Translate this page into:
Acral porokeratosis associated with anonychia
Correspondence Address:
Gurumoorthy Rajesh
Department of Dermatology, Sri Manakula Vinayagar Medical College and Hospital, Madagadipet, Puducherry
India
| How to cite this article: Rajesh G, Devan P, Keerthi S, Karthikeyan K. Acral porokeratosis associated with anonychia. Indian J Dermatol Venereol Leprol 2018;84:81-82 |
Sir,
Among dermatological disorders, porokeratosis remains an enigma owing to its uncertain pathogenesis, varied clinical presentations, and unpredictable outcome. Porokeratosis is characterized by marginate scaling lesions, histologically showing a column of parakeratotic keratinocytes (the cornoid lamella). Various morphological patterns include classical porokeratosis of Mibelli, disseminated superficial actinic porokeratosis, disseminated superficial porokeratosis of immunosuppression, childhood forms, linear porokeratosis, porokeratosis palmaris et plantaris disseminata, and punctate porokeratosis.[1]
While a few cases involving distal extremities with nail changes have been described in the literature, complete loss of nail (anonychia), with exclusive involvement of the acral area, is very rare.
A 35-year-old female patient, an agricultural laborer, presented with a history of raised asymptomatic lesions, over the right hand and bilateral feet, of one-year duration. She had noticed a ring-like lesion over her feet, involving the toes, with associated nail discoloration and subsequent dystrophy. Subsequently, she noticed similar lesions involving the right hand. The skin lesions preceded the involvement of nails. There was no family history of similar illness.
On cutaneous examination, a well-defined, hyperpigmented plaque with a prominent peripheral keratotic ridge and central atrophy and depigmentation was seen over the right hand involving the thumb, and the medial border of the second finger and first interdigital space [Figure - 1]. Anonychia of the right thumb nail was seen. Bilaterally, the dorsa of the feet showed similar plaques of size 5 × 5 cm over the first and second toes. There was anonychia over both the great toe nails [Figure - 2]. The right second toe nail showed dystrophy. There was no involvement of the oral or genital mucosa. The patient had no features of immunosuppression.
 |
| Figure 1: A well-defined, hyperpigmented plaque with a prominent keratotic ridge at the periphery and central atrophy and depigmentation seen over the right hand |
 |
| Figure 2: Bilateral dorsa of feet shows well defined plaques of size 5 cm × 5 cm with peripheral raised margins over the first and second toes. There was anonychia over both the great toe nails |
