Translate this page into:
A retrospective study of the clinical and imaging features of 60 cases of odontogenic cutaneous fistula
Corresponding author: Dr. Guan Jiang, Department of Dermatology, Affiliated Hospital of Xuzhou Medical University, Xuzhou, Jiangsu, China. dr.guanjiang@xzhmu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Xia J, Tang H, Jiang G. A retrospective study of the clinical and imaging features of 60 cases of odontogenic cutaneous fistula. Indian J Dermatol Venereol Leprol. 2024;90:777-81. doi: 10.25259/IJDVL_1059_2023
Abstract
Background
Odontogenic cutaneous fistulas (OCST) are pathological connections between the facial skin and oral cavity caused by chronic dental infection. They are often misdiagnosed or underdiagnosed by dermatologists.
Aims
This study explores the clinical and radiographic features of patients with odontogenic cutaneous fistulas.
Methods
This study retrospectively analysed the clinical data of 60 patients diagnosed with odontogenic cutaneous fistulas between January 2016 and February 2022.
Results
The study identified a predominance of OCST in males (53.3%) with a mean age of 49 years. There was a significant difference in the distribution between the maxillary and mandibular zones [(14/60, 23.3%) vs (46/60, 76.7%), p < 0.001]. Nodules are the most frequent morphology (48.3%). Imaging findings included periapical radiolucency, bone erosion and the presence of a sinus tract. All patients responded well to dental treatments with no recurrences noted.
Limitations
This is a retrospective study design and has a limited number of patients.
Conclusion
Collaborative efforts between dentists and dermatologists are crucial for accurate diagnosis and treatment, enhancing patient outcomes.
Keywords
Odontogenic infection
Cutaneous
Fistula
Tooth
Introduction
Odontogenic cutaneous fistulas (OCST) are challenging to diagnose in dermatology due to their deceptive clinical manifestations. These conditions, primarily stemming from dental infections, create an abnormal conduit that connects the facial skin to the oral cavity which often results in misdiagnosis or underdiagnosis. This study aims to highlight the clinical and radiographic features of OCST to improve recognition and treatment.
Methods
We retrospectively reviewed 60 cases of OCST at the Affiliated Hospital of Xuzhou Medical University from January 2016 to February 2022. Data on demographics, lesion characteristics, diagnostic imaging and treatment outcomes were collected and analysed. Once suspected, all patients were referred to the stomatology department for confirmation and necessary treatment. SPSS 26.0 was used for statistical processing. Categorical variables were compared by using Pearson’s χ2 test or Fisher’s exact test, p < 0.05 was considered statistically significant.
Results
Patient demographics and clinical presentation: Among the 60 patients, there was a slight male predominance (53.3%) with ages spanning from 8 to 79 years [Table 1]. Dermatological assessment revealed that the most common manifestation of OCST was persistent orofacial swelling. Notably, 50% (n=30) of the patients reported pain associated with the affected area and 30% (n=18) experienced purulent discharge through cutaneous sinus tracts.
| Number of patients | |
|---|---|
| Gender (Male/Female) | 32/28 |
| Age (years) | |
| 0–18 | 5 |
| 19–40 | 18 |
| 41–60 | 23 |
| >60 | 14 |
| Site of the sinus tract | |
| Chin | 15 |
| Cheek | 12 |
| Mandibular area | 21 |
| Neck | 1 |
| Nasal region | 10 |
| Infraorbital region | 1 |
| Origin (maxillary, mandibular) | |
| Incisor | 0, 9 |
| Canine | 11, 5 |
| Molar | 3, 17 |
| Premolar | 0, 9 |
| Wisdom teeth | 0, 6 |
| Morphology | |
| Nodular type | 29 |
| Cyst type | 6 |
| Fistula type | 7 |
| Ulcer type | 8 |
| Scar type | 10 |
| Examination | |
| Panoramic radiograph | 31 |
| Cone beam computed tomography | 36 |
| Ultrasonography | 2 |
| Final treatment | |
| Extraction | 14 |
| Extraction + fistula removal (or curettage) | 4 |
| Root canal therapy | 36 |
| Root canal therapy + fistula removal (or curettage) | 6 |
| Duration of illness | |
| <6 months | 47 |
| ≥6 months | 13 |
Lesion Characteristics: Lesion characteristics varied with nodules being the most common presentation (48.3%) [Figures 1a and 1b]. Other manifestations included scarred [Figure 1c], ulcerated [Figures 1d and 1e], fistular and cystic lesions. Lesion diameters ranged from 5 mm to 30 mm. The statistical analysis revealed a significant difference in the distribution of affected teeth between the maxillary and mandibular zones [(14/60, 23.3%) vs (46/60, 76.7%), p < 0.001], with the mandibular area being the most common location (35.0%), mandibular molars showing most frequent involvement. The nasal region and chin are more affected in patients aged over 40 years. In patients aged 60 years and above, the nasal region emerged as the most common site of OCST (11.7%) [Figure 2]. Disease duration before seeking medical advice varied significantly, from several weeks to 19 years, averaging 12.9 months.

- Clinical photographs showing the nodular morphology of an odontogenic dermatological fistula.

