Translate this page into:
Disseminated asymptomatic yellowish papules on the face, trunk and limbs in a 3-year-old boy
2 Department of Pathology, Tri-Service General Hospital, Taipei, Taiwan
Correspondence Address:
Chiang Chien-Ping
Department of Dermatology, Tri-Service General Hospital, No.325, Sec. 2, Chenggong Road, Neihu Dist., Taipei City 114
Taiwan
| How to cite this article: Ching-Fu H, GW, Bai-Yao W, Wei-Ming W, Chien-Ping C. Disseminated asymptomatic yellowish papules on the face, trunk and limbs in a 3-year-old boy. Indian J Dermatol Venereol Leprol 2011;77:537 |
History
A 3-year-old boy presented with asymptomatic, yellowish skin lesions scattered over his whole body. His parents stated that the lesions appeared about 1 year previously and that some flattened spontaneously [[Figure - 1], arrow]. His past medical history was unremarkable, but the parents had familial hyperlipidemia of unknown type. On physical examination, numerous asymptomatic 2-4 mm yellowish papules on the face, abdomen, back, and upper and lower extremities were seen that did not merge into plaques. Although no treatment was prescribed, some lesions spontaneously resolved with hyperpigmentation. Laboratory investigation of lipid profiles showed low-density lipoprotein cholesterol (84 mg/dl; normal value < 130 mg/dl), total cholesterol (160 mg/dl; normal value < 200 mg/dl), triglyceride (50 mg/dl; normal value < 160 mg/dl). Histopathology of the representative skin lesion (thigh) showed diffuse dermal infiltrate of foamy histiocytes [Figure - 2] and [Figure - 3].
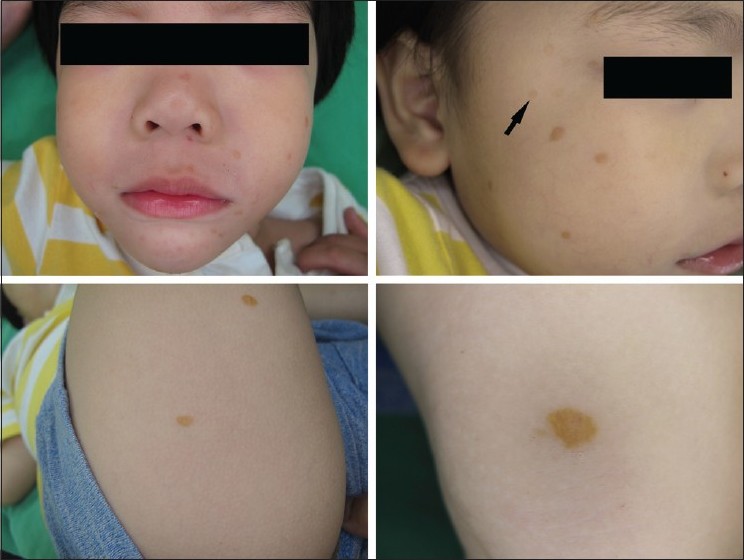 |
| Figure 1: Multiple yellowish papules scattered on the perioral area, bilateral cheeks and thighs. Some lesions spontaneously flattened (arrow) |
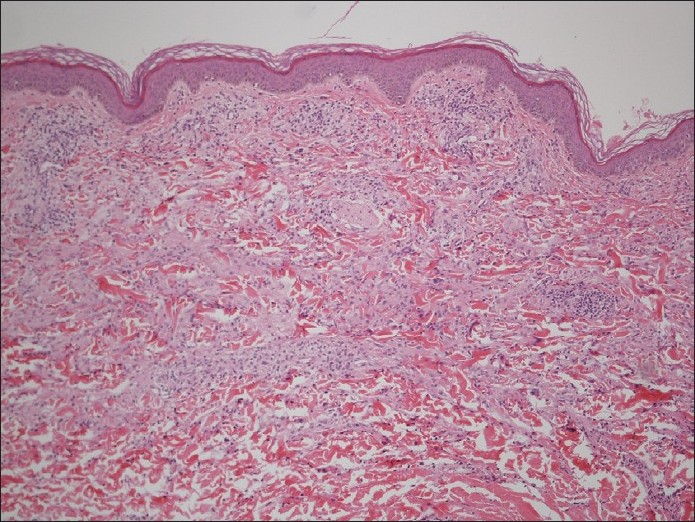 |
| Figure 2: Dense infiltrate of mononuclear cells with other scant inflammatory cells from the upper to lower dermis (H and E, ×100) |
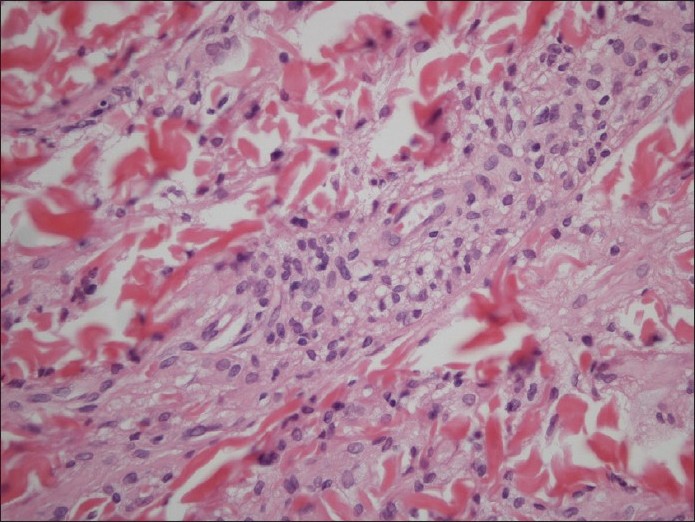 |
| Figure 3: Diffuse dermal infiltrate of foamy histiocytes (H and E, ×400) |
What is Your Diagnosis?