Skin biopsy, taken from the edge of the lesion, showed acanthosis, hyperkeratosis, papillomatosis, and a keratin-filled invagination with a central parakeratotic column, suggestive of cornoid lamellae. The epidermis underlying the cornoid lamella showed absence of granular layer [Figure - 3]. The dermis showed minimal perivascular lymphocytic infiltration. All the other laboratory investigations were found to be within normal limits. Patient chose treatment with electrocautery; however, the response was poor.
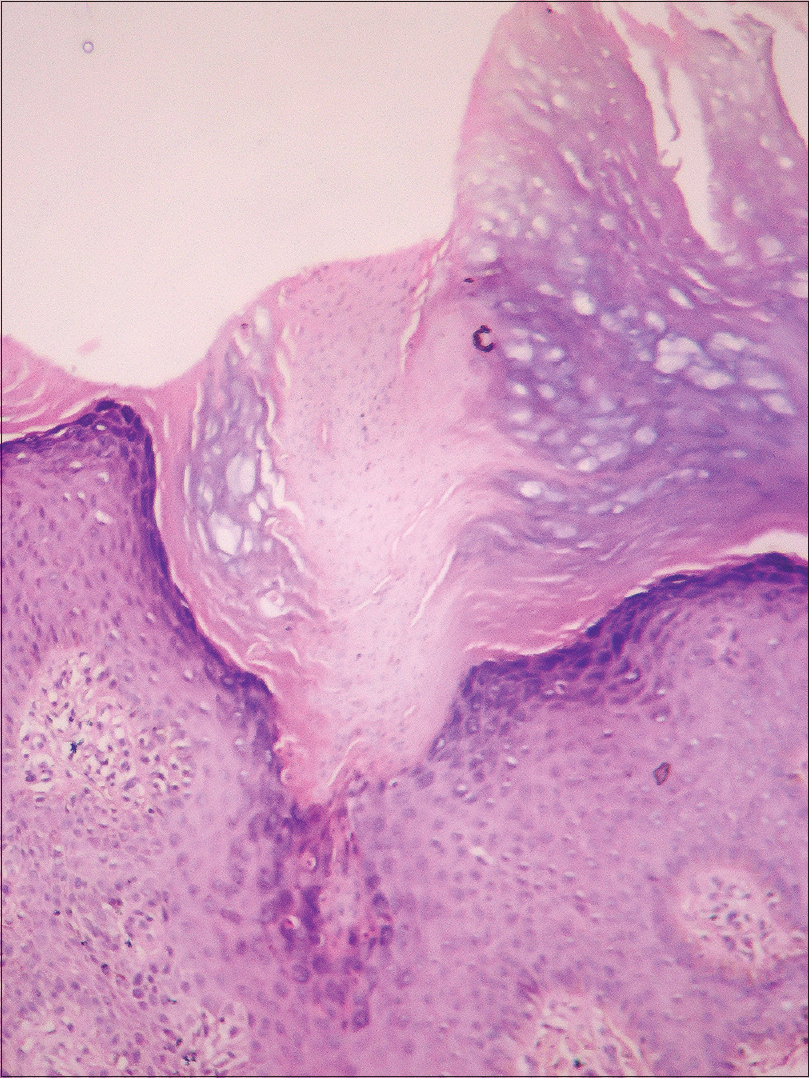 |
| Figure 3: Hyperkeratosis, papillomatosis and a keratin filled invagination. From the center of the keratin filled invagination raises a parakeratotic column suggestive of cornoid lamellae (H and E, ×100) |
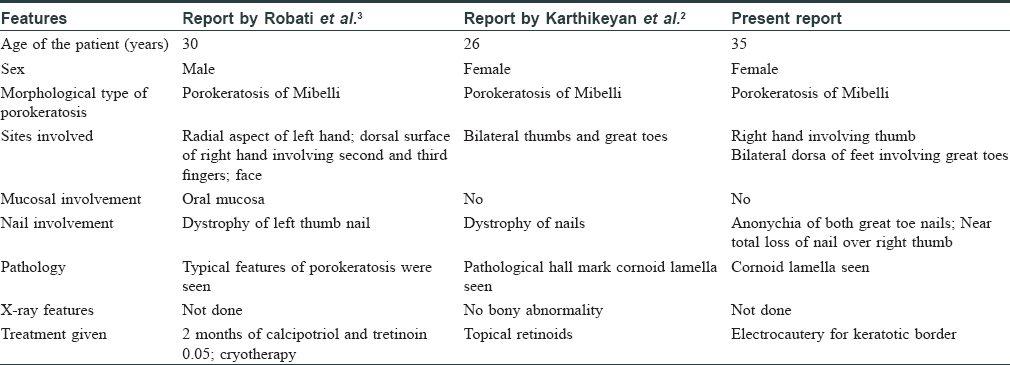
Porokeratosis presents itself in a fascinating array of morphological variants. The morphology of porokeratosis depends upon the site and the triggers. Based on the site, facial prorokeratosis, genital porokeratosis, and porokeratosis ptychotropica have been described in the literature.[1],[2] However, porokeratosis of the acral areas, particularly the thumbs, with nail involvement is very rare. Two case reports describing nail involvement are compared with this case in [Table - 1]. This case presented with anonychia of the affected digits and it could be due to the disease process involving the nail matrix and nail bed.
Apart from the genetic causes, certain environmental triggers such as irradiation/ultraviolet light, mechanical trauma, infective agents have been proposed as etiological factors. Immunosuppression has also been implicated. Certain drugs, such as thiazide diuretics, and immunosuppressive drugs such as prednisolone, azathioprine, used in organ transplantation, have also been reported as etiological factors in elderly patients. This case is being presented for the unusual involvement of acral areas, along with anonychia, giving rise to the intriguing possibility of a new clinical variant of porokeratosis i.e., acral porokeratosis with anonychia. [3]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sertznig P, von Felbert V, Megahed M. Porokeratosis: Present concepts. J Eur Acad Dermatol Venereol 2012;26:404-12.
[Google Scholar]
|
| 2. |
Karthikeyan K, Thappa DM, Udayashankar C. Porokeratosis of mibelli with nail dystrophy. J Dermatol 2003;30:420-2.
[Google Scholar]
|
| 3. |
Robati RM, Rahmati-Roodsari M, Ayatollahi A, Hejazi S. Facial and bilateral acral porokeratosis with nail dystrophy: A case report. Dermatol Online J 2011;17:5.
[Google Scholar]
|
Fulltext Views
3,558
PDF downloads
2,565





