Translate this page into:
A survey on the pattern of dermoscopy use among dermatologists in India
2 Department of Dermatology, KIMS AL Shifa Super Speciality Hospital, Perinthalmanna, Kerala, India
3 Department of Dermatology, Amrita Institute of Medical Sciences, Kochi, Kerala, India
Correspondence Address:
Feroze Kaliyadan
Department of Dermatology, College of Medicine, King Faisal University, Al-Hasa 31982
Saudi Arabia
| How to cite this article: Kaliyadan F, Ashique KT, Jagadeesan S. A survey on the pattern of dermoscopy use among dermatologists in India. Indian J Dermatol Venereol Leprol 2018;84:120 |
Abstract
Introduction and Background: Dermoscopy is being increasingly used for improving dermatological diagnosis. Use of dermoscopy in the early recognition of skin malignancies, especially melanoma, is well established. Of late, its use in general clinical dermatology is growing with the recognition of new and specific patterns in conditions such as hair disorders, inflammatory disorders, and infections/infestations. This cross-sectional survey aims to assess the common patterns of dermoscopy use by Indian dermatologists.Methods: This was across-sectional survey. An online questionnaire was used to collect data. The questionnaire focused on the frequency of dermoscopy use by Indian dermatologists, reasons for using it or not, and the training they had received on dermoscopy.
Results: Of the total 150 valid responses, eighty two (54.7%) participants reported that they were using dermoscopy routinely in their clinical practice. Lack of familiarity and lack of proper training were the important reasons cited for not using dermoscopy regularly. Among the dermatologists using dermoscopy, consensus on effectiveness was highest for hair disorders.
Conclusions: Dermoscopy use by dermatologists in India is mainly in the context of inflammatory dermatosis and hair disorders rather than skin tumors. Lack of familiarity with the technique appears to be main factor limiting the use of dermoscopy in India.
Limitations: Small sample size is the major limitation of this study. It is possible that a large number of dermatologists who do not use dermoscopy might not have responded to the survey, there by affecting the results and their interpretation.
Introduction
Dermoscopy is being increasingly used for improving dermatological diagnosis. Use of dermoscopy in the early recognition of skin malignancies, especially melanoma, is well established. Of late, its use in general clinical dermatology is growing with the recognition of new and specific patterns in conditions such as hair disorders, inflammatory disorders, and infections/infestations.[1],[2] Although there are no national surveys or cross country data, the incidence of skin malignancies is significantly less in India, primarily due to the darker skin type of the population. In India, non melanoma skin cancers are relatively more common compared to melanoma.[3],[4] The low incidence of skin cancers is probably the main reason why dermoscopy has less relevance in India for early recognition of skin malignancies. Despite this, the interest in dermoscopy as a general diagnostic tool has been growing in India as evidenced by the increasing space devoted to dermoscopy in Indian dermatology journals and dermatology conferences held in India.[2] This cross-sectional survey aims to assess the common patterns of dermoscopy use by Indian dermatologists.
Methods
This was across-sectional questionnaire-based survey. The questionnaire was adapted from a previously validated questionnaire used in a cross-sectional survey by Butler et al.[5] The modified questionnaire was pretested on a group of six dermatologists and was further refined based on their feedback to obtain the final draft. The final questionnaire was sent out as an electronic survey (as an electronic link via email) to approximately 1000 dermatologists. The identity of the dermatologists responding to the survey was not blinded to the investigators. The survey was live for about 12 weeks from November 2016 to January 2017.
Results
The questionnaire was sent as an electronic survey to approximately 1000 active members of the Indian Association of Dermatologists, Venereologists and Leprologists. One hundred and fifty valid responses were obtained.
Of the total 150 respondents, 76 were females. Eighty two (54.7%) respondents used dermoscopy routinely in their clinical practice. Forty eight among them were males.
In the group who were using dermoscopy routinely (n = 82), thirty two (39%) were working in an academic setting compared to 30 (44.2%) in the group not using dermoscopy.
