Translate this page into:
Pediculosis capitis: An update
Correspondence Address:
Uday Khopkar
OPD 117, First floor, Old OPD building, Seth GS Medical College and KEM Hospital, Parel, Mumbai-400012, Maharashtra
India
| How to cite this article: Madke B, Khopkar U. Pediculosis capitis: An update. Indian J Dermatol Venereol Leprol 2012;78:429-438 |
Abstract
Head louse infestation, or pediculosis capitis, caused by Pediculus humanus var. capitis, is a common health concern in pediatric age group. An itching of the scalp is the chief symptom, whereas presence of viable nits confirms the diagnosis of head louse infestation. Secondary bacterial infection with impetignization with cervical and occipital lymphadenopathy can complicate the clinical scenario with physician misdiagnosing pediculosis to a primary bacterial infection. Screening and treatment of all close contacts is necessary for an adequate management of pediculosis. Medical management of head louse infestation requires proper application of topical pediculicidal agents', chiefly permethrin lotion and wet combing with a fine toothcomb. Severe cases with high parasitic load justify the use of either oral cotrimoxazole or Ivermectin. Other described technique involves a single application of hot air for 30 minutes. Radical but culturally unacceptable method would be shaving of scalp in resistant cases. Environmental fogging with insecticides is neither necessary nor recommended.Introduction
Pediculosis is an ectoparasitic infestation of human scalp. [1] The causative lice- Pediculus humanus var. capitis De Geer (Anoplura: Pediculidae), feed on the human blood. An infestation is commonly encountered in pediatric population in the age group of 6 - 12 years. [2] In rural areas, prevalence rate ranges from in the age group of 3 - 13 years, ranges varies from 13.3% to 49%. [3],[4],[5] Girls are 2 to 4 times more frequently infested than boys, especially in rural and developing areas owing to their hair length. Although pediculosis is not a major health problem (no vector-borne disease reported), it can be cause of social embarrassment, isolation, parental anxiety, peer-criticism, unnecessary absenteeism from academics and difficult issue for school authorities to handle. [6]
Life Cycle of the Lice
The human head louse (plural-lice): Pediculus humanus var. capitis is an ectoparasite of the order Psocodea whose only host is humans [Figure - 1]. The louse chiefly resides in close contact to human scalp and takes blood meals, which is postulated to be 6 times per day. [7] With each blood meal, a minute quantity of louse saliva gets inoculated into the scalp skin, and the host becomes sensitized to louse antigen and fecal matter eliciting an inflammatory response leading to scratching and secondary impetignization.
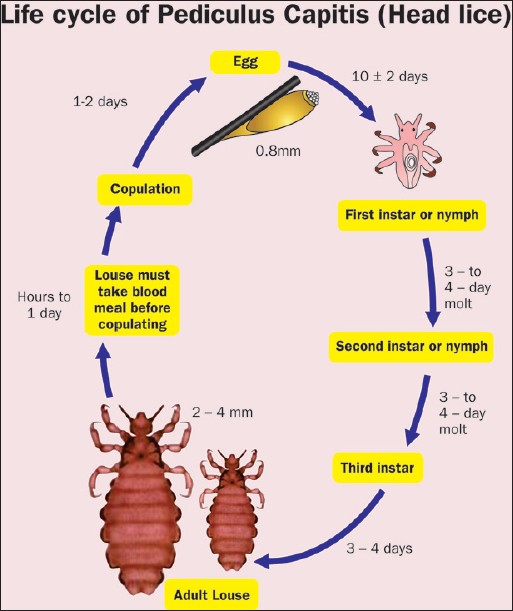 |
| Figure 1: Diagrammatic representation of life cycle of head louse Redrawn from Dermatology [Bolognia JL, Jorizzo JL, Rapini RP. (editors)], 2nd edition, Meinking TL, Burkhart CN, Burkhart CG, Elgart G, Infestations, page-1295, ©Elsevier (2008) |
The life cycle of the head louse has 3 stages: Egg, nymph and adult.
