Translate this page into:
Idiopathic eruptive macular pigmentation with papillomatosis: Report of nine cases
Correspondence Address:
Rajiv Joshi
14 Jay Mahal, A Road, Churchgate, Mumbai - 400 020
India
| How to cite this article: Joshi R. Idiopathic eruptive macular pigmentation with papillomatosis: Report of nine cases. Indian J Dermatol Venereol Leprol 2007;73:402-405 |
Abstract
Nine patients, seven males and two females aged 6-14 years, presented with extensive, asymptomatic, brown-black macules and mildly elevated, pigmented lesions of a few months' duration. The sites affected were the face, trunk and proximal extremities. The skin lesions were discrete and individual lesions were less than 2 cm in size. The clinical diagnoses rendered by the referring physicians were lichen planus pigmentosus, urticaria pigmentosa, erythema dyschromicum perstans and postinflammatory hyperpigmentation. Histology in all nine cases showed papillomatosis of the dermis with prominent pigmentation of the basal layer (pigmented papillomatosis) without any significant dermal inflammation. Two cases had spores of Pityrosporum ovale in the thickened horny layer, one of which also had, in addition, bacterial colonies in the stratum corneum. The pigmentation resolved on its own over several months. This presentation is similar to the previously described idiopathic eruptive macular pigmentation with the additional histological finding of papillomatosis that is being described for the first time and may be nosologically related to acanthosis nigricans and confluent and reticulate papillomatosis.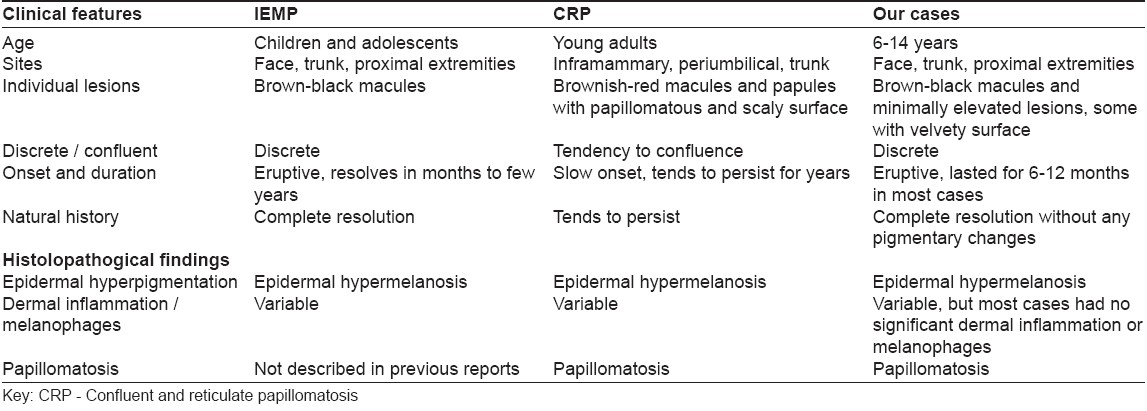
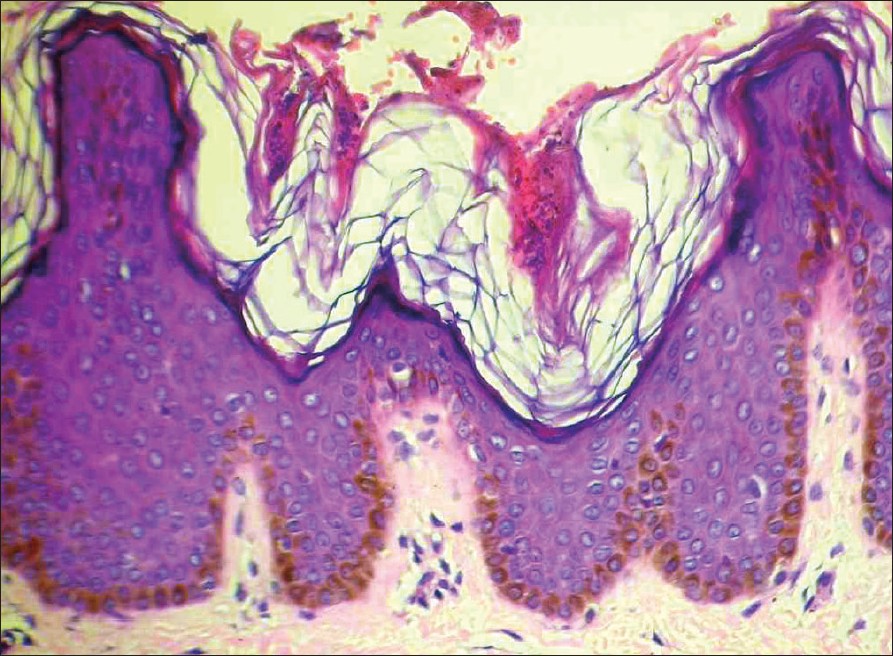 |
| Figure 3: Papillomatosis and marked hyperpigmentation of basal cell layer of epidermis (H and E stain, X200) |
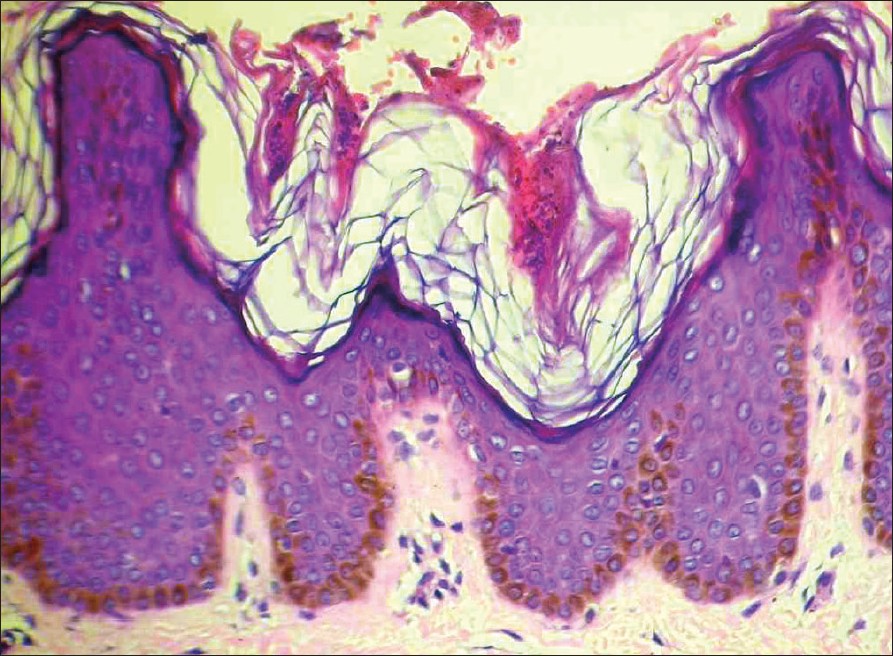 |
| Figure 3: Papillomatosis and marked hyperpigmentation of basal cell layer of epidermis (H and E stain, X200) |
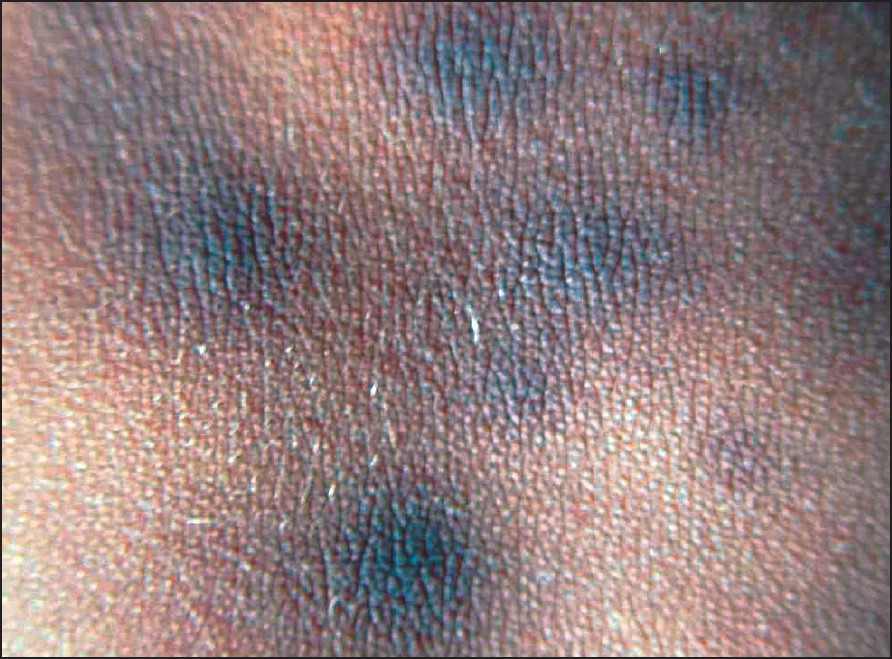 |
| Figure 2: Pigmented velvety macules on the posterior trunk |
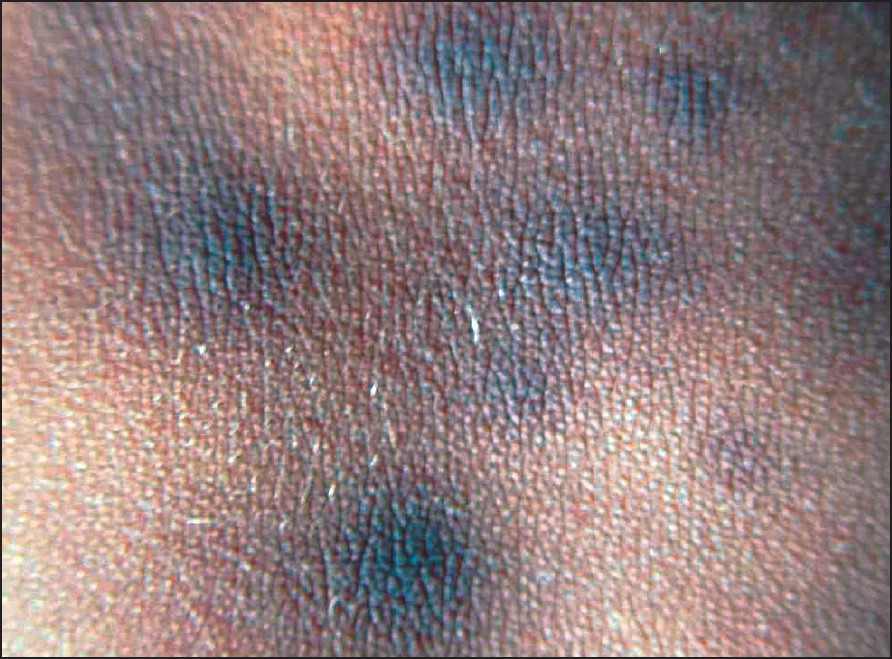 |
| Figure 2: Pigmented velvety macules on the posterior trunk |
 |
| Figure 1: Numerous pigmented macules on anterior trunk and upper limbs |
 |
| Figure 1: Numerous pigmented macules on anterior trunk and upper limbs |
Introduction
Idiopathic eruptive macular pigmentation (IEMP) is an uncommon condition characterized by the presence of asymptomatic pigmented macules that involve the face, trunk and proximal extremities in children and adolescents. These dark brown and brown-black macules occur in crops and gradually resolve over months or years without any residual pigmentation or scarring. There have been a total of 25 published cases of this disorder. The first description was by Degos et al. in 1978 [1] in French while the first description in English was by Sanz de Galdeano et al. in 1996. [2] That paper summarized the criteria for diagnosis of this condition, namely, (1) Eruption of brownish-black, discrete, nonconfluent, asymptomatic macules involving the neck, trunk and proximal extremities in children and adolescents, (2) Absence of any preceding inflammatory lesions, (3) No previous drug exposure, (4) Basal layer hyperpigmentation of the epidermis with dermal melanophages without any basal cell damage or lichenoid infiltrate, (5) Normal mast cell counts. The largest series of ten cases has been described by Jang et al. from Korea. [3]
In this report, nine Indian cases are being described that clinically fulfilled all the criteria for this entity. Additionally, a few lesions had velvety surfaces, reminiscent of acanthosis nigricans with prominent papillomatosis of the dermis and marked basal cell pigmentation without any significant dermal inflammation. These findings have not been described in any of the previously published cases. The histolopathogical picture described in these cases is similar to acanthosis nigricans and it is speculated that IEMP may be an eruptive variant of acanthosis nigricans. Nine such Indian cases are described here.
