Translate this page into:
Pigeon tick infestation in humans: A case from North India
Correspondence Address:
Jasleen Kaur Sandhu
Department of Dermatology, D Block, Level 5, Government Medical College and Hospital, Chandigarh - 160 031
India
| How to cite this article: Sandhu JK. Pigeon tick infestation in humans: A case from North India. Indian J Dermatol Venereol Leprol 2019;85:523-524 |
Sir,
Urban areas with their high-rise buildings provide nesting and breeding facilities for feral pigeons. This, along with availability of food, has led to an explosive increase in population of feral pigeons in the cities. The feral pigeon acts as a host for many ectoparasites like pigeon bug (Cimex columbiaris), red mites (Dermanyssus gallinae), pigeon flea (Ceratophyllus columba), and the most frequent pigeon tick (Argas reflexus).[1] Due to the close proximity of the natural habitat of pigeons and humans in cities, these ectoparasites can cause infestations in humans also. Out of all these, pigeon tick is of the most medical importance because of its potential to transmit tick-borne infections and high rates of sensitization to its bite, with even fatal anaphylactic reactions being reported.[2]
There have been several reports of pigeon tick infestation in humans from Europe.[2],[3],[4] This is a report of pigeon tick infestation in humans from a North Indian city. There are no prior reports of this ectoparasite infestation in humans from India. It is very likely due to underdiagnosis and may not entirely be due to its absence. This report intends to increase the awareness of this infestation among dermatologists and physicians.
A 35-year-old man, a medical professional residing in an urban area, presented to the dermatology outpatient department with a history of recurrent insect bites for the past 3 years. There was history of similar complaints in other family members also. The bites were always noticed in the mornings and occurred only when any of the members slept in a particular bedroom. He also brought along insects which were found in this bedroom. The bites used to occur on exposed parts and caused itchy reddish swellings which were painful. These used to subside in about 10 days to 3 weeks. The bite he presented with had occurred around 2 weeks back. There was no history of generalized rash, hypotension or breathing difficulty. There were no pet animals and he had not noticed any seasonal variation. On examination, a skin-colored papule was seen on the right wrist [Figure - 1]. Microscopic examination of the insect identified it to be a pigeon tick [Figure - 2]. Further enquiries revealed that the patient's family lived on the top floor of a three-storey building and this particular bedroom opened to a balcony which had many pigeons and pigeon nests. The patient was counseled about pigeon tick infestation. He was already contemplating a residence change and did not suffer any new bites after moving to the new residence.
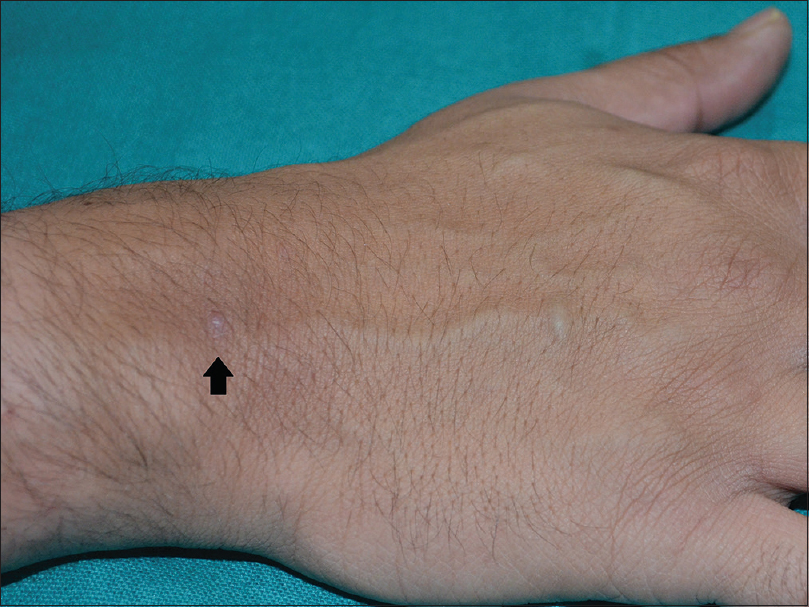 |
| Figure 1: A 2-week-old bite seen as a skin-colored papule (arrow) on the right wrist |
 |
| Figure 2: Pigeon tick (Argas reflexus) found by the patient in the bedroom |
Pigeon tick, Argas reflexus, is one of the most common temporary blood-sucking ectoparasite of feral pigeons. It belongs to the soft tick family Argasidae.[5] It is brownish in color, 4–15 mm long and 6–7 mm wide when unfed. It has a flattened appearance dorsoventrally.[5] The immense ecological success of this tick species is due to its long life span of 7–10 years and the ability to live without blood meal for a long time even upto many years.[1]