Egg
Eggs are laid by an adult fertile female and are cemented at the base of the hair shaft nearest the scalp [Figure - 2]. To attach each egg, the adult female secretes glue-like substance from her reproductive organ. This glue quickly hardens into a "nit sheath" that covers the hair shaft and the entire egg except for the operculum, a cap through which the embryo respires. They are hard to see and are often confused for dandruff or hair spray droplets. The term nit refers to either a louse egg or a louse nymph. These nits cannot be moved along the hair shaft in contrast to pseudonits. They are of size 0.8 mm by 0.3 mm, oval and usually yellow to white. Nits take about 1 week to hatch (range 6 to 9 days). Viable eggs are usually located within 6 mm of the scalp as morphogenesis is enhanced at human body temperature. A single fertile female can lay about 150 - 250 eggs during its 30-day life cycle. [8]
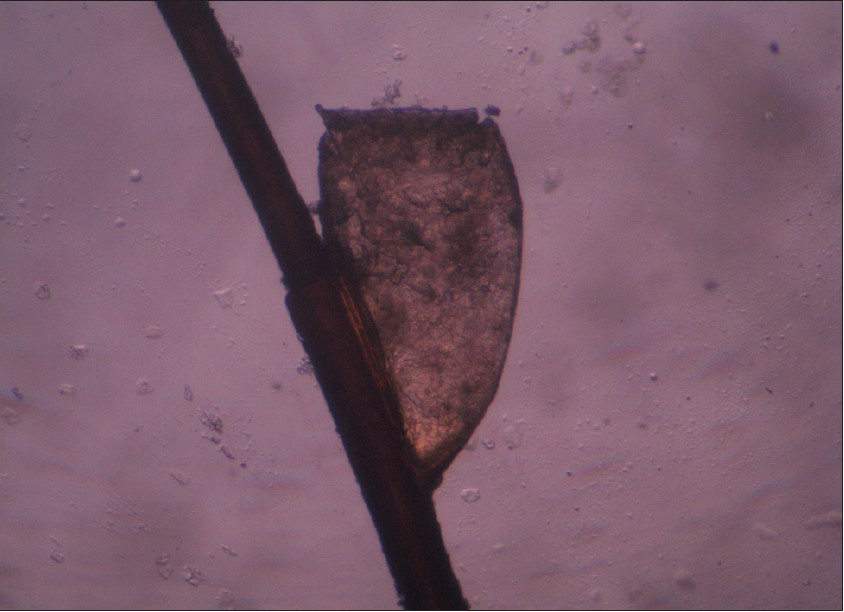 |
| Figure 2: Yellowish brown nit attached to hair shaft |
Nymph
The egg hatches to release a single nymph. The nit shell then becomes a more visible, dull yellow and remains attached to the hair shaft. The nymph looks like an adult head louse, but is about the size of a pinhead. Nymphs mature after 3 molts (instar) and become adults about 7 - 10 days after hatching. The first and second instar forms are relatively immobile, hence not easily transmitted between individuals; most spread is related to the third instar forms and adults form. [9]
Adult
The adult louse is about the size of a sesame seed i.e. 2 - 4 mm, has 6 legs (each with claws), and is tan to grayish-white. In persons with dark hair, the adult louse will appear darker. Females are usually larger than males and can lay up to 8 nits per day [Figure - 3]. An adult male usually dies after copulation- a phenomenon common in arthropod world. The female is distinguished from the male by her larger size and by the posterior protrusions that create an invaginated "V" structure, which she uses to cling onto the hair shaft for laying eggs. The male has dark brown bands across his back. Head lice move at a speed of up to 23 cm/min. Adult louse can live up to 30 days on a person′s head and, once mature, can lay up to 10 eggs per day. To live, adult louse need to feed on blood several times daily. Head louse rarely survives beyond 36 hours away from the host without a blood meal. [10] Adult head louse reproduce sexually, and copulation is must for female to lay eggs. Lice are repelled by light and will usually favor darker areas, hence girls are more heavily infested than boys do.
 |
| Figure 3: An adult female lice of approximately 3 mm in size. Note the claw at the distal end for clutching the hair shaft and presence of blood in the alimentary system |
Mode of Transmission
Close personal contact and sharing of headgear is the chief mode of transmission among susceptible contacts. Head-to-head contact is by far the most common route of lice transmission. [11] Head louse cannot fly as they lack wings, and they do not possess powerful legs for jumping. They move from one infested hair to another with the help of claw on their legs.
Clinical Features
After successful landing on scalp skin, head louse takes a blood meal (hematophagia) usually 4 to 5 times per day. While taking a blood meal, lice injects its saliva through the scalp skin to prevent clotting of blood, thereby maintaining the fluidity for an easy sucking. Chronic and heavy lice infestation can rarely lead to anemia, especially in rural females who are already suffering from iron deficiency anemia. On examination, one can see nits that are firmly attached to hair shaft within 6 mm from the scalp skin [Figure - 4]. Nits are often found in the occipital pit (louse pit) and retro-auricular areas of the head and are easier to observe than crawling adult lice. Skin is sensitized to louse antigen, introduced during blood meal or lice excreta whose chief symptom is severe pruritus. However, asymptomatic lice infestation is a common occurrence. Repeated scratching by the affected individual lead to loss of skin integrity with secondary bacterial infection and impetignization. Severe pyoderma of the scalp can rarely lead to irregular patches of cicatricial alopecia. Few patients can present with fever, malaise, irritability, and cervical and occipital lymphadenopathy. In contrasting to pubic lice, head louse do not affect the ciliary hairs (Pediculosis palpebrum). [12] Patients with plica polonica (plica neuropathica) can have innumerable nits and live lice [Figure - 5]. [13] In cases of pediculosis capitis with heavy infestation, plica polonica usually results due to entangled mass of hairs with exudates. Hyper infestation with head louse can lead to iron deficiency anemia in school children. [14]
 |
| Figure 4: Multiple nits present in a young female |
 |
| Figure 5: Plica polonica (Plica neuropathica) in a young schizophrenic female with abundant nits. (Photo courtesy by Professor Rachita Dhurat M.D) |
Diagnosis
The diagnosis of pediculosis capitis requires keen observation by the physician for viable eggs (nits), nymphs and live lice. One should spare an adequate time for thorough search for various stages of parasite. An examination carried out in haste can lead to misdiagnosis and can be counterproductive. [Table - 1] gives the differential diagnosis for pediculosis capitis.
