Translate this page into:
A case of multiple eruptive dermatofibromas in a Chinese man with chronic inactive hepatitis B infection
Correspondence Address:
Conghui Li
No. 165 of Caoshi Street, Department of Dermatology, Chengdu Second People's Hospital, Chengdu 610000, Sichuan
China
| How to cite this article: Li C, Wang W, Zhang L, Xu L. A case of multiple eruptive dermatofibromas in a Chinese man with chronic inactive hepatitis B infection. Indian J Dermatol Venereol Leprol 2020;86:72-75 |
Sir,
We report the case of multiple eruptive dermatofibromas in a Chinese man with chronic inactive hepatitis B infection. We were unable to find any previous reports of such association.
A 35-year-old man presented for evaluation of multiple asymptomatic lesions on his trunk, which appeared within a period of approximately 6 months [Figure - 1]a, [Figure - 1]b, [Figure - 1]c. On physical examination, more than 100 reddish-brown papules were observed on his trunk, mainly on the chest. They ranged in size from 2 to 10 mm, were symmetrical, firm, reddish-brown, nonconfluent and remained stable over time. No lesions were found on the head, limbs or mucous membranes. There was no regional lymphadenopathy. The patient had no antecedent trauma. He was in good health previously, and both medical history and family history were unremarkable.
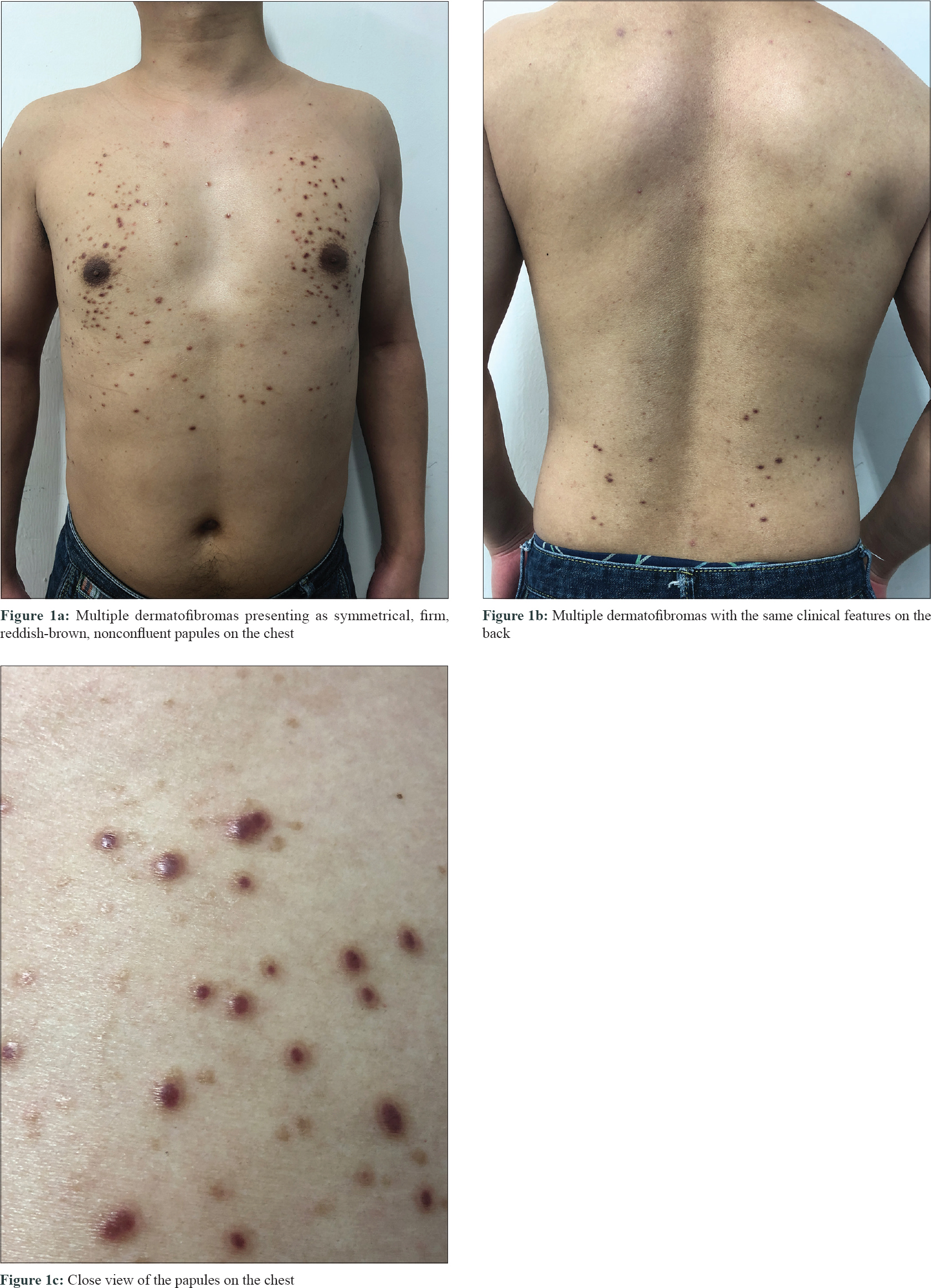 |
| Figure 1: |
Dermoscopy of a representative lesion showed a central reddish-brown patch with peripheral light brown network. In some lesions linear or arborizing telangiectasia were seen, and in some, both the features were noted [Figure - 2]a, [Figure - 2]b. Histopathological examination of a representative lesion revealed a fibrous spindle-cell proliferation in the dermis with a swirling storiform appearance and the periphery had entrapment of dermal collagen fibers [Figure - 3]. The diagnosis of multiple eruptive dermatofibromas was made, based on the clinical manifestation and dermatoscopic findings, along with histopathological confirmation.