The average age of the respondents was 37.8 years (range = 27–65 years). Nonusers' average age was 36.7 years and users' average age was 38.9 years. This difference was not statistically significant (unpaired t-test, 95% confidence intervals: −5.2077–0.9877, P value = 0.18) The average duration of practice was lower in the group not using dermoscopy routinely (8.12 years) compared to the group using dermoscopy routinely (11.09 years). This difference was also not statistically significant (unpaired t-test, 95% confidence intervals −5.9618–0.0218, P value = 0.052).
Among the 150 respondents, only one disagreed with the statement that “dermoscopy is a useful tool for dermatological practice in India”. A total of 24 (16%) respondents took a neutral view (neither agreeing nor disagreeing), seventy four (49.3%) respondents agreed with the statement, and 51 (34%) strongly agreed with the statement. Among the group using dermoscopy routinely, the consensus on utility of dermoscopy use was expectedly stronger: forty one (50%) strongly agreeing, thirty five (42.6%) agreeing, and only six (7.3%) with a neutral view as compared to the group not using dermoscopy in which 39 (57.3%) agreeing, ten (14.7%) strongly agreeing, eighteen (26.4%) being neutral, and one (1.4%) participant disagreeing.
Major reasons given for not using dermoscopy at present included the following (more than one option was chosen by some respondents):
- Not familiar with the technique – 47 (69.1%)
- High cost –21 (30.8%)
- Not convinced of the utility – 20 (29.4%)
- Lack of time – 11 (16.1%).
Regarding dermoscopy training, fifty five (36.6%) respondents mentioned that they had not undergone training of any kind related to dermoscopy. Nine (6%) respondents had received formal training/fellowships in dermoscopy. Thirty two (21.3%) respondents had attended short workshops for dermoscopy and 53 (35.3%) respondents mentioned that they had learnt dermoscopy by themselves “on the job”. Of the respondents using dermoscopy, seventy five (91.4%) agreed that dermoscopy significantly improved diagnostic accuracy in their routine clinical practice. Thirty seven (45%) among them actively participated in discussions on dermoscopy in social media.
The extent of dermoscopy use, i.e. the average percentage of case for which they used dermoscopy during routine clinical practice, varied from 1% to 100% (some respondents mentioned that they used the dermoscopy for all cases they see). The average was 12.5% of the cases.
The reasons given for using dermoscopy in clinical practice included the following (more than one option was chosen by some respondents):
Belief that it would enhance patient care – 40 (48.7%)
Enthusiasm for the concept – 37 (45%)
Keen on trying new gadgets – 12 (14.6%)
Got it as a gift – 7 (8.5%)
“For the heck of it”– 2 (2.4%).
Among the common brands of dermoscopes used by the respondents, the two most popular brands were – Dermlite® (19; 23.17%) and Heine™ (13; 15.8%). Other brands included Dermaindia®, Tejco®, Dinolite®, Canfield®, Firefly®, and Cas-lite®.
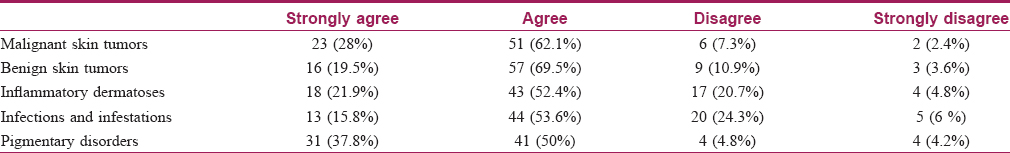
Regarding the specific conditions for which the respondents found dermoscopy useful, maximum consensus was for hair disorders –48 (58.5%) respondents strongly agreeing and 34 (41.4%) agreeing. For other conditions, the response was as follows: [Table - 1]
Discussion
The use of dermoscopy in India has contextual differences compared to other countries because of the very low incidence of skin malignancies here. Despite this, the popularity of dermoscopy is growing in India with new dermascopy patterns being described in inflammatory disorders and infections. A recent large pan-European survey (n = 7480) on patterns, attitudes and training of the use of dermoscopy showed that 89% of the respondents used dermoscopy regularly. The two most important reasons cited for not using dermoscopy were lack of equipment (58% of nonusers) and lack of training (42%). Higher use of dermoscopy across the entire spectrum of skin diseases was reported by 62% of dermoscopy users and it was statistically associated with obtaining dermoscopy training during residency, use of polarized light and digital dermoscopy devices, longer dermoscopy practice, younger age, and female gender.[6]