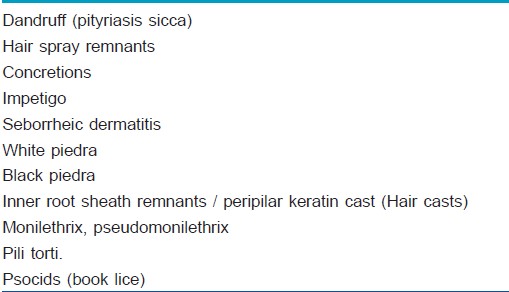
Peripilar keratin (hair) cast and flakes are freely movable along the hair shaft. In contrast to nits, which occupy only a part of circumference of hair shaft, hair casts and white piedra are circumferential. Book lice possess larger head, bigger mouthparts and longer rear legs. [15] The nits are easier to find in retroauricular areas and occipital area (louse pit). One should bear in mind that presence of nits is not sufficient for diagnosis as they can be non-viable; however, presence of nits within 7 mm of the scalp indicates an active louse infestation. Thorough combing with custom-made louse comb or fine toothcomb for 10 minutes can be a useful screening tool. [16] As lice seeks darker areas; mere visual inspection of hair shaft will prove counter-productive for establishing diagnosis. Use of magnifying lens can aid in visualization of ectoparasite either nits, nymph or adult live lice. Non-contact dermoscopy is a useful instrument for confirming the diagnosis with facility to store the images for future reference. In suspicious cases, dermoscopy can aid us to differentiate between pediculosis capitis and seborrheic dermatitis. [17] Any case of eczematous condition, affecting the scalp in a child, pediculosis capitis should be ruled out. In a mentally disturbed patient, pediculosis capitis needs to be differentiated from delusion of parasitosis (Ekbom′s disease) as management protocol differs entirely. Patients with delusional disorders usually bring with them dust-like particles in a matchbox or plastic bags mistaking them for insects (′Matchbox sign′).
Management
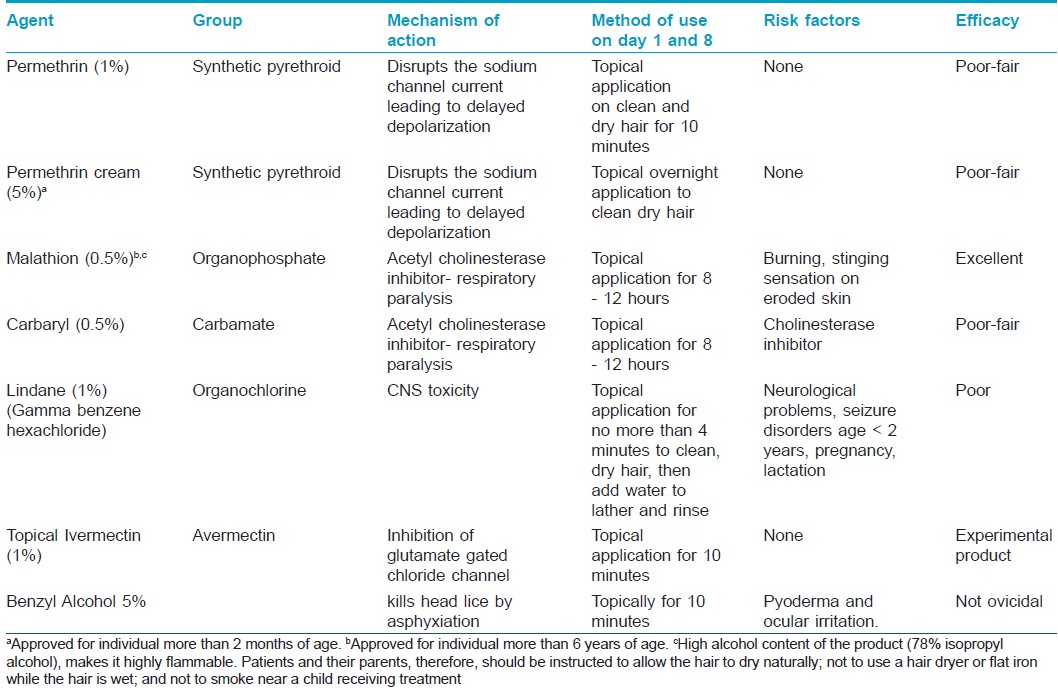
The cuticle of louse is lipoidal and allows penetration of insecticides according to law of partition. As per partition law, insecticides move from higher concentration (drug formulation) to lower concentration (cuticle waxes). The principle of treating ectoparasite infestation is that the parasite should acquire the maximum amount of drug with minimal systemic penetration into human. Various drug formulations that can be employed for treating pediculosis are [18]
- Phase separation lotions
- Evaporating lotions
- Insecticidal conditioning shampoo
Every suspected household member should be screened thoroughly, and if any sign of active infestation is noticed, then only treatment should be advised. The main aim of the treatment is to kill the ova (eggs, nits) and lice. This can be achieved with 3 most effective treatment options: Topical pediculicidal agents available in different formulations, wet combing and oral therapy. All pediculicidal agents should be rinsed after prescribed time limit with cool water over a sink. Rinsing with warm water can increase systemic absorption due to vasodilation of scalp vasculature. Any suspected bacterial infection should be treated with anti-staphylococcal antibiotic, preferably first-generation cephalosporin (cephalexin: Adult dose- 0·25 -1 gm 6 - 8 hourly/ children dose- 25 - 100 mg/kg/day) and further antibiotic therapy should be tailored as per microbiological studies.
In conjunction with medical treatment, disinfestation of surrounding household environment is necessary to prevent relapse and to achieve an adequate debugging. All clothing, towels, bed linens, upholstery used by an infested child within 2 days prior to diagnosis should be washed in hot water at about 50°C, or machine dried at the highest heat setting, for at least 30 minutes.
[Table - 2] gives brief information about various topical preparations that can be used as pediculicidal agent.
Removal of nit
As none of the topical insecticidal agent is 100% effective, it is reasonable to remove the nits manually. Removal of nits is a tedious and time-consuming procedure. Removal can be facilitated by combing wet hair with a fine toothcomb. Prior priming of nit-infested hair with vinegar (4% acetic acid) for 3 minutes dissolves the cementing substance that attaches nits to hair shaft and can make combing easier.