Diagnosis: Multiple papular xanthomas
Histopathology of the yellowish papules revealed a cellular infiltrate with foamy histiocytes from upper to lower dermis [Figure - 2] and [Figure - 3]. Infiltration of other inflammatory cells including lymphocytes or neutrophils was scant. Immunohistochemical analysis for S-100 and CD1a was negative. These histopathological features and clinical appearance were suggestive of multiple papular xanthomas (PXs).
Discussion
PX without any underlying disorder was first described by Winkelmann in 1980. [1] The diagnostic criteria in the literature include: (1) generalized asymptomatic yellowish papulonodular lesions that do not merge into plaques or involve flexural areas, (2) no visceral involvement, (3) normal lipid profile, (4) infiltrate of foamy cells with negative immunostaining for S-100 and CD1a, and (5) no primitive histiocytic phase or infiltrate of other inflammatory cells. [1],[2] Initially, all cases of PX reported were adults and the lesions did not resolve spontaneously. In 1990, Caputo et al. observed that the skin lesions in 10 children presented similar clinical and histopathologic features to those reported for adults, but with a self-healing course within 1-5 years, [3] where the healed lesions might leave transient hyperpigmentation and anetoderma-like scars. [2],[3]
Clinically, PX is manifested by asymptomatic, widespread yellowish 2-10 mm papulonodules on the head, face, extremities and trunk, with sparing of flexural areas, palms and soles, that do not show any tendency to merge into plaques. [1],[2],[3] The histological feature is a diffuse dermal infiltrate of xanthomatized histiocytes characterized by central nuclei with surrounding foamy cytoplasm with no other inflammatory cells such as lymphocytes, plasma cells or eosinophils.
The histiocytes are strongly positive for oil red O staining but are negative for S-100 and CD1a. [2],[3] Ultrastructural study reveals no Birbeck granules or laminated bodies. The results of both immunostaining and ultrastructural study indicate foamy cells of non-Langerhans histiocytic origin.
Differential diagnoses of PX include juvenile xanthogranuloma (JXG), xanthoma disseminatum (XD) and benign cephalic histiocytosis (BCH). JXG usually presents as a dome-shaped, solitary, yellowish nodule with superficial telangiectases on the head and neck. Histologically, it presents initially as a primitive intradermal collection of predominantly histiocytes progressing later to a mixed infiltrate of histiocytes, foamy cells and Touton giant cells with scattered lymphocytes, eosinophils and plasma cells. These microscopic features are quite different from PX. In XD, clinical lesions have a tendency to merge into plaques and usually involve the mucosal and flexural areas, [2] and it is frequently associated with systemic disease, the most common manifestation being diabetes insipidus. [2] The histological findings consist of histiocytes with scalloped borders in the dermis. [4] Although rare cases of XD have a dermal infiltrate of foamy cells, a mixed infiltrate of other inflammatory cells is a common characteristic. [3] BCH occurs in early childhood, and lesions are round, erythematous to brownish-yellow papules, mainly on the face. It eventually spontaneously regresses without scarring. Histologically, it is characterized by a cellular infiltrate of non-Langerhans histiocytes with abundant eosinophilic cytoplasm and vesicular nuclei in the upper dermis. However, lipidized histiocytes are absent in BCH.
PX has three clinical variants: a self-limiting form, a persistent form and a progressive form. [2] In children, PX has a limited clinical course and lesions gradually disappear in 1-5 years without treatment. Although hyperlipidemia or hypercholesterolemia is not a feature of PX, one case of abnormal lipid profiles has been reported in the literature. [5] Hence, more data may be needed to evaluate the exact relationship between PX and lipid profiles.
| 1. |
Winkelmann RK. Cutaneous syndromes of non-X histiocytosis: A review of the macrophage-histiocyte disease of the skin. Arch Dermatol 1981; 117:667-72.
[Google Scholar]
|
| 2. |
Caputo R, Passoni E, Cavicchini S. Papular xanthoma associated with angiokeratoma of Fordyce: Considerations on the nosography of this rare non-Langerhans cell histiocytoxanthomatosis. Dermatology 2003; 206:165-8.
[Google Scholar]
|
| 3. |
Caputo R, Gianni E, Imondi D, Carminati G, Gianotti R. Papular xanthoma in children. J Am Acad Dermatol 1990; 22:1052-6.
[Google Scholar]
|
| 4. |
Zelger BW, Sidoroff A, Orchard G, Cerio R. Non-Langerhans cell histiocytoses: A new unifying concept. Am J Dermatopathol 1996; 18:490-504.
[Google Scholar]
|
| 5. |
Alan Arbuckle H, Prok L. Case report: Papular xanthoma in a 10-year-old female with abnormal lipid profile. Pediatr Dermatol 2010; 27:86-8.
[Google Scholar]
|
Fulltext Views
2,948
PDF downloads
3,652





