Translate this page into:
Crusted nipple and areola: A new aetiology of secondary hyperkeratosis of the nipple and areola
Correspondence Address:
Dhaifallah A Alenizi
Department of Dermatology, Faculty of Medicine, Northern Borders University, P.O. Box: 1321, Arar 91431
Kingdom of Saudi Arabia
| How to cite this article: Alenizi DA. Crusted nipple and areola: A new aetiology of secondary hyperkeratosis of the nipple and areola. Indian J Dermatol Venereol Leprol 2019;85:169-170 |
Abstract
Hyperkeratosis of the nipple and areola is a rare condition first described by Tauber in 1923. Less than 100 cases have been reported in the literature. Hyperkeratosis of the nipple and areola presents as hyperkeratotic, hyperpigmented plaques on the nipple and areola. It is more common in females. An 18-year-old female patient presented with hyperkeratotic, plaque-like, hard crusts on both nipples and areolas. The examining physician could successfully remove this crust using his finger. The crust had accumulated as a result of the patient's reluctance to touch or clean the breast area due to psychological issues. A crusted nipple and areola may occur as a secondary condition due to a patient's reluctance to touch or clean their breasts.
Introduction
Hyperkeratosis of the nipple and/or areola is a rare skin condition defined as over-keratinization of the nipple and/or areola and is characterized by the presence of hyperpigmented, crusted, keratotic thickening of the nipple and/or areola. It is often misdiagnosed. It is classified into three subsets: Type I hyperkeratosis of the nipple and areola due to the extension of an epidermal nevus, type II hyperkeratosis of the nipple and areola in conjunction with disseminated dermatoses and type III nevoid hyperkeratosis of the nipple and areola.[1] Moreover, primary hyperkeratosis of the nipple and areola is idiopathic, while secondary hyperkeratosis of the nipple and areola is caused by a variety of skin conditions (e.g. epidermal nevus, organoid nevus and leiomyomas).[2],[3],[4],[5],[6]
Case Report
An 18-year-old female patient visited us at Alkhibrah Medical Complex in Arar, Saudi Arabia, with complaints of dark-brown, verrucous, plaque-like hard crusts on both the nipples and areolas, which had developed over the preceding 5 months. The crust had first appeared mainly on the areolas and expanded inward. She had type IV skin with a normal body mass index. Her medical and surgical history was unremarkable and she was not taking any medications. Her mother was 51 years old and had been diagnosed with ductal breast cancer 2 years earlier. She received chemotherapy and radiotherapy, but died 3 months after our patient presented with her complaints. Following this, the patient had become anxious that she would also develop breast cancer and, therefore, she became obsessive about not cleaning or touching her breasts.
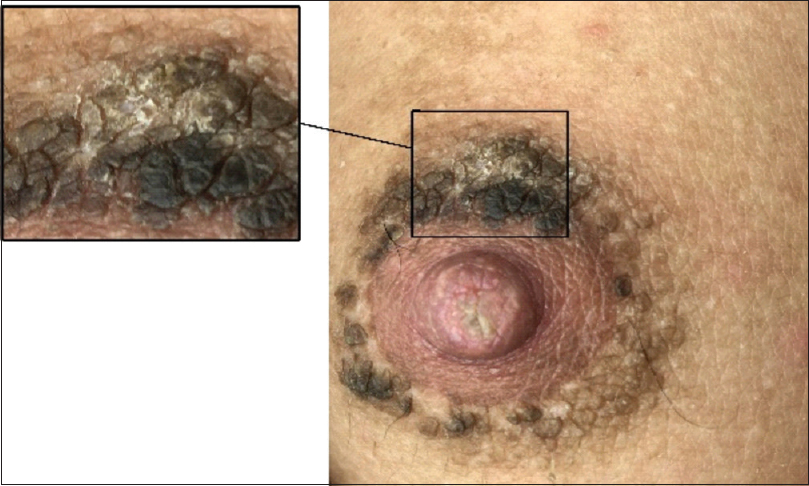
Examination revealed bilateral yellow/dark-brown, plaque-like, friable hard crusts covering both areolas and nipples [Figure - 1] and [Figure - 2]. There were no similar lesions on any other body parts. A mammography was performed before dermatology consultation and no abnormality was detected.
 |
| Figure 1: Bilateral yellow/dark-brown, plaque-like, friable hard crusts covering both the areola and nipple |
 |
| Figure 2: The successful removal of crust following treatment with 5% salicylic acid ointment |
The patient was shown how to clean her breasts, and was reassured that cleaning and handling the breast does not increase the likelihood of developing breast cancer. In addition, 5% salicylic acid ointment was applied and the crust disappeared within a week. Informed consent was obtained from the patient to publish this case.