Wet combing
Mechanical removal of lice with the use of wet combing is a time-tested method. The rationale behind it is the fact that lice cannot move to another host within 7 days after hatching (first and second instar stage of nymph are non-motile), and cannot reproduce within 10 days, and all eggs hatch within 7 to 10 days. Therefore, if all young lice are combed out a few days after hatching, the infestation can be eradicated completely. The combing procedure is done on wet hair with added lubricant (hair conditioner or coconut oil/vegetable oil) and continued until no lice are found (15 to 30 minutes per session or longer for long, thick hair). Fine toothcombs on both sides are commonly available in Indian market at an affordable rate [Figure - 6]. In Chile, workers have shown that the diagnostic efficacy of metal microchaneled fine-toothed comb (Assy 2000) to be twice as fast and 3.6 times more efficient than through direct visual exam. [20] It is logical to use a comb of lighter shade (yellow, white, pink) to allow an easy visualization of lice. Combing is repeated once every 2 to 3 days for several weeks and should continue for 2 weeks after any session in which an adult louse is found.
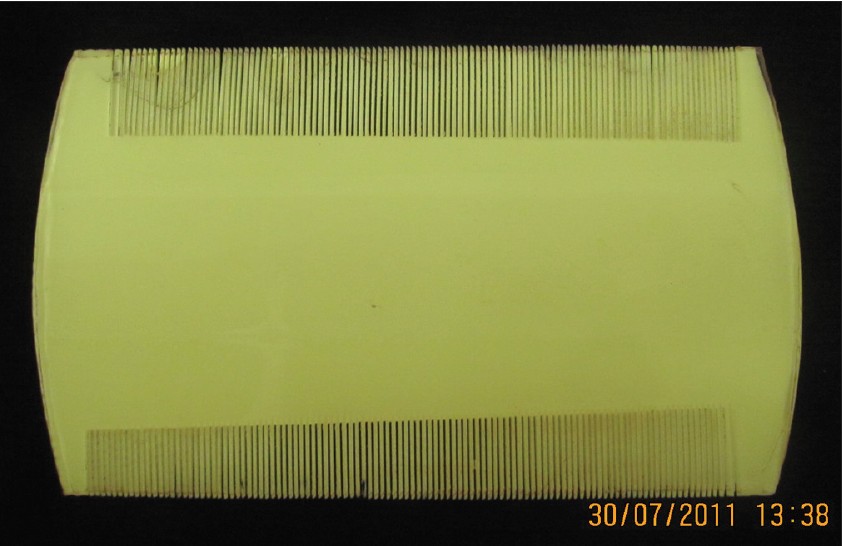 |
| Figure 6: Fine toothcomb available in market at an affordable price of Rs 10 (23¢) |
Hot-air treatment (Louse-buster) [21],[22]
Some investigators, for eradication of head-louse, have used constant flow of hot air. In this method, custom designed hand piece is attached to a hot air blower to expose the hair roots to puff of hot air. The whole assembly of instrument has been called as ′Louse buster with hand piece.′ A temperature of about 58° - 60°C is generated at an airflow rate of 88 cubic feet per minute, which is sufficient for causing thermal damage to nits, nymphs and live lice. The total time required for total scalp treatment is approximately 30-minutes. Louse buster method has demonstrated a lice mortality rate of 80% at 3 hours post-treatment and 98% of egg mortality (percentage of incubated eggs still unhatched after 2 weeks of treatment). The major advantage of this method is lack of resistance. Hot-air treatment is associated with minimal and tolerable discomfort. The machine is expensive, and the operator requires training in its use and can be a limiting factor in resource-poor settings. However, one must resist the temptation to use commonly available blow dryer as there is a chance of lice getting air-borne and can thus spread to other susceptible contacts even the treating physician!
Oral drugs
Systemic therapy of pediculosis acts as an adjuvant therapy in conjunction with topical treatment. Drugs like cotrimoxazole and ivermectin have demonstrated good efficacy against head lice while others like albendazole, levamisole have shown moderate killing effect.
Sulfamethoxazole / Trimethoprim is a sulfonamide-containing antibiotic, which has sequential blockade of action in the folate metabolism. Head lice depend on the vitamins B and folic acid, synthesized by bacterial flora present in its alimentary tract. When cotrimoxazole is administered to infested individual, drug reaches the circulation of lice during blood meal, as a result, gut flora of Pediculus is killed, and thereby depriving the lice of essential vitamins. [23] Death results from vitamin B deficiency. Cotrimoxazole is not approved by US-FDA for treatment of head lice.
