Translate this page into:
Correlating epidermal thickness and basement membrane length to angiogenesis in the centre and the periphery of vitiligo lesion
Correspondence Address:
Aroni Kyriaki
Mikras Asias 75 str, Goudi, Athens, 11527
Greece
| How to cite this article: Stylianos V, Eleftherios I, Nikolaos K, Kyriaki A. Correlating epidermal thickness and basement membrane length to angiogenesis in the centre and the periphery of vitiligo lesion. Indian J Dermatol Venereol Leprol 2012;78:368-371 |
Sir,
In vitiligo it is well-documented that epidermis is thicker than in normally pigmented skin in frozen sections and that inflammatory changes are more frequent and intense in the epidermis and dermis of perilesional skin. Moreover angiogenesis, vascular endothelial growth factor (VEGF)-positive cells and mast cells are increased in the center compared to the periphery. [1],[2],[3]
Based on the above we investigated the thickness of keratin, the subjacent epithelium and the length of the basement membrane in the center (final stage) and the periphery (initial stage) of vitiligo, in order to find any difference between the two areas of the same lesion and a possible correlation between epidermal thickness and increased dermal angiogenesis.
After the approval of the Ethical Committee of the Medical School of the University of Athens biopsies were taken with informed consent from a group of 33 Greek patients (9 men, 24 women; age range, 20-72 years), with different phototypes [Fitzpatrick II (n=7), Fitzpatrick III (n=11), Fitzpatrick IV (n=15)], all suffering from generalized vitiligo vulgaris, stable for at least 2 years. The patients did not reveal any hyper- or hyposensitivity to pain, heat, cold, tickle, or touch, and did not show other abnormal sensations in their involved or clinically nondepigmented (uninvolved) skin areas. The duration of the disease ranged from 2 to 35 years. The patients had not received any treatment for vitiligo for the last 5 years atleast.
