratum corneum, focal perivascular lymphocytic infiltration in the papillary dermis and lymphocytic liquefaction of basal layer (H and E, ×100). (b) Focally increased melanin pigment in the basal layer of the epidermis. (Fontana-Masson, ×200) |
Complete cure was attained by powerful swabbing of the skin with isopropyl alcohol-soaked gauze pads [Figure - 1]b. The patient was satisfied with the outcome of this intervention and there was no recurrence at 6 months of follow-up.
Case 2
A 20-year-old man presented with a 2-year history of itchy, thick and dark skin lesions. Previously he had received several prescribed and OTC topical medications without beneficial effects. His medical history was notable for atopic dermatitis. His washing habits consisted of daily shower and instant application of 10% urea containing emollients.
On dermatological examination there were reticular, brown-grey, pigmented plaques with a chamois leather appearance on the neck and upper back [Figure - 3]. Stigma of atopic dermatitis was also observed, i.e., Dennie-Morgan periorbital skin folds, allergic shiner, xerosis cutis and keratosis pilaris.
 |
| Figure 3: Thick, reticulated, brown plaques, resembling Morocco leather on the back. Note alcohol-wiped finger-like normal skin |
Biopsy was not attempted, since a ′wipe test′ with 70% ethyl alcohol accomplished clearance of lesions. A diagnosis of TFFD was established and patient was sent home with adequate information on how to get rid of this ′dirty′ appearance.
Discussion
TFFD is a recently described cutaneous pigmentation disorder. It is probably more prevalent than cited in the literature. [1],[3],[5] The disorder affects all age groups (age range: 3 months to 72 years) and both genders. [1],[3],[5],[6],[7]
Clinically, TFFD is characterized by brown-grey, velvety, pigmented patches or plaques. [1],[4],[6],[8] Involvement of the face, neck, trunk or ankles is usual, although unusual sites such as scalp, lips, chest, axilla, back, umbilical area, pubis, arms and legs have been reported. [3],[5],[6],[7],[8],[9] The distribution may be localized, generalized or symmetrical. [6] Rarely palpable verrucous or papillomatous plaques, reticulated patches and focal slight scaling have been observed. [6],[7] Symptomatic cases are rare; however, TFFD is a cause of cosmetic concern. [1],[3] Lesions in our first patient consisted of brown-grey scaly patches with islands of normal skin. Intense pruritus was the most remarkable feature in this patient. Thick velvety, reticulated plaques were observed in our second patient.
The histopathological description encompasses prominent lamellar hyperkeratosis with focal areas of compact whorled orthokeratosis, [1],[3] papillomatosis, mild acanthosis and deposition of keratotic material within the valleys between the papilla. [9] There is no parakeratosis. Dermal inflammation is trivial. [4],[9] Other findings with special stains include increased melanin content in the compact hyperkeratotic and basal areas of the epidermis (Fontana-Masson), [1],[3] scattered keratin globules throughout stratum corneum (Toluidine blue) [1],[3],[9] and occasional yeast cells indicative of Pityrosporum (Periodic Acid Schiff). [3],[9],[10]
The precise mechanism of TFFD remains obscure. Existing data does not support a familial predominance or genetic susceptibility. [4],[6] One hypothesis portrays TFFD as a disorder of abnormal and delayed keratinization and incriminates incomplete keratinocyte maturation, melanin retention and buildup and compaction of scales in the pathogenesis. [4],[6],[8],[9] Accordingly, TFFD represents a retention, rather than a proliferative hyperkeratosis. [7]
Some reports have focused on sunlight exposure as a triggering factor. [1],[4],[5],[8]
The diagnosis of TFFD is confirmed by forceful rubbing with a gauze pad immersed into 70% isopropyl alcohol or ethyl alcohol. [1],[3],[4],[6] This diagnostic test prevents unnecessary laboratory work-up or biopsy. [5] In addition, it offers a magical and prompt therapeutic cure for the disorder. [1],[3],[4] A pink normal skin underneath is exposed after the wiping procedure. [9] Reappearance is unusual once the skin is devoid of ′dirty′ appearance. [1],[5] Prophylactic weekly application of alcohol has been recommended for resistant or recurrent cases. [1],[3] Patients should be reassured about the benign nature of TFFD and educated about the cleaning procedure. [3],[6]
Differential diagnosis includes acanthosis nigricans, confluent and reticulated papillomatosis, pityriasis versicolor, epidermal nevi, dirty neck syndrome of atopic dermatitis and dermatosis neglecta (DN). [1],[5],[6],[8],[9] Most of these disorders can be excluded by alcohol swab test. [1,5] DN results from ′neglect′, i.e., poor hygiene or inadequate skin cleansing. [10],[11],[12] TFFD is distinguished from DN arbitrarily by presence of adequate hygiene, absence of cornflake-like brownish scales and successful eradication of pigmentation with isopropyl alcohol in the former and effective clearance of lesions with soap and water in the latter. [1],[3],[4],[7],[8],[9],[10],[11] However, isopropyl alcohol is operative in both disorders. [1],[9] Histologically, DN is similar to TFFD, except for the absence of whorled hyperkeratosis in DN. [1],[9],[11] Nevertheless, the distinction between TFFD and DN is blurred and there seems to be a considerable clinical and histological overlap between the two disorders.