Ivermectin
Ivermectin is an anthelminthic drug, structurally similar to the macrolide antibiotics without antibacterial activity, which is derived from Streptomyces avermitilis. [11] Ivermectin binds to glutamate-gated chloride channels with high affinity and specificity, which occur in invertebrate nerve and muscle cells, causing an increase in the permeability of the cell membrane to chloride ions of the nerve or muscle cell. This results in hyperpolarization, leading to flaccid paralysis culminating in the death of the parasite. Fortunately, Ivermectin have minimal affinity for mammalian glutamate gated chloride channel and does not readily cross the blood-brain barrier in humans. The recommended dose of Ivermectin is 200 μg/kg of body weight. 2 oral doses of 12 mg once a day at 7 - 10 days apart give satisfactory eradication. Due to an immaturity of blood-brain barrier in pediatric population, Ivermectin is not recommended below 5 years of age, pregnancy and lactation. In a recent study of 2010 where 44 children with an active infestation were treated with a single dose of 200 μg/kg, workers have noticed complete resolution of excoriations in all children, and minimal or no symptoms of pruritus were reported in 93% (N = 41). [24] Ivermectin is also available as a 1% topical preparation that is applied for 10 minutes and has shown promising results. [25]
Albendazole
Albendazole is a broad-spectrum antiparasitic pregnancy category X drug, used worldwide for treatment of various helminthic and protozoal infections. It has manifold action against the parasite, chiefly: Inhibition of mitochondrial function, uncoupling of oxidative phosphorylation and inhibition of glucose transport pathway, ultimately leading to ATP depletion and cell death. It also binds to β-tubulin protein of the microtubules of the parasite with high affinity and inhibits its polymerization. It is commonly employed in the dose of 400 mg as either single oral dose or repeated over 3 days. A repeat dose of 400 mg at day 7 - 10 has been recommended. Akisu et al have demonstrated the efficacy of 61.5% (single dose + repeated at day 7) and 66.6% (3 daily doses + repeated at day 7). [25]
Levamisole
Levamisole is an acetylcholine nicotinic receptor agonist, which is rapidly and almost completely absorbed from the gastrointestinal tract. Due to its agonistic action on acetylcholine receptor, there is tonic paralysis of the ectoparasite and killing. Levamisole also interferes with the carbohydrate metabolism of the parasite by inhibition of enzyme fumarate hydratase. In an uncontrolled pilot study, Namazi have demonstrated the efficacy of levamisole against pediculosis at a dose of 3.5 mg/kg administered for 10 days. [26] The recommended dose of levamisole for children between 10 - 19 kg body weight is 50 mg daily and 100 mg for those weighing between 20 - 39 kg body weight. [27]
Other treatment options
Another messy treatment option is to apply petrolatum jelly to entire scalp surface and hairs and left on overnight with shower cap. However, this method is messy and difficult to remove during bath. Thorough shampooing of scalp skin and hairs for 10 days is needed to remove the residual occlusive agent. This thick petrolatum jelly covers the operculum of eggs and respiratory apparatus of lice leading to asphyxiation and death. [28] Cetaphil® cleansing lotion has been shown to be effective in removal of lice by causing suffocation; however, the study was poorly randomized and had pitfalls in methodology. [29]
Newer developments
Spinosad (0·9% cream) is a recently introduced topical pediculicidal agent in the therapeutic armamentarium. [30] It is a fermentation product of the soil bacterium Saccharopolyspora spinosa. Spinosad is a natural mixture of the pediculicidal tetracyclic macrolides spinosyn A and spinosyn D. [31] It causes involuntary muscle contractions and widespread excitation of the arthropod central nervous system, eventually resulting in spastic and then later flaccid paralysis. It is left on the scalp and hair for 10 minutes and then rinsed with tap water. The hair is then shampooed as usual. In a comparative study between spinosad and permethrin, carried out by Stough and colleagues, spinosad (N = 243; without comb) was more effective than permethrin (N = 256; with comb) at the end of study period (94.2% vs. 68.1%). [32] According to a review done by Cole and Lundquist, spinosad can be considered a convenient and effective treatment for head lice in patients aged 4 years and older. [33]
In a recent paper by Vlckova and colleagues, efficacy of 3 different topical formulation: (a) Diffusil H Forte Spray (carbaryl 1%), (b) Diffusil Care (isopropyl myristate, cyclomethicone, and dimethiconol) and (c) Paranit (coconut oil, anise oil, and ylang ylang oil) was tested in an in-vitro conditions. Of the 3 preparations, the first 2 formulations, i. e. Diffusil H Forte Spray and Diffusil Care, caused 100% mortality of exposed lice while Paranit only killed 12.2% of exposed lice. [34]
Workers from Tamilnadu, India have tested the efficacy of hexane flower bud extract of Syzygium aromaticum (Myrtaceae) against P. humanus capitis in a closed and open chamber method. The percent adult mortalities were determined for every 5 in 60 min (closed method) and for every 10 in 180 min (open method). The closed method showed the percent mortality was 45, 88, and 100 at 5, 10, and 15 min, respectively. In the open-container method, the percent mortality was observed 5, 20, 47, 84, and 100 at 10, 20, 60, 120, and 180 min, respectively, thereby confirming that effect of hexane extract was due to the vapor phase exhibiting fumigant toxicity. [35]
Izri et al. has evaluated the pediculicidal and ovicidal effects of 1 application of a silicon-oil complex composed of dimethiconol and castor oil. As per the prospective study conducted by investigators, results showed the pediculicidal effect in 91.7% of treated subjects, whereas the ovicidal effect was shown in 73.2% of the study population, however; the efficacy of this newly studied formulation is at par with already available drugs like permethrin and malathion. [36]
Few authors have turned their attention to age-old remedies for an infestation, which is centuries old. The term galenic relates to second- century Greek physician Galen or a medicine made from natural rather than synthetic components. Investigators from Brazil have developed a safer galenic meta-emulsion (Oxyphthirine® ) comprising of triglycerides, isohexadecane, sorbitane ester and water. The globules of this emulsion were calibrated to the size of operculum of lice eggs, so that the lotion can penetrate inside the eggs and desiccate to form a physical plug, thereby blocking the gas exchange ability of the operculum and killing the growing larva. The meta-emulsion was shown to behave in a similar asphyxiating manner on the lice′s respiratory orifices. [37]