Biopsies (4 mm) were taken from the center and the periphery of the same lesion in each patient. Every effort was made to ensure that the diameter of tissue taken, the subsequent measurement of basement membrane length and the percentage of shrinkage of the tissue specimen after excision, due to skin elasticity would not be affected by the procedure. The thickness of keratin layer and subjacent epithelium (granular layer to basement membrane) was measured in H-E (Hematoxylin-Eosin)-stained sections (center and periphery). The length of the basal membrane was measured in PAS (Periodic Acid-Schiff)-stained sections.
All above measurements were performed semi-automatically. Specifically, for the measurement of the thickness were selected five different sites including the thicker and the thinner of each section. Then by the appropriate image analysis software (Image ProPlus, V.5, Media Cybernetics, Bethesda, MD, USA) the measurements were performed automatically. A grid of 4-mm long was used to perform accurate measurement of the full length of the basal membrane and cases with slides not properly embedded and cut and with different full length between center and periphery were excluded.
Endothelial cells were visualized using mouse monoclonal antibody against CD34 (Novocastra, Leika Microsystems, Newcastle upon Tune, UK).
The evaluation of histochemical and immunohistochemical stains was made by image analysis.
Statistical analysis was based on paired-t test.
Results are demonstrated in [Table - 1], [Table - 2] and [Table - 3].
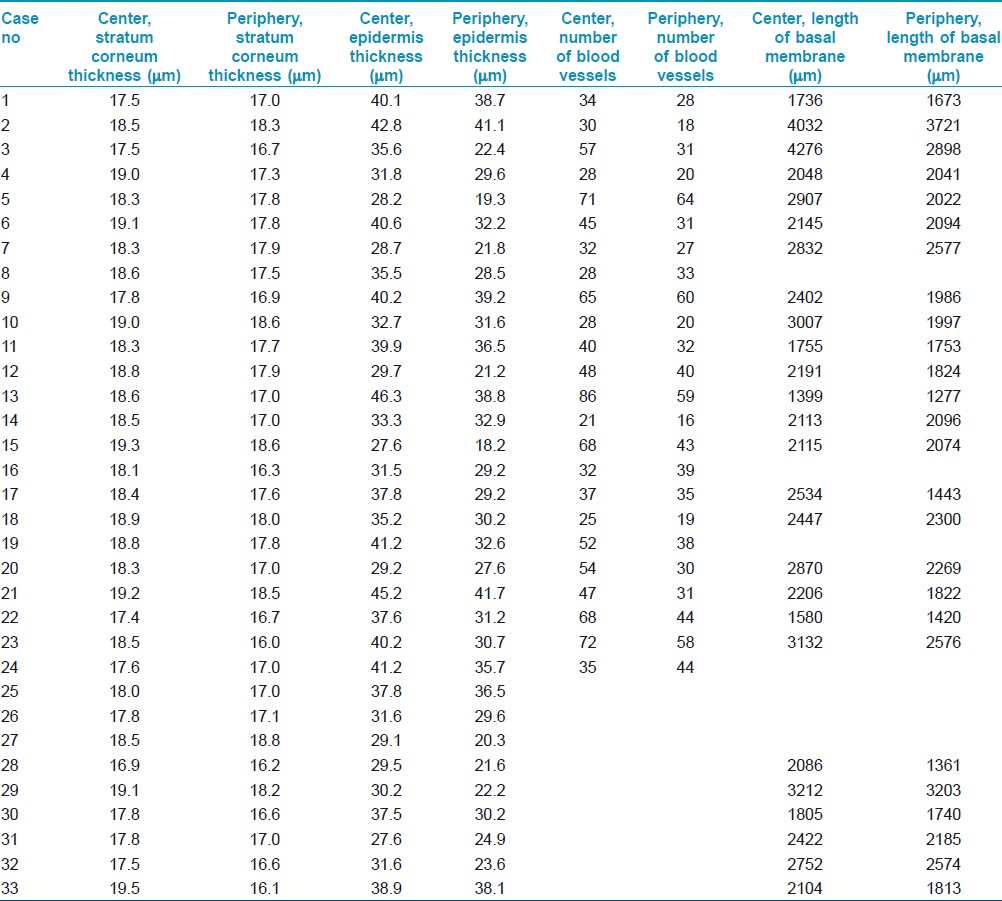
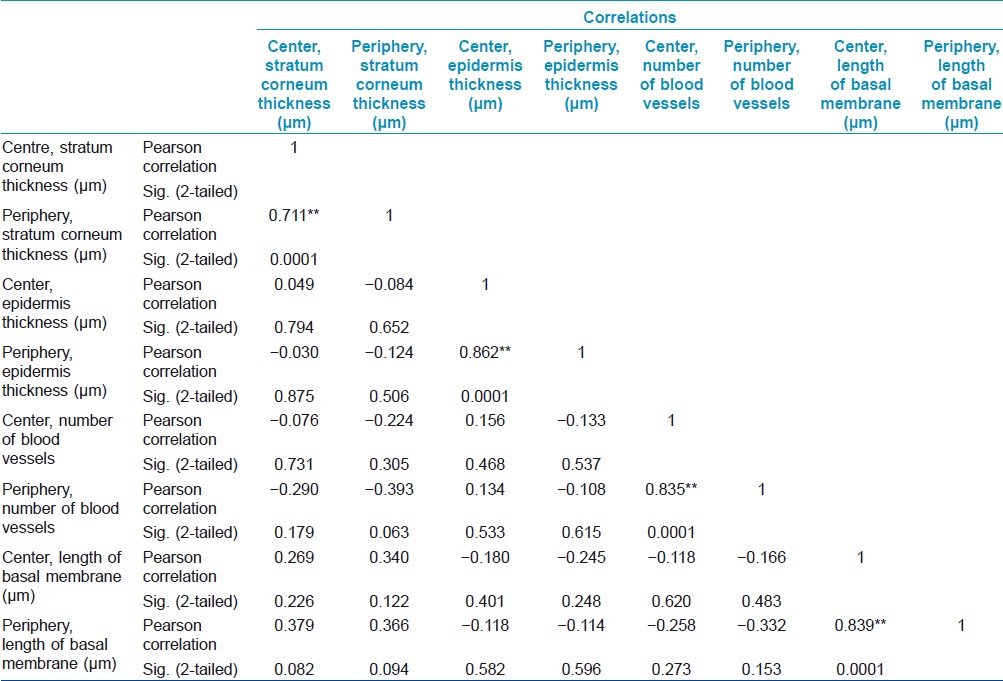
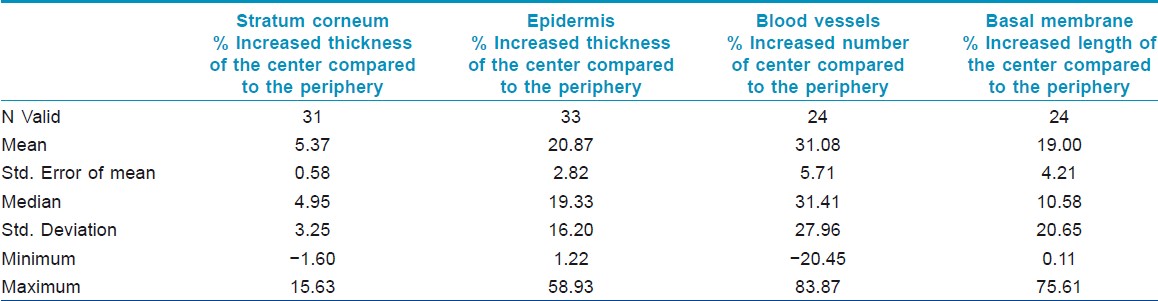
The increased thickness of the stratum corneum and the underlying epidermis and the loss of melanin were constant findings in all our cases, both in sun and non-sun-exposed sites, independently from the age of the lesion. In our study the thickness of stratum corneum and underlying epidermis in the center was higher, compared to the periphery of the lesion and basal membrane was longer in the center than in the periphery. Increased length of basement membrane is the result of increased number and/or length of epidermal rete ridges. All the above measurements allow us to conclude that the depigmented epidermis in vitiligo became hyperplasic with increased rete ridges.
