Translate this page into:
Epidermal skin grafts from the scalp for hyperkeratosis of nipple and areola
Corresponding author: Dr. Muzhang Xiao, 1688# Moon Avenue, Changde, Hunan 415000, China. 120740851@qq.com
-
Received: ,
Accepted: ,
How to cite this article: Li L, Xiao M, Huang X, Jin H. Epidermal skin grafts from the scalp for hyperkeratosis of nipple and areola. Indian J Dermatol Venereol Leprol 2022;88:228-9.
Sir,
The literature points out that hyperkeratosis of the nipple and areola was first described by Tauber in 1923. Just over 100 cases have been reported globally in the past 100 years.1 The primary treatment, topical keratolytic medication, has a positive effect, but almost all cases recur after discontinuing medication. There are occasional reports of surgical resection with relatively positive outcomes. However, the use of scalp tissue for skin grafting has not been reported. We herein report a case of bilateral hyperkeratosis of the nipple and areola treated by surgical resection and epidermal skin grafting from the scalp.
A 20-year-old lady presented to the outpatient clinic with asymptomatic hyperpigmented and thickened skin lesions on her nipples and areolas which had been present for two years. Examination revealed hyperpigmented verrucous plaques on the bilateral areolas and nipples [Figure 1]. Routine investigations were within normal limits. A biopsy from the lesion showed hyperkeratosis without any signs of fungal infection. Our patient opted for a surgical treatment. During the surgery, the verrucous plaques on the areolas and the edges of the nipples were resected from the superficial dermis and only the parts of the nipples without obvious hyperkeratosis were preserved. Epidermal graft was harvested from the scalp. The grafts were then transplanted onto the areolas. Pathological examination of the resected lesions confirmed hyperkeratosis of the nipple and areola [Figure 2]. Examination after seven days proved that the epidermal skin grafts had survived. A follow-up after six months revealed areolas with good cosmetic appearance without obvious scars or disease recurrence [Figure 3].
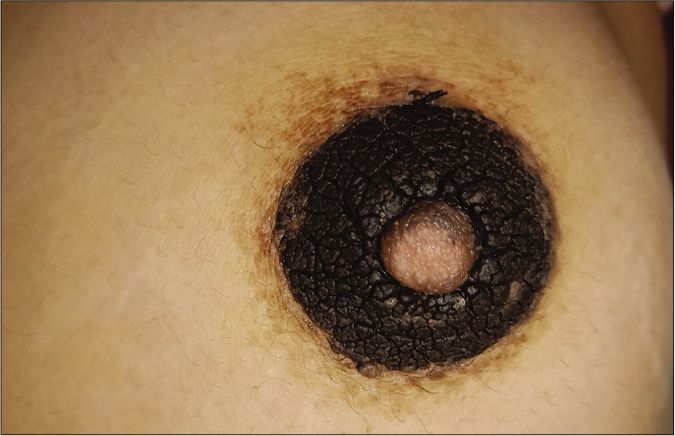
- Hyperpigmented verrucous plaque on areola and nipple
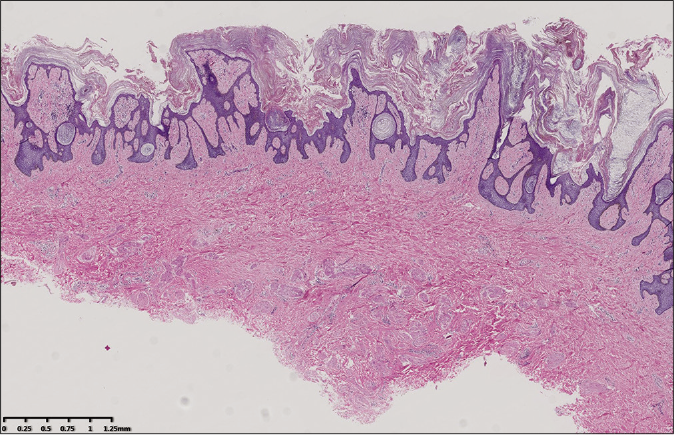
- Hyperkeratosis in the resected area (haematoxylin and eosin, ×20)

- Follow-up at six months shows a natural appearance without obvious scars or disease recurrence
Hyperkeratosis of the nipple and areola is a rare skin disease. The typical pathological features are persistent verrucous thickening and dark brown pigmentation of the nipples and areolas, without induration or oozing. The aetiology of naevoid hyperkeratosis of the nipple and areola is unclear. According to the research by Obayashi et al., 80% of cases are women aged 20–40 years. It occurs bilaterally and affects the nipples and areolas in more than 70% of the cases.2 However, it has been reported that it may not only appear in females during puberty or pregnancy but also in males using diethylstilbestrol for prostate cancer treatment or as a result of hormonal disorders.3 Others have pointed out that hyperkeratosis of the nipple and areola may be a secondary symptom of malignant acanthosis nigricans.4 Li et al. reported that Malassezia may be a factor leading to hyperkeratosis of the nipple, but it is not clear whether it is the direct cause of the disease.5 Levy-Frankel classification has been widely used for hyperkeratosis of the nipple and areola. Type 1 hyperkeratosis is an extension of an epidermal nevus. Type 2 hyperkeratosis is associated with other dermatoses, such as acanthosis nigricans, ichthyosis, lymphoma or Darier disease and Type 3 is idiopathic or naevoid hyperkeratosis. This case was classified as Type 3.1
At present, there is no unified and effective treatment for hyperkeratosis of the nipple and areola. Drug therapies alone have great differences in effect and disease recurrence has been reported after discontinuation of most of these drugs.6 Cryotherapy, radiofrequency ablation and fractional laser have been reported to have good results in individual cases. However, the recovery time may be long and the depth of treatment is difficult to control. If the treatment scope is too shallow the disease can easily relapse, while if the treatment scope is too deep it can lead to scars.7 Surgical treatment including scraping and surgical resection is occasionally reported in the literature.8 We believe that scraping alone does not completely remove the lesions and the disease can easily recur. As the lesions of hyperkeratosis of the nipple and areola are very superficial it is enough to excise the lesions only from the superficial dermis. Skin grafts only aimed to speed up wound healing. As preferred by the patient, we transplanted epidermal skin grafts from the scalp which did not cause further damage to the donor site and could also preserve the texture of the affected areas. This method resulted in a quick recovery and provided a better natural appearance.
Acknowledgment
We would like to thank Editage (www.editage.com) for English language editing and publication support.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Special fund project for science and technology innovation and development of Changde Science and Technology Bureau (2019s226).
Conflicts of interest
There are no conflicts of interest.
References
- Bilateral hyperkeratosis of the nipples and areolae with linear nevus: A rare case report and review of the literature. Postgrad Med. 2018;130:361-4.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperkeratosis of the nipple and areola as a sign of malignant acanthosis nigricans. Clin Exp Dermatol. 2005;30:721-2.
- [CrossRef] [PubMed] [Google Scholar]
- Malassezia associated hyperkeratosis of the nipple in young females: Report of three cases. Indian J Dermatol Venereol Leprol. 2014;80:78-80.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of nevoid hyperkeratosis of the areola and nipple with topical tacalcitol: A case report. Dermatol Ther. 2018;31:e12602.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral nevoid/primary hyperkeratosis of nipple and areola successfully treated with radiofrequency ablation. J Cutan Aesthet Surg. 2011;4:214-5.
- [CrossRef] [PubMed] [Google Scholar]
- Focal nevoid hyperkeratosis of the nipple in a prepubertal girl. Pediatr Dermatol. 2019;36:247-8.
- [CrossRef] [PubMed] [Google Scholar]