Choi and other co-workers have tested the efficacy of clove, Eugenia caryophyllata, and eucalyptus, Eucalyptus globulus, essential oils and 15 formulations containing these essential oils alone against susceptible and pyrethroid/malathion-resistant head lice. In their study of contact plus fumigant and human hair wig (placed over the head of mannequin) mortality bioassays, they found out that essential oils from eucalyptus (0.225 mg/cm 2 ) and clove (1.149 mg/cm 2 ) were less effective than either d-phenothrin (0.0029 mg/cm 2 ) or pyrethrum (0.0025 mg/cm 2 ). However, their work was significant in terms of better efficacy of eucalyptus applied as 8% sprays (15 or 20 ml) against pediculosis even to insecticide-resistant louse populations. [38]
Dimeticone 4% lotion is a physically acting pediculicidal compound based on 4% high molecular weight dimeticone in a cyclomethicone base. Dimethicone 4% lotion (Hedrin® 4% lotion) was being used in several European nations as an overnight topical pediculicidal agent with a moderate efficacy with either an incomplete eradication of infestation or complete inhibition of egg hatching. [39] However, the enthusiasm for its use began to decline in ensuing years due to an excessive fluidity of the dimethicone lotion and dripping of the active agent away from hair root, thereby rendering it ineffective. However, in a recent paper by Burgess and Burgess, the authors have demonstrated good ovicidal and pediculicidal action of dimethicone 4% gel after a single 15-minute application. [40] In a research letter, Heukelbach et al. have, in contrast, demonstrated the lack of efficacy of 4% dimethicone to kill young or mature eggs (0% and 0.3% efficacy), respectively. They have proposed the excellent ovicidal action of 92% viscous dimethicone with a 100% killing action on young eggs and 94.9% efficacy on mature eggs. [41]
Toloza and colleagues have assessed the insecticidal activity of essential oils from native and cultivated aromatic plants from Argentina for their activity against permethrin-resistant head lice. They studied 25 species of native and exotic plants in 13 different families, of which the plants from 4 species - Aloysia citriodora, Satureja parvifolia, Baccharis salicifolia and Chenopodium ambrosioides were the most effective. However, this study was conducted in an in vitro environment, these essential oils are yet to be incorporated in commercial formulations, and much research work is pending before they are labeled safe for human use. [42]
Resistance in Head Louse
Analogous to microbiological world, ectoparasitic conditions are showing with problem of resistance having novel mechanism. Resistance to topical pediculicides is an emerging concern in most parts of the world. The problem of resistance to a particular agent is directly related to the frequency of use of that agent in the affected population. A novel mechanism has been elucidated for gaining of resistance in voltage-sensitive sodium channel α-subunit gene termed as Knock down resistance (KDR), by virtue of which there is slower killing of lice, which can be encountered by sequential use of pediculicides and systemic agents. [43],[44] KDR mutation leads to insensitivity of nervous system of ectoparasite to compounds like DDT, the pyrethrins and the pyrethroids. 3 point mutations, resulting in the amino acid substitutions M815I, T917I and L920F in the voltage sensitive sodium channel (VSSC) α-gene of head louse have been identified in permethrin- and DDT resistant head lice. [45] An early detection of resistance to available pediculicidal agents is necessary, especially in areas where frequency of resistant lice is still low so that appropriate measures can be placed to reverse resistance development. [46] Marcoux et al. have conducted serial invasive signal amplification reaction (SISAR) for genotyping the T917I mutation and demonstrated that head lice possess resistance allele (R) frequency of 97.1%, whereas only 2.9% had a susceptible allele (S) frequency. [47]
Treatment of Contacts and Community Approaches
Pediculosis is a common health problem, especially among the impoverished sections of the society. [48] The prevalence of pediculosis capitis among primary school going children is around 3.6%. [49] Children below the age of 12 years, especially female bear the highest burden of disease. Oral Ivermectin in a dose of 200 μg/kg of body weight has been utilized as a household-wide treatment among susceptible populations in rural areas. Transmission of head louse can be tackled by periodic mass administration of oral Ivermectin as it has been showed that such mass treatment with oral ivermectin has halted the transmission of onchocerciasis in endemic areas. [50]
Community based treatment with oral ivermectin in susceptible, and poor sections of the society has given us a promising results with number of annual episodes of head lice infestation reduced from 19 to 14 in girls and from 15 to 5 in boys. [51] As per survey done by few workers, there exists a knowledge gap in understanding of head lice infestation among parents of children as well as a growing trend towards application of natural substances for prevention and treatment. Proper education of the public and health professionals and clear treatment plans are essential in combating pediculosis capitis. [52]
| 1. |
Angel TA, Nigro J, Levy ML. Infestations in the pediatric patient. Pediatr Clin North Am 2000;47:921-35.
[Google Scholar]
|
| 2. |
Bloomfield D. Head lice. Pediatr Rev 2002;23:34-5.
[Google Scholar]
|
| 3. |
Muhammad Zayyid M, Saidatul Saadah R, Adil AR, Rohela M, Jamaiah I. Prevalence of scabies and head lice among children in a welfare home in Pulau Pinang, Malaysia. Trop Biomed 2010;27:442-6.
[Google Scholar]
|
| 4. |
Bosely HA, El-Alfy NM. Head lice infestations (Anoplura: Pediculidae) in Saudi and non-Saudi school-aged children. J Egypt Soc Parasitol 2011;41:131-40.
[Google Scholar]
|
| 5. |
Amin TT, Ali A, Kaliyadan F. Skin disorders among male primary school children in Al Hassa, Saudi Arabia: Prevalence and socio-demographic correlates - A comparison of urban and rural populations. Rural Remote Health 2011;11:1517.