Pigeon tick typically lives in and around the nests of feral pigeons and feeds at night while remaining hidden in crevices during the day. It is forced into human dwellings in search of blood meal if the natural host pigeons are not available in sufficient numbers. Although these ticks may attack humans, it is known that it is unable to lay eggs with human blood. Therefore, any human infestation can always be traced back to its natural host pigeon, without which it cannot establish a population.[1]
Bite reactions by the pigeon tick vary from mild mosquito bite–like reaction to severe immunoglobulin E-mediated anaphylaxis.[2],[6] Even fatal anaphylactic shock has been reported.[2] The antigen is likely to be tick salivary proteins and is highly allergenic with induction of hypersensitivity in around 40% of bitten individuals.[4] Anaphylactic shock has been reported in 8% of individuals with pigeon tick bites in a study of 148 cases.[4] The time for resolution of local bite reaction varies from several days to weeks to even years depending on the patients' physiological response to the antigen and presence of any secondary infection.[6]
This ectoparasite infestation very likely suffers from underdiagnosis as there are fewer reports of pigeon tick bites in humans when compared to the high likelihood of its presence in urban areas with large population of pigeons. In this case also, the diagnosis could be made because the patient brought the insects along with him. Otherwise, the cause of skin lesion may have been attributed to some other arthropod and would have been treated symptomatically. The difficulty in diagnosis arises because most of the blood-sucking parasites feed at night, and hide during the day. So the patient is mostly unaware of the source of the bite.
Awareness along with a high index of suspicion is the key to the diagnosis of this potentially life-threatening ectoparasite infestation. Patients need to be asked about the presence of feral pigeons nesting in or around their homes and guided to careful inspection of their living quarters for these parasites for confirmation of the diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Acknowledgement
The author would like to thank Dr. M. Ramam, Professor, Dermatology and Venereology, AIIMS, New Delhi for the help with the macro photography of the pigeon tick and Dr. Archana Chauhan, Assistant Professor, Department of Zoology, Panjab University, for the identification of the tick.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Haag-Wackernagel D, Bircher AJ. Ectoparasites from feral pigeons affecting humans. Dermatology 2010;220:82-92.
[Google Scholar]
|
| 2. |
Rolla G, Heffler E, Boita M, Doyen V, Mairesse M, Cvackova M, et al. Pigeon tick bite: A neglected cause of idiopathic nocturnal anaphylaxis. Allergy 2018;73:958-61.
[Google Scholar]
|
| 3. |
Buczek A, Bartosik K, Kulina D, Raszewska-Famielec M, Borzęcki A. Skin lesions in humans bitten by European pigeon tick Argas reflexus (Fab.) (Ixodida: Argasidae) massively occurring in the upper Silesian conurbation of South-West Poland. Ann Agric Environ Med 2018;25:234-40.
[Google Scholar]
|
| 4. |
Kleine-Tebbe J, Heinatz A, Gräser I, Dautel H, Hansen GN, Kespohl S, et al. Bites of the European pigeon tick (Argas reflexus): Risk of IgE-mediated sensitizations and anaphylactic reactions. J Allergy Clin Immunol 2006;117:190-5.
[Google Scholar]
|
| 5. |
Walker AR, Bouattour A, Camicas JL, Estrada-Pena A, Horak IG, Latif AA, et al., editors. Biology of ticks and methods of identification. In: Ticks of Domestic Animals in Africa: A Guide to Identification of Species. Edinburgh, Scotland: Biosciences Reports; 2014. p. 21-7.
[Google Scholar]
|
| 6. |
Bircher AJ. Systemic immediate allergic reactions to arthropod stings and bites. Dermatology 2005;210:119-27.
[Google Scholar]
|
Fulltext Views
17,061
PDF downloads
1,659