Both patients in this report had normal washing habits. However, because of their skin disease, they were advised to use oil soaps and emollients and avoid liquid cleansers and scrubs. We believe that TFFD could arise from failure to rinse oil soaps or liquid cleansers during shower. Alternatively, application of humectants such as urea-containing emollients on dry or eczematous skin could also be responsible. Remnant soaps, cleansers, emollients and pathological scaling in diseased skin may impart the skin adhesive or keratoplastic properties at some sites, preventing normal keratinocyte shedding and accumulating scales, dirt and sebum. Thus, TFFD might represent a milder form of DN, where ′neglect′ is unintentional or secondary to professional advice. Awareness of the condition is required in order to congregate similar observations.
| 1. |
Pavloviæ MD, Dragos V, Potocnik M, Adamic M. Terra firma-forme dermatosis in a child. Acta Dermatovenerol Alp Panonica Adriat 2008;17:41-2.
[Google Scholar]
|
| 2. |
Duncan WC, Tschen JA, Knox JM. Terra firma-forme dermatosis. Arch Dermatol 1987;123:567-9.
[Google Scholar]
|
| 3. |
Browning J, Rosen T. Terra firma-forme dermatosis revisited. Dermatol Online J 2005;11:15.
[Google Scholar]
|
| 4. |
Guarneri C, Guarneri F, Cannavò SP. Terra firma-forme dermatosis. Int J Dermatol 2008;47:482-4.
[Google Scholar]
|
| 5. |
Berk DR. Terra firma-forme dermatosis: A retrospective review of 31 cases. Pediatr Dermatol 2011. [In press]
[Google Scholar]
|
| 6. |
Guarneri C, Cannavò SP. Is this skin diseased, or is it just dirty? JAAPA 2009;22:17.
[Google Scholar]
|
| 7. |
Berk DR, Bruckner AL. Terra firma-forme dermatosis in a 4-month-old girl. Pediatr Dermatol 2011;28:79-81.
[Google Scholar]
|
| 8. |
O'Brien TJ, Hall AP. Terra firma-forme dermatosis. Australas J Dermatol 1997;38:163-4.
[Google Scholar]
|
| 9. |
Akkash L, Badran D, Al-Omari AQ. Terra Firma forme dermatosis. Case series and review of the literature. J Dtsch Dermatol Ges 2009;7:102-7.
[Google Scholar]
|
| 10. |
Choudhary SV, Bisati S, Koley S. Dermatitis neglecta. Indian J Dermatol Venereol Leprol 2011;77:62-3.
[Google Scholar]
|
| 11. |
Qadir SN, Ejaz A, Raza N. Dermatosis neglecta in a case of multiple fractures, shoulder dislocation and radial nerve palsy in a 35-year-old man: A case report. J Med Case Reports 2008;2:347.
[Google Scholar]
|
| 12. |
Martin LM, Mendes MF, Takaoka LE, Martin MM, Martin BM. Dermatosis neglecta: A report of two cases. An Bras Dermatol 2010;85:217-20.
[Google Scholar]
|
Fulltext Views
22,870
PDF downloads
5,015