Case Reports
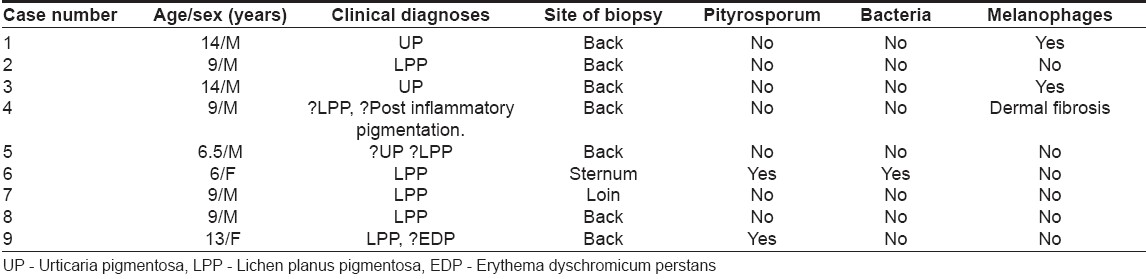
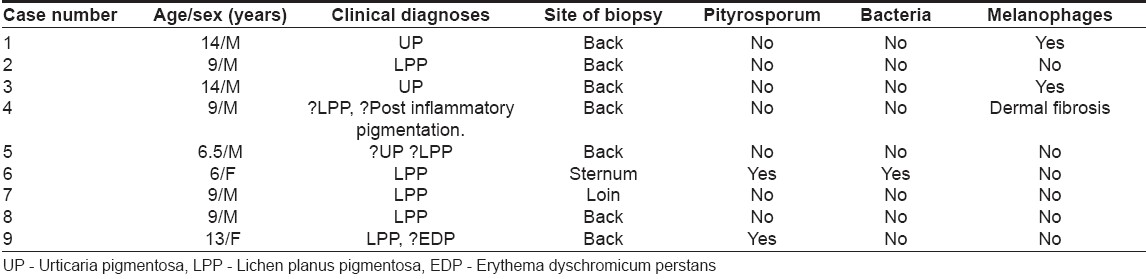
The details of all the nine cases are summarized in [Table - 1]. The patients were in the 6-14 years′ age group and comprised seven boys and two girls. All presented in an almost identical manner with an eruption of numerous dark brown and brown-black macules and barely elevated lesions on the face, anterior and posterior trunk and extremities [Figure - 1]. These pigmented lesions were asymptomatic, without any pruritus and were not preceded by any other skin lesions. No drug ingestion was documented in any of the cases. The lesions had been present for a few months before presentation, progressively increasing in number and size, although no individual lesion was more than 2-3 cm in diameter. There was no scaling seen on the surface and Darier′s sign was negative in all patients. Some of the lesions especially the older ones, showed on closer examination, a velvety surface similar to that seen in acanthosis nigricans [Figure - 2]. All patients were in good health, not obese and no patient had any evidence of acanthosis nigricans elsewhere on the body. The clinical diagnosis of these patients was varied and the most common diagnosis considered by the referring physician was lichen planus pigmentosus (6), followed by urticaria pigmentosa (3), erythema dyschromium perstans (1) and postinflammatory hyperpigmentation (1). Two patients had more than one diagnosis.
Biopsy was taken from the back in seven cases, the loin in one and the sternal region in one patient. All cases showed similar histological findings of prominent papillomatosis of the dermis with elongated dermal papillae and a thickened basket-weave orthokeratotic, stratum corneum that filled the dells adjacent to the elongated papillae. The basal layer of the epidermis had very prominently increased melanin without any increase in the number of melanocytes at the dermo-epidermal junction [Figure - 3]. Spores of Pityrosporum were seen in the thickened horny layer in case nos. 6 and 9 and case 6 also had several colonies of coryneform bacteria in the stratum corneum. The dermis had a very sparse perivascular lymphocytic infiltrate. A few melanophages were seen in case nos. 1 and 3 and mild upper dermal fibrosis was seen in case no. 4. The overall histological picture resembled that of acanthosis nigricans.