A study by Butler et al. from United Kingdom compared two surveys on dermoscopy use among dermatologists - one in 2003 (n = 292) and another in 2012 (n = 209). Most (98.5%) of the respondents in 2012 reported regular use of dermoscopy, where as only 54% were using it regularly in 2003. The same study reported a significant increase in those who received formal training in dermoscopy - from approximately 40% in 2003 to 81% in 2012.[5] This study also showed that dermoscopy use was being extended to conditions such as inflammatory dermatosis, infestations, and hair, and nail disorders.[5]
A study from United states by Murzaku et al. (n = 277) also showed a high percentage of routine use of dermoscopy (80.7% of the respondents). Unlike in our study, Murzaku et al. reported that 97.8% of dermatologists who were five years or less in dermatology practice used dermoscopy and 100% had received training on its use. This could be partly attributed to dermoscopy becoming an integral part of the residency training. However, it is interesting that, in this study only 31.3% reported performing dermoscopy on all pigmented lesions, based on which the authors concluded that dermoscopy is still underutilized.[7] This study by Murzaku et al. showed an increasing trend of dermoscopy use and training compared to previous studies from the United States reported by Engasser and Warshaw and Noor et al.[8],[9]
Engasser and Warshaw in a previously reported survey from the United states with a larger sample size (n = 3238) showed that approximately half of the respondents used dermoscopy in their practice. Dermoscopy users were more likely to be younger, involved in resident teaching and had received training in dermoscopy.[9]
In a study reported by Noor et al. (n = 105), only 60% of the participants reported regular use of dermoscopy. The main reasons cited in this survey for not using dermoscopy included lack of conviction regarding its effectiveness, need for receiving more training and excessive time involved in its use.[8] The reasons for not using dermoscopy were similar in our study too.
The relatively low incidence of skin malignancies in India partly explains the fact that most dermatologists using dermoscopy in this study felt that the most common indication for which they used dermoscopy was hair disorders (trichoscopy). Trichoscopy has been described to be useful in the diagnosis of numerous disorders related to the hair follicles. Hair diseases in which specific patterns have been described include alopecia areata, androgenetic alopecia, discoid lupus erythematosus, folliculitis decalvans, genetic hair shaft abnormalities, lichen planopilaris, scalp psoriasis, tinea capitis, and trichotillomania.[10]
An interesting finding in our study, although not statistically significant, was that the average age and years of experience of dermatologists who were using dermoscopy regularly was higher than those not using it. A good dermoscope can be a costly investment and it is likely that an established dermatologist is more likely to invest in it. This trend is expected to change in coming years, when younger dermatologists are exposed to training in dermoscopy.
A survey from Australia by Piliouras et al. in 2014 also showed a generally positive attitude towards dermoscopy among the respondents (n = 143). All the respondents in this study were using dermoscopy, and 84% mentioned that they performed it whenever skin tumors are suspected.[11] In our study, the use of dermoscopy, in terms of percentage of patients in which it was used, was quite low. This would probably be a reflection of the lower incidence of skin tumors in our population. A previous study from Australia by Venugopal et al. showed a high percentage of dermoscopy use (98%, n = 99), wherein 78% also used some image capture device along with the dermoscope.[12]
A survey from France conducted by Breton et al. (n = 76) showed an increased use of dermoscopy in nonacademic centers compared to academic centers.[13] Our study showed an opposite pattern. We assume that, in the Indian context, academic centers are more likely to invest in a dermoscope for clinical and research needs compared to nonacademic centers.