- Nodular morphology of an odontogenic dermatological fistula.

- Scarred morphology of an odontogenic fistula.

- Ulcerated morphology of an odontogenic fistula.

- Ulcerated morphology of an odontogenic fistula, can be misdiagnosed as pyogenic granuloma.
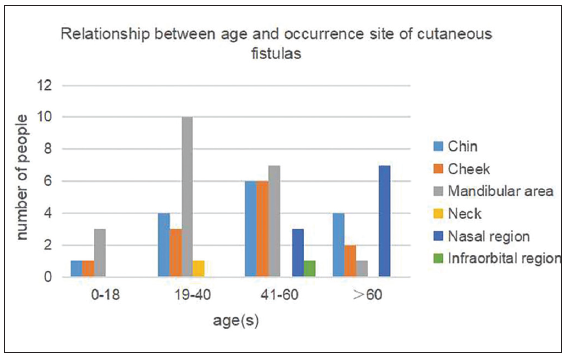
- Relationship between age and occurrence site of cutaneous fistulas.
The aetiology of OCST in 60 patients was mainly caries and trauma. The aetiology of the adolescent patients was dental caries. The aetiology of the adult patients was more complex than that of other patients with caries, trauma and pericoronitis being the most common causes [Figure 3].
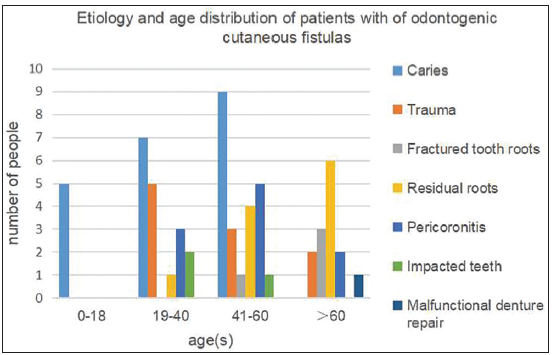
- Aetiology and age distribution of patients with of odontogenic cutaneous fistulas.
Diagnostic Imaging: Panoramic radiography [Figure 4a], used in 31 patients (51.7%), provided an initial overview of dental structures and potential infection sources, revealing hypodense shadows in the apical regions in some cases. Cone Beam Computed Tomography (CBCT) [Figures 4b–4d] (n=36) was instrumental in delineating the depth and trajectory of the sinus tracts, revealing bone erosion in the patients. In addition, colour Doppler ultrasound, utilised in two cases, revealed hyperechoic areas with irregular margins extending from the skin nodules to the subcutaneous tissue, including a blood flow signal, providing valuable insights into vascular involvement and inflammation around the fistulas.
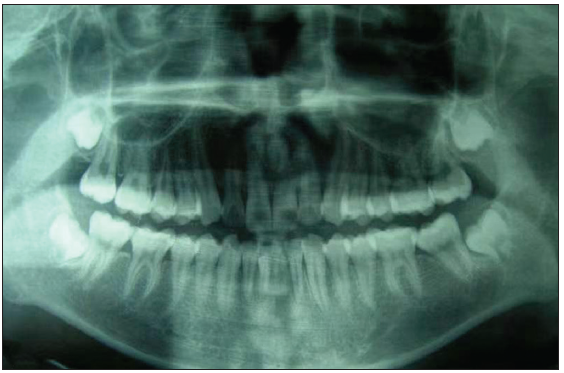
- Panoramic radiographs of patient in Figure 1c showed hypodense shadows in the left mandibular central incisor apical region.
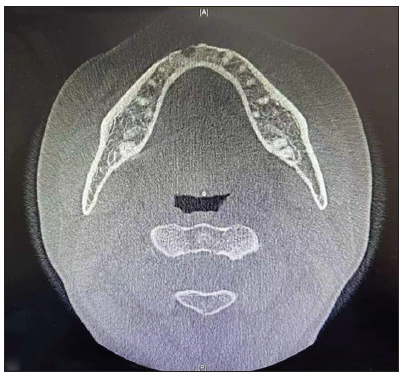
- CBCT scan with an axial view of the patient (1a).
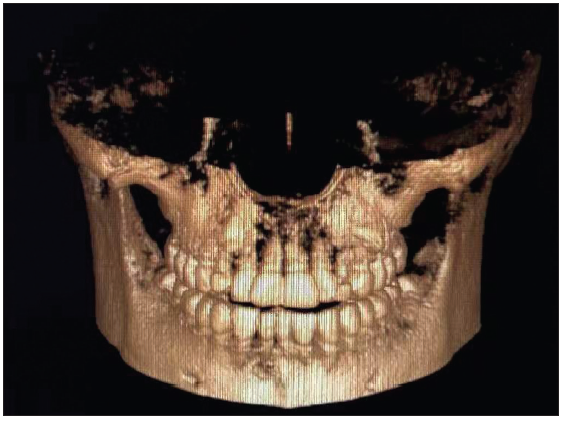
- 3D reconstruction of a fistula under the right lower central incisor of the patient (1a).
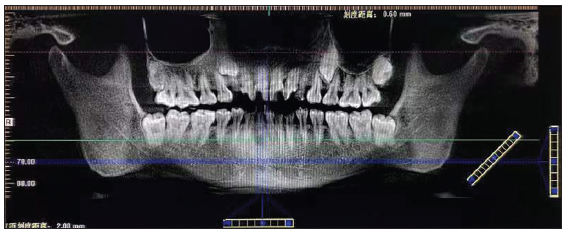
- CBCT scan with a panoramic view of the patient (1a).
Differential diagnosis: The initial misdiagnosis among dermatologists may be attributed to the variable cutaneous presentation of OCST. In this study, 78.3% of patients initially seeking treatment within 6 months of fistula discovery, received diagnoses such as pyogenic granuloma [Figure 1e], epidermoid cyst and invasive fungal infections leading to ineffective treatments such as surgical excision, laser therapy and antifungal medication, only to see a recurrence of symptoms within months.
Upon correct diagnosis, all patients underwent dental treatment, predominantly tooth extraction or root canal therapy with no recurrences noted. Notably, patients with nodular odontogenic fistulas exhibited better healing and less scar formation. Patients treated within 6 months of diagnosis generally experienced better prognoses. Our clinical experience showed that patients who delay seeking medical attention for their skin fistulas and those who have undergone previous excisions, drainages or laser surgeries at the same site are more susceptible to developing scars than other patients. However, this conclusion is based solely on our observations.
Discussion
Our investigation elucidated the aetiological diversity of OCST with dental caries and trauma being pinpointed as the predominant causative factors, aligning with the outcomes of preceding research.1 A significant variation in causative factors was observed across various age demographics. This aetiological diversity calls for a multifaceted approach to prevention, diagnosis and treatment, tailored to the patient’s age and dental history.