Patients were treated with topical steroids but continued to get new lesions for several months. Lesions started subsiding on their own after 6-8 months and gradually cleared completely. Most patients were lost to follow-up once the lesions started clearing, but case no. 1 was seen recently by the author after five years and had complete clearing of all lesions without any residual pigmentation or scarring.
Discussion
Idiopathic eruptive macular pigmentation (IEMP) is a benign, self-limiting melanosis that occurs in children and adolescents. The oldest patient described so far was a 24 year-old woman of Indian origin who had had the condition for 21 years, with two periods of spontaneous complete remission at age 11 years (onset of puberty) and again at 13 years with recurrence. [4] This case seems to be unusual in that the lesions persisted for so long and recurred after two remissions. All other cases described so far, including the present cases, had spontaneous remission of lesions within months to years with no further recurrences.
Idiopathic eruptive macular pigmentation may be difficult to differentiate clinically from urticaria pigmentosa and lichen planus pigmentosus as all three conditions present with numerous, discrete, pigmented macules on the trunk and proximal extremities. A positive Darier′s sign may be elicited in urticaria pigmentosa and is of help to differentiate it from IEMP, however, diagnosis may be difficult on clinical grounds alone.
On biopsy, IEMP can be differentiated from other conditions that are commonly considered in the differential diagnoses, namely, urticaria pigmentosa, lichen planus pigmentosus and erythema dyschromicum perstans. Urticaria pigmentosa, like IEMP, has prominent pigmentation of the basal layer of the epidermis but has in addition, numerous mast cells in the upper dermis that are diagnostic.
Both lichen planus pigmentosus and erythema dyschromicum perstans are interface dermatitides that show basal cell vacuolization with individually necrotic keratinocytes at the dermo-epidermal junction with numerous melanophages scattered in a variably thickened papillary dermis.
Histopathologically, IEMP is an epidermal hypermelanosis with increased melanin in the basal layer of the epidermis and variable dermal inflammation and melanophages in the dermis. However, as these findings in IEMP are not specific, biopsy is important in the diagnosis of idiopathic eruptive macular pigmentation to exclude the other conditions, which clinically resemble it.
The apparent rarity of this condition is probably due to physicians not being familiar with this entity. Reluctance to biopsy children may be another factor that leads to underreporting of this condition.
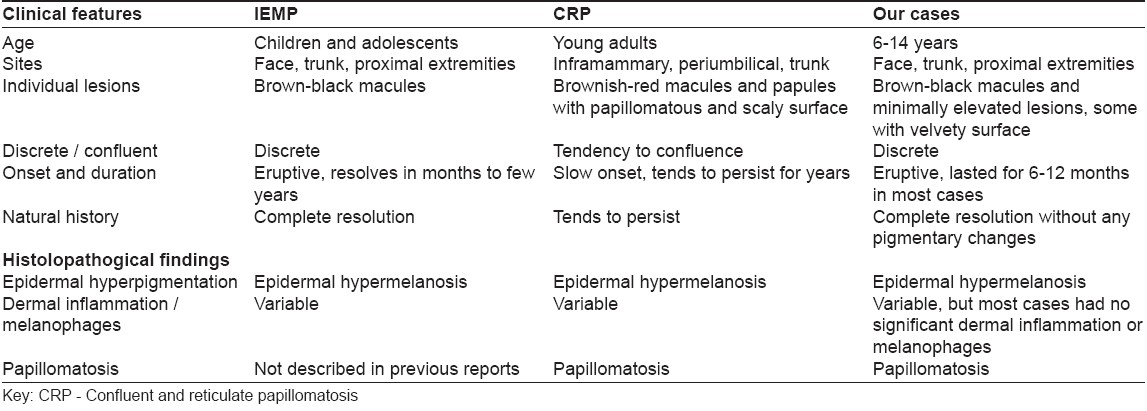
All our cases fulfill the criteria described by Galdeano et al. [2] and are consistent with idiopathic eruptive macular pigmentation. Histologically, IEMP as described by Galdeano et al. and us are primarily epidermal hypermelanotic conditions. An additional finding in our cases is papillomatosis, which has not been described before. Only clinical photographs appear in all the other reports on IEMP. No photomicrographs have been published and it is not possible for the reader to independently assess the true histological picture. On the other hand, our cases were grouped together based on the common, repetitive histological findings. These findings included pigmented papillomatosis in all cases, with no features of either lichen planus pigmentosus or urticaria pigmentosa (the clinical diagnoses most often rendered by the referring clinicians). On clinico-pathological correlation, these findings were found to have clinical presentations that satisfied all criteria of IEMP. Therefore, because our cases satisfy the diagnostic criteria previously alluded to, these cases are IEMP with the additional finding of papillomatosis.