To our knowledge, this is the first survey assessing the patterns of dermoscopy use among dermatologists in India. The use of dermoscopy in India has contextual differences because of the very low incidence of skin malignancies here. Specific dermoscopic patterns have been described (with new findings being described) in diseases of skin, hair and nails more commonly seen in India. However, there are very few studies addressing the question whether or not dermoscopy makes significant differences to the decision-making process in these cases. More studies are needed to assess the effectiveness of dermoscopy in improving accuracy of diagnosis, decision-making and patient outcomes in skin diseases commonly seen in India. Understanding the basics of dermoscopy and proper training are important for its effective use as a diagnostic tool. This is especially true in conditions such as malignancy.[14]
Conclusions
In summary, though dermoscopy is being increasingly used by Indian dermatologists, the usage appears to be less compared to other geographical areas such as Europe, Australia, and the United states. Dermoscopy use by dermatologists in India is mainly in the context of inflammatory dermatos is and hair disorders rather than skin tumors. Lack of familiarity and proper training are important reasons cited for dermoscopy not being used regularly. The cost of the equipment, lack of conviction about its utility and lack of time are other reasons cited for not using dermoscopy routinely in clinical practice.
Limitations
Small sample size of the respondents is the major limitation of the study. We attribute the small response rate to the possibility that a large number of dermatologists who are not using dermoscopy in their clinical practice might not have responded to the survey. Hence, this survey might have overestimated the percentage of dermatologists who use dermoscopy in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Micali G, Lacarrubba F, Massimino D, Schwartz RA. Dermatoscopy: Alternative uses in daily clinical practice. J Am Acad Dermatol 2011;64:1135-46.
[Google Scholar]
|
| 2. |
Kaliyadan F. The scope of the dermoscope. Indian Dermatol Online J 2016;7:359-63.
[Google Scholar]
|
| 3. |
Panda S. Non melanoma skin cancer in India: Current scenario. Indian J Dermatol 2010;55:373-8.
[Google Scholar]
|
| 4. |
Talvalkar GV. Squamous cell carcinoma of the skin. Its incidence and etio-pathogenesis in 625 cases. Indian J Cancer 1970;7:24-33.
[Google Scholar]
|
| 5. |
Butler TD, Matin RN, Affleck AG, Fleming CJ, Bowling JC. Trends in dermoscopy use in the UK: Results from surveys in 2003 and 2012. Dermatol Pract Concept 2015;5:29-38.
[Google Scholar]
|
| 6. |
Forsea AM, Tschandl P, Del Marmol V, Zalaudek I, Soyer HP, Eurodermoscopy Working Group, et al. Factors driving the use of dermoscopy in Europe: A pan-European survey. Br J Dermatol 2016;175:1329-37.
[Google Scholar]
|
| 7. |
Murzaku EC, Hayan S, Rao BK. Methods and rates of dermoscopy usage: A cross-sectional survey of US dermatologists stratified by years in practice. J Am Acad Dermatol 2014;71:393-5.
[Google Scholar]
|
| 8. |
Noor O 2nd, Nanda A, Rao BK. A dermoscopy survey to assess who is using it and why it is or is not being used. Int J Dermatol 2009;48:951-2.
[Google Scholar]
|
| 9. |
Engasser HC, Warshaw EM. Dermatoscopy use by US dermatologists: A cross-sectional survey. J Am Acad Dermatol 2010;63:412-9, 419.e1.
[Google Scholar]
|
| 10. |
Rudnicka L, Rakowska A, Olszewska M. Trichoscopy: How it may help the clinician. Dermatol Clin 2013;31:29-41.
[Google Scholar]
|
| 11. |
Piliouras P, Buettner P, Soyer HP. Dermoscopy use in the next generation: A survey of Australian dermatology trainees. Australas J Dermatol 2014;55:49-52.
[Google Scholar]
|
| 12. |
Venugopal SS, Soyer HP, Menzies SW. Results of a nationwide dermoscopy survey investigating the prevalence, advantages and disadvantages of dermoscopy use among Australian dermatologists. Australas J Dermatol 2011;52:14-8.
[Google Scholar]
|
| 13. |
Breton AL, Amini-Adle M, Duru G, Poulalhon N, Dalle S, Thomas L, et al. Overview of the use of dermoscopy in academic and non-academic hospital centres in France: A nationwide survey. J Eur Acad Dermatol Venereol 2014;28:1207-13.
[Google Scholar]
|
| 14. |
Esdaile B, Mahmud I, Palmer A, Bowling J. Diagnosing melanoma: How do we assess how good we are? Clin Exp Dermatol 2014;39:129-34.
[Google Scholar]
|
Fulltext Views
3,818
PDF downloads
2,414