[Google Scholar]
|
| 6. |
Mumcuoglu KY, Klaus S, Kafka D, Teiler M, Miller J. Clinical observations related to head lice infestation. J Am Acad Dermatol 1991;25:248-251.
[Google Scholar]
|
| 7. |
Khokhar A. A study of pediculosis capitis among primary school children in Delhi. Indian J Med Sci 2002;56:449-52.
[Google Scholar]
|
| 8. |
Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol 2004; 50:1-12.
[Google Scholar]
|
| 9. |
Leung AK, Fong JH, Pinto-Rojas A. Pediculosis capitis. J Pediatr Health Care 2005;19:369-73.
[Google Scholar]
|
| 10. |
Orkin M, Maibach H. Scabies and pediculosis. In: Freedberg IM, Eisen A, Wolff K, Austen KF, Goldsmith LA, Katz SI, et al., editors. Fitzpatrick's dermatology in general medicine. 5th ed. New York: McGraw-Hill; 1999:2677-84.
[Google Scholar]
|
| 11. |
Frankowski BL, Weiner LB. Head lice. Pediatrics 2002;110:638- 43.
[Google Scholar]
|
| 12. |
Krishna A, Classic A. Pediculosis palpebrarum (le). Indian J Dermatol Venereol Leprol 1998;64:158.
[Google Scholar]
|
| 13. |
Pavithran K. Plica neuropathica causing traction alopecia. Indian J Dermatol Venereol Leprol 1990;56:141-2.
[Google Scholar]
|
| 14. |
Burke S, Mir P. Pediculosis causing iron deficiency anaemia in school children. Arch Dis Child 2011;96:989.
[Google Scholar]
|
| 15. |
Elston DM. What's eating you? Psocoptera (book lice, psocids). Cutis 1999;64:307-8.
[Google Scholar]
|
| 16. |
Mumcuoglu KY, Friger M, Ioffe-Uspensky I, Ben-Ishai F, Miller J. Louse comb versus direct visual examination for the diagnosis of head louse infestations. Pediatr Dermatol 2001;18:9-12.
[Google Scholar]
|
| 17. |
Badri T, Hammami H, Benmously R, Mokhtar I, Fenniche S. Dermoscopic diagnosis of pediculosis capitis. Acta Dermatovenerol Alp Panonica Adriat 2010;19:45-6.
[Google Scholar]
|
| 18. |
Maunder JW. Insecticides in pediculosis capitis. Arch Dis Child 1989;64:69-70.
[Google Scholar]
|
| 19. |
Meinking TL, Burkhart CN, Burkhart CG, Elgart G. Infestations. In: Bolognia JL, Jorizzo JL, Rapini RP. (editors) Dermatology, 2 nd edition, Spain: Mosby Elseveir; 2008:1297.
[Google Scholar]
|
| 20. |
Neira PE, Molina LR, Correa AX, Américo Muñoz NR, Oschilewski DE. [Metal microchanelled fine-toothed comb use in the diagnosis of pediculosis]. An Bras Dermatol 2009; 84:615-21.
[Google Scholar]
|
| 21. |
Goates BM, Atkin JS, Kevin G. Wilding KG, Kurtis G. Birch KG, et al. An Effective Nonchemical Treatment for Head Lice: A Lot of Hot Air. Pediatrics 2006;118:1962-70.
[Google Scholar]
|
| 22. |
Bush SE, Rock AN, Jones SL, Malenke JR, Clayton DH. Efficacy of the LouseBuster, a new medical device for treating head lice (Anoplura:Pediculidae). J Med Entomol 2011;48: 67-72.
[Google Scholar]
|
| 23. |
Dodd CS. Interventions for treating headlice. Cochrane Database Syst Rev 2001:CD001165.
[Google Scholar]
|
| 24. |
Ameen M, Arenas R, Villanueva-Reyes J, Ruiz-Esmenjaud J, Millar D, Domínguez-Dueñas F, et al. Oral ivermectin for treatment of pediculosis capitis. Pediatr Infect Dis J 2010;29: 991-3.
[Google Scholar]
|
| 25. |
Akisu C, Delibas SB, Umit Aksoy U. Albendazole: Single or Combination Therapy with Permethrin against Pediculosis Capitis. Pediatr Dermatol 2006;23:179-82.
[Google Scholar]
|
| 26. |
Namazi MR. Levamisole: A safe and economical weapon against pediculosis. Int J Dermatol 2001;40:292-4.
[Google Scholar]
|
| 27. |
Tripathi KD, editor. Essentials of Medical Pharmacology, 6 th edition, New Delhi: Jaypee Publications; 2010:812.
[Google Scholar]
|
| 28. |
Schachner LA. Treatment resistant head lice: Alternative therapeutic approaches. Pediatr Dermatol 1997;14:409-10.
[Google Scholar]
|
| 29. |
Pearlman D. Cetaphil cleanser (Nuvo lotion) cures head lice. Pediatrics 2005;116:1612
[Google Scholar]
|
| 30. |
Salgado VL. Studies on the mode of action of spinosad: Insect symptoms and physiological correlates. Pestic Biochem Physiol 1998;60:91-102.
[Google Scholar]
|
| 31. |
McCormack PL. Spinosad: In pediculosis capitis. Am J Clin Dermatol 2011;12:349-53.
[Google Scholar]
|
| 32. |
Stough D, Shellabarger S, Quiring J, Gabrielsen AA. Efficacy and Safety of Spinosad and Permethrin Creme Rinses for Pediculosis Capitis (Head Lice). Pediatrics 2009;124:389-95.