It is well known that there are two routes of photoprotection, pigmentary and nonpigmentary route (increase of epidermal thickness). The last one is seen in vitiligo. [3] Epidermal hyperplasia in vitiligo occurs independently both in high and low sun exposed body areas. [1]
It has been reported that UV (Ultra Violet) exposure induces proliferation of the epidermal cells. Even a single exposure to UVB radiation can induce erythema, epidermal hyperplasia, and increased cutaneous vascularization. [4]
The increased number of dermal blood vessels in the center is also accompanied by hyperplasia of the overlying epidermis in 87% of our cases.
Epidermal hyperplasia and angiogenesis have an intimate relationship. Epithelial cells are dependent on the dermal blood supply during the phases of hyperproliferation. Evidence suggests that the stimulus for cutaneous neovascularization originates from epidermal, not dermal, cells. [4]
Angiogenesis accompanied by epidermal hyperplasia, is a histological finding observed also in psoriatic lesions. In psoriasis the morphological alterations of the blood vessels are prior to visible epidermal hyperplasia accompanied by lymphocytic infiltration. [5] In vitiligo there is not any known temporal correlation between increased angiogenesis and epidermal hyperplasia in the center of the lesion, where there is almost no lymphocytic infiltration. [2]
Factors like TNF-α (Tumor Necrosis Factor-alpha) and IL-6 (Interleukin-6) are increased in the center of vitiligo lesion compared to the periphery and can induce hyperplasia of the epidermis and increased number of blood vessels. [6]
In our study there wasn′t any linear correlation between these two parameters in the center of the lesion.
The loss of melanin leads to the above histopathological changes in the end stage of vitiligo, whereas its presence is important to maintain the normal cutaneous histological picture. This study, to the best of our knowledge, is the first to demonstrate the higher epidermal hyperplasia of the center compared to the periphery in vitiligo lesions, to correlate this epidermal hyperplasia to increased dermal angiogenesis and to attempt the measurement of basal membrane. Epidermal hyperplasia and accompanying increased angiogenesis may be part of a possible repairing/protective process. [7] We believe that the histological picture can help us understand disease′s pathogenesis better and lead us to choose the proper treatment.
| 1. |
Gniadecka M, Wulf HC, Mortensen NN, Poulsen T. Photoprotection in vitiligo and normal skin. A quantitative assessment of the role of stratum corneum, viable epidermis and pigmentation. Acta Derm Venereol 1996;76:429-32.
[Google Scholar]
|
| 2. |
Le Poole IC, van den Wijngaard R, Westerhof W, Das PK. Presence of T cells and macrophages in inflammatory vitiligo skin parallels melanocyte disappearance. Am J Pathol 1996;148:1219-28.
[Google Scholar]
|
| 3. |
Aroni K, Voudouris S, Ioannidis E, Grapsa A, Kavantzas N, Patsouris E. Increased angiogenesis and mast cells in the centre compared to the periphery of vitiligo lesions. Arch Dermatol Res 2010;302:601-7.
[Google Scholar]
|
| 4. |
Hennessy A, Oh C, Rees J, Diffey B. The photoadaptive response to ultraviolet exposure in human skin using ultraviolet spectrophotometry. Photodermatol Photoimmunol Photomed 2005;21:229-33.
[Google Scholar]
|
| 5. |
Heidenreich R, Röcken M, Ghoreschi K. Angiogenesis drives psoriasis pathogenesis. Int J Exp Pathol 2009;90:232-48.
[Google Scholar]
|
| 6. |
Kristensen M, Chu CQ, Eedy DJ, Feldmann M, Brennan FM, Breathnach SM. Localization of tumour necrosis factor-alpha (TNF-alpha) and its receptors in normal and psoriatic skin. Clin Exp Immunol 1993;94:354-62.
[Google Scholar]
|
| 7. |
Bielenberg DR, Bucana CD, Sanchez R, Donawho CK, Kripke ML, Fidler IJ. Molecular regulation of UVB-induced cutaneous angiogenesis. J Invest Dermatol 1998;111:864-72.
[Google Scholar]
|
Fulltext Views
2,520
PDF downloads
1,560