We also observed that OCST predominantly occurs in the mandibular area, particularly the molars, as corroborated by other literature.2 A diversity of lesions was observed in our study, predominantly nodules, but also scars, ulcers, fistulae and cystic lesions, with or without pain and purulence. These findings are significant, especially for dermatologists who first encounter these patients, to consider OCST in their differential diagnoses, when faced with such lesions.
The high rate of initial misdiagnosis, particularly among dermatologists, highlights a significant gap in the current diagnostic approach to cutaneous presentations of OCST. It underscores the importance of incorporating detailed dental history and examination into the evaluation of patients presenting with cutaneous orofacial lesions, to avoid unnecessary treatment and ensure timely and appropriate intervention.
Accurate diagnosis is crucial and involves methods like endodontic sensitivity tests, tracing with gutta-percha points and radiological imaging.3-5 Our findings reinforce the pivotal role of imaging, particularly panoramic radiography and CBCT, in diagnosing OCST. These imaging modalities not only facilitate the identification of underlying dental pathologies but also assist in the accurate mapping of sinus tracts, crucial for effective treatment planning. The utility of colour Doppler ultrasound in revealing vascular and inflammatory involvement offers an additional diagnostic tool that could enhance the understanding of OCST’s pathophysiology.
The marked improvement in patients following accurate diagnosis and dental treatment with no recurrences noted, underscores the effectiveness of these interventions. Notably, the correlation between treatment timing and outcomes accentuates the importance of early diagnosis and intervention in achieving favourable prognoses. Our clinical observations suggest that delayed treatment and prior ineffective interventions contribute to scar formation, emphasising the need for prompt and accurate diagnosis.
Limitations
Reliance on historical medical records and imaging data introduces potential biases. The retrospective nature as well as the single-centre design may constrain the generalisability of our findings. Future research should aim to address these limitations through prospective study designs, multicentre collaborations and the inclusion of patient-reported outcome measures.
Conclusion
This study highlights the critical challenges in diagnosing and managing OCST, underscoring the necessity for heightened awareness among dermatologists regarding the odontogenic origins of certain cutaneous orofacial lesions. The findings advocate for an integrated, multidisciplinary approach to patient care, emphasising on the importance of early and accurate diagnosis to optimise treatment outcomes.
Acknowledgements
Thanks to Dr. Zhongjing Lü from the Department of Stomatology at the Affiliated Hospital of Xuzhou Medical University for his technical guidance.
Ethical approval
The research/study was approved by the Institutional Review Board at the Ethics Committee of the Affiliated Hospital of Xuzhou Medical University, number XYFY2022-KL455-01, dated 2023.1.6.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Problems with diagnosis and treatment of an odontogenic fistula of facial skin. Pol Merkur Lekarski. 1997;2:120-1.
- [PubMed] [Google Scholar]
- Clinical characteristics of odontogenic cutaneous fistulas. Ann Dermatol. 2016;28:417-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Odontogenic cutaneous fistulas: clinical and epidemiologic characteristics of 75 cases. Int J Dermatol. 2015;54:50-5.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of odontogenic cutaneous sinus tracts of endodontic origin: Three case studies. Int Endod J. 2009;42:271-6.
- [CrossRef] [PubMed] [Google Scholar]
- Management of extraoral sinus cases: A clinical dilemma. J Endod. 2004;30:541-7.
- [CrossRef] [PubMed] [Google Scholar]