Discussion
When hyperkeratosis of the nipple and areola is idiopathic, the recommended classification is primary hyperkeratosis of the nipple and areola. When it is associated with epidermal nevus, organoid nevus, leiomyomas, verruca, congenital, acquired or erythrodermic ichthyosis, malignant acanthosis nigricans, Darier's disease, atopic dermatitis, cutaneous T-cell lymphoma or chronic mucocutaneous candidiasis,[2],[3],[4],[5],[6] the recommended classification is secondary hyperkeratosis of the nipple and areola. It has been reported in women of child-bearing age and males receiving hormonal therapy for prostate cancer[7],[8] as well as males receiving estrogen therapy for androgen insensitivity syndrome.[9]
This case demonstrates a potential new aetiology that may mimic secondary hyperkeratosis of the nipple and areola, named “crusted nipple and areola.” Kaminska-Winciorek et al. described two similar cases as “neglected nipples,” which had presented as acanthosis nigricans-like plaques that developed due to avoidance of nipple cleansing.[10]
In conclusion, crusting of the nipple and areola can manifest as secondary hyperkeratosis of the nipple and areola due to negligence or avoidance of cleaning the breasts due to fear, misconception or a psychological condition. When dealing with hyperkeratosis of the nipple and areola, the physician should try to remove the plaque using fingers. Additionally, wiping the affected area with an alcohol swab is helpful[11] to confirm that it is simply a hard crust. Because a hard crust could clinically mimic hyperkeratosis of the nipple and areola, it is recommended that it should be included as a potential cause of secondary hyperkeratosis of the nipple and areola.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Acknowledgement
We would like to thank Editage (www.editage.com) for English language editing and publication support.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Pérez-Izquierdo JM, Vilata JJ, Sánchez JL, Gargallo E, Millan F, Aliaga A, et al. Retinoic acid treatment of nipple hyperkeratosis. Arch Dermatol 1990;126:687-8.
[Google Scholar]
|
| 2. |
Baz K, Kokturk A, Kaya TI, Ikizoglu G, Düşmez D, Koca A, et al. A case of hyperkeratosis of the nipple and areola resulting from organoid nevus. Int J Dermatol 2003;42:318-20.
[Google Scholar]
|
| 3. |
Samimi M, Maître F, Estève E. Hyperkeratotic lesion of the nipple revealing cutaneous leiomyoma. Ann Dermatol Venereol 2008;135:571-4.
[Google Scholar]
|
| 4. |
Lee HW, Suh HS, Choi JC, Lee MW, Choi JH, Moon KC, et al. Hyperkeratosis of the nipple and areola as a sign of malignant acanthosis nigricans. Clin Exp Dermatol 2005;30:721-2.
[Google Scholar]
|
| 5. |
Fitzgerald DA, Lewis-Jones MS. Darier's disease presenting as isolated hyperkeratosis of the breasts. Br J Dermatol 1997;136:290.
[Google Scholar]
|
| 6. |
Ahn SK, Chung J, Soo Lee W, Kim SC, Lee SH. Hyperkeratosis of the nipple and areola simultaneously developing with cutaneous T-cell lymphoma. J Am Acad Dermatol 1995;32:124-5.
[Google Scholar]
|
| 7. |
Schwartz RA. Hyperkeratosis of nipple and areola. Arch Dermatol 1978;114:1844-5.
[Google Scholar]
|
| 8. |
Mold DE, Jegasothy BV. Estrogen-induced hyperkeratosis of the nipple. Cutis 1980;26:95-6.
[Google Scholar]
|
| 9. |
Lambiris AG, McCormick F. Unilateral hyperkeratosis of nipple and areola associated with androgen insensitivity and oestrogen replacement therapy. J Eur Acad Dermatol Venereol 2001;15:376-7.
[Google Scholar]
|
| 10. |
Kaminska-Winciorek G, Wydmanski J, Scope A, Argenziano G, Zalaudek I. “Neglected nipples”: Acanthosis nigricans-like plaques caused by avoidance of nipple cleansing. Dermatol Pract Concept 2014;4:81-4.
[Google Scholar]
|
| 11. |
Saha A, Seth J, Sharma A, Biswas D. Dermatitis neglecta-A dirty dermatosis: Report of three cases. Indian J Dermatol 2015;60:185-7.
[Google Scholar]
|
Fulltext Views
15,739
PDF downloads
1,340