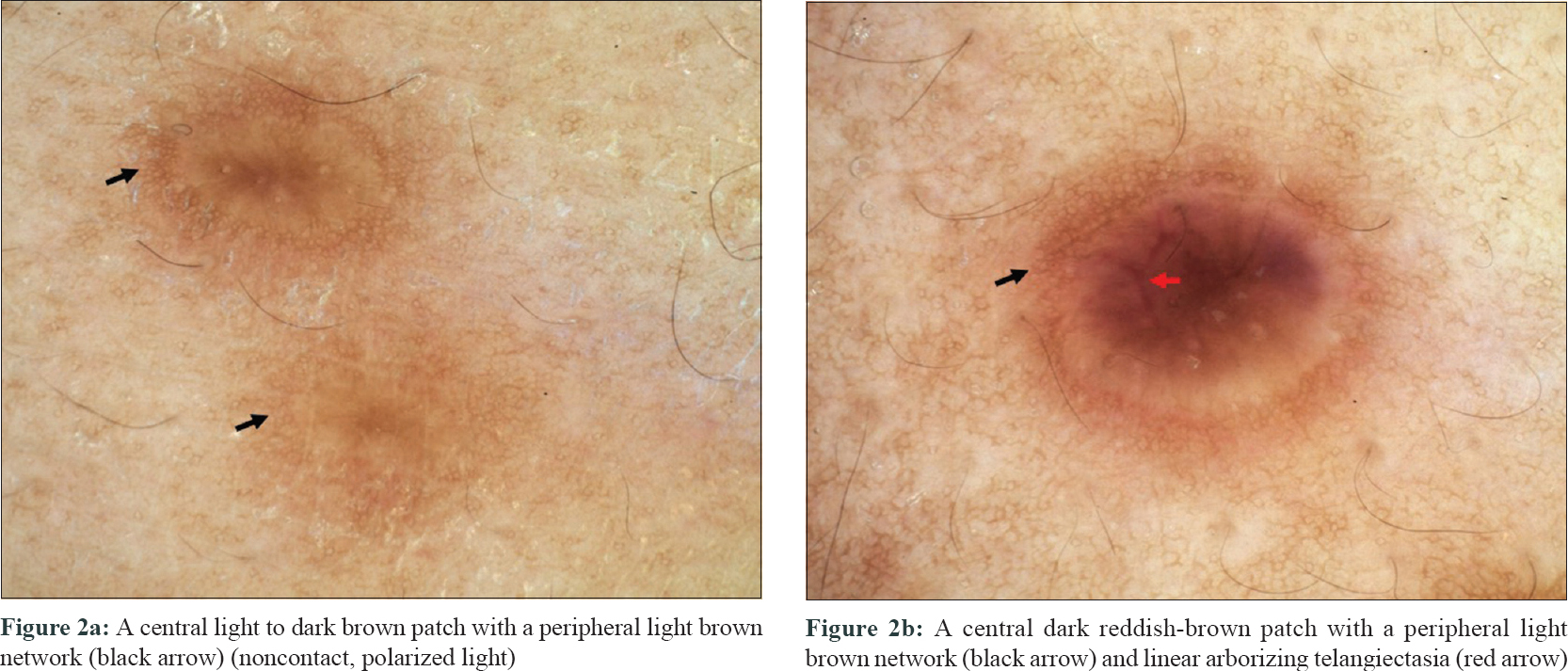 |
| Figure 2: |
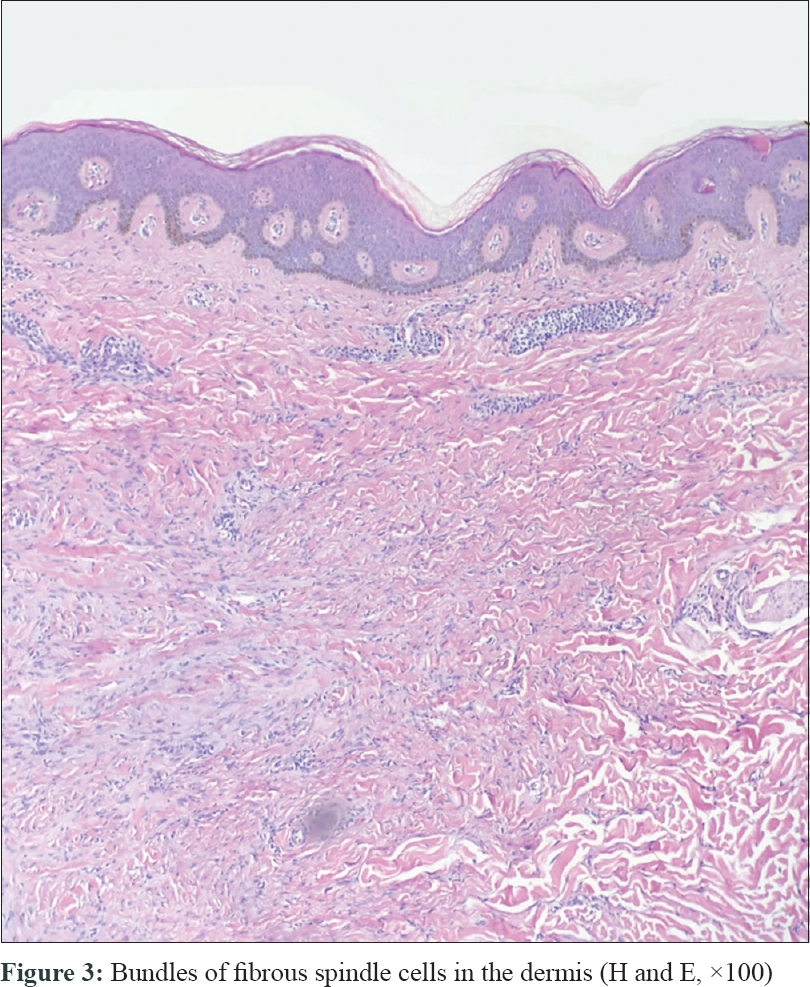 |
| Figure 3: Bundles of fibrous spindle cells in the dermis (H and E, ×100) |
Laboratory tests showed a raised triglycerides level (1.91 mmol/L; normal range 0.4–1.73 mmol/L); ultrasonography showed densely enhanced liver parenchyma echo; and further investigation revealed that HBsAg, HBcAb, and HBeAb were positive. HBV-DNA level was less than 1000 IU/ml. Other laboratory investigations including full blood count, liver function tests, renal function tests and blood glucose were normal. Lymphocyte subgroup detection revealed decreased CD3 + T cell count (456.00; normal range 770.00–2860.00), CD4 + T cell count (308.00; normal range 500.00–1440.00), CD8 + T cell count (116.00; normal range 238.00–1250.00), and a raised CD4/CD8 ratio (2.66; normal range 1.00–2.47).