[Google Scholar]
|
| 33. |
Cole SW, Lundquist LM. Spinosad for treatment of head lice infestation. Ann Pharmacother 2011;45:954-9.
[Google Scholar]
|
| 34. |
Vlckova J, Rupes V, Chmela J, Kensa M, Mazánek L. In vitro efficacy of three novel delousing formulations against the head louse (Pediculus capitis L.). Epidemiol Mikrobiol Imunol 2011;60:41-2.
[Google Scholar]
|
| 35. |
Bagavan A, Rahuman AA, Kamaraj C, Elango G, Zahir AA, Jayaseelan C, et al. Contact and fumigant toxicity of hexane flower bud extract of Syzygium aromaticum and its compounds against Pediculus humanus capitis (Phthiraptera: Pediculidae). Parasitol Res 2011. [Epub ahead of print].
[Google Scholar]
|
| 36. |
Izri A, Uzzan B, Maigret M, Gordon MS, Bouges-Michel C. Clinical efficacy and safety in head lice infection by Pediculus humanis capitis De Geer (Anoplura: Pediculidae) of a capillary spray containing a siucon-oil complex. Parasite 2010; 17:329-35.
[Google Scholar]
|
| 37. |
Militão de Sousa F, Vasconcelos AW, de Nadon J, Duhot PY. Treatment of human head lice infestations in a single application with a new galenic lotion. Int J Cosmet Sci 2010. [Epub ahead of print].
[Google Scholar]
|
| 38. |
Choi HY, Yang YC, Lee SH, Clark JM, Ahn YJ. Efficacy of spray formulations containing binary mixtures of clove and eucalyptus oils against susceptible and pyrethroid/ malathion-resistant head lice (Anoplura: Pediculidae). J Med Entomol 2010;47:387-91.
[Google Scholar]
|
| 39. |
Burgess IF, Brown CM, Lee PN. Treatment of head louse infestation with 4% dimeticone lotion: Randomised controlled equivalence trial. BMJ 2005;330:1423-5.
[Google Scholar]
|
| 40. |
Burgess IF, Burgess NA. Dimeticone 4% liquid gel found to kill all lice and eggs with a single 15 minute application. BMC Res Notes 2011;4:15.
[Google Scholar]
|
| 41. |
Heukelbach J, Sonnberg S, Becher H, Melo I, Speare R, Oliveira FA. Ovicidal efficacy of high concentration dimeticone: A new era of head lice treatment. J Am Acad Dermatol 2011;64:e61-2.
[Google Scholar]
|
| 42. |
Toloza AC, Zygadlo J, Biurrun F, Rotman A, Picollo MI. Bioactivity of Argentinean Essential Oils Against Permethrin-Resistant Head Lice, Pediculus humanus capitis. J Insect Sci 2010;10:185.
[Google Scholar]
|
| 43. |
Bialek R, Zelck UE, Fölster-Holst R. Permethrin Treatment of Head Lice with Knockdown Resistance-like Gene. N Engl J Med 2011;364:386-7.
[Google Scholar]
|
| 44. |
Lee SH, Gao J-R, Yoon KS, Mumcuoglu KY, Taplin D, Edman JD, et al. Sodium channel mutations associated with knockdown resistance in the human head louse, Pediculus capitis (De Geer). Pestic Biochem Physiol 2003;75:79-91.
[Google Scholar]
|
| 45. |
Hodgdon HE, Yoon KS, Previte DJ, Kim HJ, Aboelghar GE, Lee SH, et al. Determination of knockdown resistance allele frequencies in global human head louse populations using the serial invasive signal amplification reaction. Pest Manag Sci 2010;66:1031-40.
[Google Scholar]
|
| 46. |
Heukelbach J, Wilcke T, Winter B, Feldmeier H. Epidemiology and morbidity of scabies and pediculosis capitis in resource-poor communities in Brazil. Br J Dermatol 2005;153:150-6.
[Google Scholar]
|
| 47. |
Marcoux D, Palma KG, Kaul N, Hodgdon H, Van Geest A, Previte DJ, et al. Pyrethroid pediculicide resistance of head lice in Canada evaluated by serial invasive signal amplification reaction. J Cutan Med Surg 2010;14:115-8.
[Google Scholar]
|
| 48. |
Abdel-Hafez K, Abdel-Aty MA, Hofny ER. Prevalence of skin diseases in rural areas of Assiut Governorate, Upper Egypt. Int J Dermatol 2003;42:887-92.
[Google Scholar]
|
| 49. |
Komba EV, Mgonda YM. The spectrum of dermatological disorders among primary school children in Dar es Salaam. BMC Public Health 2010;10:765.
[Google Scholar]
|
| 50. |
Winnen M, Plaisier AP, Alley ES, Nagelkerke NJ, van Oortmarssen G, Boatin BA, et al. Can ivermectin mass treatments eliminate onchocerciasis in Africa? Bull World Health Organ 2002;80:384-9.
[Google Scholar]
|
| 51. |
Pilger D, Heukelbach J, Khakban A, Oliveira FA, Fengler G, Feldmeier H. Household-wide ivermectin treatment for head lice in an impoverished community: Randomized observer-blinded controlled trial. Bull World Health Organ 2010;88: 90-6.
[Google Scholar]
|
| 52. |
Doulgeraki A, Valari M. Parental attitudes towards head lice infestation in Greece. Int J Dermatol 2011;50:689-92.
[Google Scholar]
|
Fulltext Views
34,612
PDF downloads
6,452