It is possible that this condition may be related nosologically to confluent and reticulate papillomatosis (CRP) and acanthosis nigricans because both these conditions show histological findings similar to our cases, namely, pigmented papillomatosis [Table - 2]. In addition, two of our cases (nos. 6 and 9) had Pityrosporum in the horny layer. Pityrosporum has been incriminated in the pathogenesis of CRP where it is postulated that microorganisms may trigger an abnormal epidermal response. [5]
However, on clinical grounds, the eruption in these patients is akin to IEMP and not CRP. In CRP, [5] the lesions begin in the intermammary region as punctate verrucous pigmented papules which may become generalized over the trunk. There may be associated itching and discomfort. At times, there are pale red macules and papules, reticulation, isolated circinate disks and confluent, brownish papillomatous surfaces. The changes show the greatest intensity between the breasts and around the umbilicus. [5] The eruption tends to show confluence and scaling and persists for long periods of time usually several years. Also the age group affected is that of young adults and not children and adolescents as seen in our cases and in other published cases of IEMP. Therefore, while histologically similar to CRP, our cases based on clinico-pathological findings match IEMP the best, albeit with the additional, finding of papillomatosis.
The pathogenesis of IEMP is not known and it is possible that hormonal factors may play a role as the condition is seen in the peripubertal age group. Pigmented papillomatosis is a histological term that succinctly describes the findings seen in our cases. Whether IEMP is always associated with pigmented papillomatosis needs to be confirmed with additional reports.
This report presents nine children with clinical presentations which fit best into idiopathic eruptive macular pigmentation, albeit with histological findings of pigmented papillomatosis, which correspond better to confluent and reticulate papillomatosis and acanthosis nigricans. It is tempting to speculate that cutaneous papillomatosis with prominent basal pigmentation (pigmented papillomatosis) is a common histological finding in IEMP and CRP and that both these are clinical variants of the primary condition, namely, acanthosis nigricans.
| 1. |
Degos R, Civatte J, Belaich S. Idiopathic eruptive macular pigmentation. Ann Dermatol Venereol 1978;105:177-82.
[Google Scholar]
|
| 2. |
Sanz de Galdeano C, Lιautι-Labrθze C, Bioulac-Sage P, Nikolic M, Taοeb A. Idiopathic eruptive macular pigmentation: Report of five patients. Pediatr Dermatol 1996;13:274-7.
[Google Scholar]
|
| 3. |
Jang KA, Choi JH, Sung KS, Moon KC, Koh JK. Idiopathic eruptive macular pigmentation: Report of 10 cases. J Am Acad Dermatol 2001;44:351-3.
[Google Scholar]
|
| 4. |
Mehta S, Aasi S, Cole R, Chu P, Weinberg JM. Idiopathic eruptive macular pigmentation: A case of 21 year's duration. J Am Acad Dermatol 2003;49:S280-2.
[Google Scholar]
|
| 5. |
Arnold HL, Odom RB, James WD. In : Andrew's Diseases of the skin. 8 th ed. Philadelphia: WB Saunders Company; 1990. p. 350.
th ed. Philadelphia: WB Saunders Company; 1990. p. 350.'>[Google Scholar]
|
Fulltext Views
5,266
PDF downloads
2,654