No other abnormal laboratory results were noted, including human immunodeficiency virus test and autoimmunity tests such as antinuclear antibody, antihepatocyte membrane antibody, antismooth muscle antibody, antiliver and kidney microsomal antibody, antisoluble liver antigen, antimitochondrial antibody and antimitochondrial antibody M2. As the patient recounted no other remarkable symptoms, he was diagnosed as chronic inactive hepatitis B infection and hypertriglyceridemia based on the laboratory examination. The patient was recommended for follow-up every 3 months with no active treatment.
Dermatofibroma is a benign cutaneous lesion which generally occurs as a solitary reddish-brown or dark-brown firm papule or nodule on lower legs in middle-aged individuals with a slight female preponderance. However, multiple eruptive dermatofibromas is a rare skin condition, defined as presence of more than 15 lesions or 5-8 dermatofibromas that appear within a period of 4 months.[1] Less than 100 cases of multiple eruptive dermatofibromas have been reported in the literature, and it is usually associated with autoimmune diseases and immunosuppression.[2]
The presence of multiple eruptive dermatofibromas is frequently associated with systemic lupus erythematosus or, less commonly, other autoimmune diseases, such as myasthenia gravis, pemphigus vulgaris, ulcerative colitis, sarcoidosis and Graves' disease.[2],[3],[4] The association of multiple eruptive dermatofibromas with hepatitis B infection has not been described previously. The pathogenesis of dermatofibroma is unclear. Some patients developed multiple eruptive dermatofibromas after the intake of immunosuppressive drugs[5] and in the context of human immunodeficiency virus infection,[1] suggesting an immunopathogenic etiology. It was proposed that dermatofibroma represents an abortive immunoreactive process mediated by dermal dendritic cells, and the development of multiple eruptive dermatofibromas can be triggered by the inhibition of regulatory T cells in immunodeficiency states or as an exaggerated response to a putative pathogen that could not be cleared by the suppressed immune system.
Studies have revealed defective T-cell immunity in hepatitis B virus infection, which is described as the 'exhaustion' state, characterized by poor effector cytotoxic activity, impaired cytokine production, and sustained expression of multiple inhibitory receptors, such as programmed cell death-1, lymphocyte activation gene-3, cytotoxic T-lymphocyte-associated antigen-4, and CD244.[6]
In our case, the patient showed decrease in regulatory T cells. Although some previous studies reported multiple eruptive dermatofibromas developing in patients with diabetes mellitus, obesity, hypertension, and hypertriglyceridemia as in our case, it seems to be questionable whether there is any correlation between multiple eruptive dermatofibromas and these diseases.[2] In conclusion, more cases and research are required to speculate on the pathogenesis and it is important to screen for altered immunity in patients with multiple eruptive dermatofibromas.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ammirati CT, Mann C, Hornstra IK. Multiple eruptive dermatofibromas in three men with HIV infection. Dermatology 1997;195:344-8.
[Google Scholar]
|
| 2. |
Niiyama S, Katsuoka K, Happle R, Hoffmann R. Multiple eruptive dermatofibromas: a review of the literature. Acta Derm Venereol 2002;82:241-4.
[Google Scholar]
|
| 3. |
Goldbach H, Wanat K, Rosenbach M. Multiple eruptive dermatofibromas in a patient with sarcoidosis. Cutis 2016;98:E15-9.
[Google Scholar]
|
| 4. |
Lopez N, Fernandez A, Bosch RJ, Herrera E. Multiple eruptive dermatofibromas in a patient with Graves-Basedow disease. J Eur Acad Dermatol Venereol 2008;22:402-3.
[Google Scholar]
|
| 5. |
Llamas-Velasco M, Fraga J, Solano-López GE, Steegmann JL, García Diez A, Requena L. Multiple eruptive dermatofibromas related to imatinib treatment. J Eur Acad Dermatol Venereol 2014;28:979-81.
[Google Scholar]
|
| 6. |
Ye B, Liu X, Li X, Kong H, Tian L, Chen Y. T-cell exhaustion in chronic hepatitis B infection: Current knowledge and clinical significance. Cell Death Dis 2015;6:e1694.
[Google Scholar]
|
Fulltext Views
6,154
PDF downloads
2,019





