Translate this page into:
Pagetoid Bowen's disease of vulva: Excellent response to imiquimod
2 Dr. Lal Path Labs, New Delhi, India
Correspondence Address:
Pravesh Yadav
RZ-97, Phase-III, Prem Nagar, Najafgarh, New Delhi - 110 043
India
| How to cite this article: Yadav P, Mendiratta V, Rana S, Makhija M. Pagetoid Bowen's disease of vulva: Excellent response to imiquimod. Indian J Dermatol Venereol Leprol 2016;82:734-737 |
Sir,
Bowen's disease is a form of intraepidermal squamous cell carcinoma with a small chance of progression to invasive malignancy. Pagetoid Bowen's disease is a histological variant of Bowen's disease which simulates the pattern of Paget's disease, especially extramammary Paget's disease.[1]
A 28-year-old married woman presented with an itchy erosion on the vulva for the past 3 years. It started as a small, itchy, red macule which developed erosions over time. She had received multiple treatments including topical corticosteroids, calcineurin inhibitors, oral antibiotics, oral dapsone, antivirals and systemic steroids with no improvement.
Examination revealed an erythematous to violaceous, minimally indurated, non-tender plaque measuring 3 cm × 2.5 cm on the upper one-third of the left labia majora. The surface of plaque had a single, well-defined, clean looking, brightly erythematous erosion with irregular margins [Figure - 1]. Regional lymph nodes were not enlarged. Investigations including hematological workup, anti-nuclear antibodies and herpes simplex virus serology were within normal limits. Serological tests for human immunodeficiency virus and syphilis were negative.
 |
| Figure 1: Erythematous to violaceous plaque on the left labia majora, showing well-defi ned irregular erosion at the surface |
Biopsy revealed a partly eroded epidermis with single and nested atypical cells in a scattered distribution occupying the full thickness of the epidermis [Figure - 2]. A dense inflammatory infiltrate was noted around eccrine glands in the deeper dermis. A differential diagnosis of pagetoid Bowen's disease and extramammary Paget's disease was considered and immunohistochemistry with p63 and carcinoembryonic antigen was undertaken.
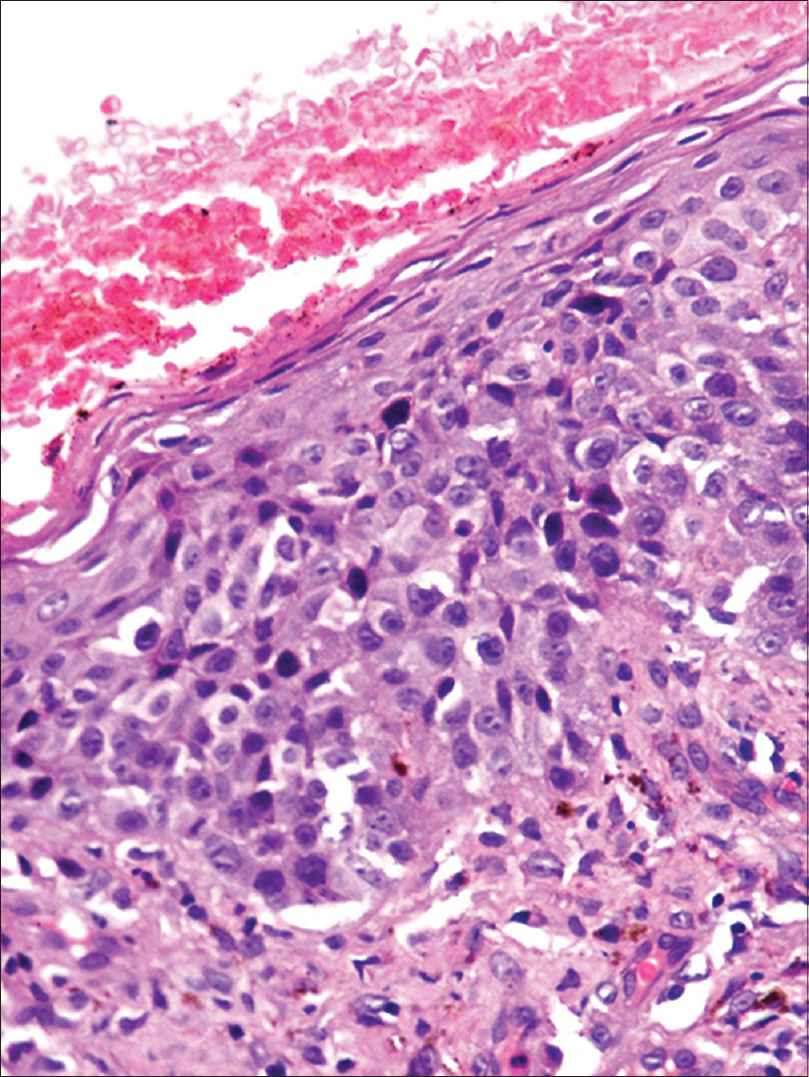 |
| Figure 2: Atypical cells with pale cytoplasm, singly as well as in clusters throughout the epidermis with minimal parakeratosis (H and E, ×400) |
Immunohistochemistry results showed strong diffuse positivity for p63 [Figure - 3]a and all the tumor cells were negative for carcinoembryonic antigen [Figure - 3]b. This confirmed the diagnosis of pagetoid Bowen's disease and the patient was started on imiquimod (5%) cream. After 6 weeks of therapy, the patient showed significant improvement [Figure - 4] and the lesion completely resolved with 12 weeks of treatment [Figure - 5]. There was no relapse after 1 year of follow-up. Further screening for internal malignancy was normal.
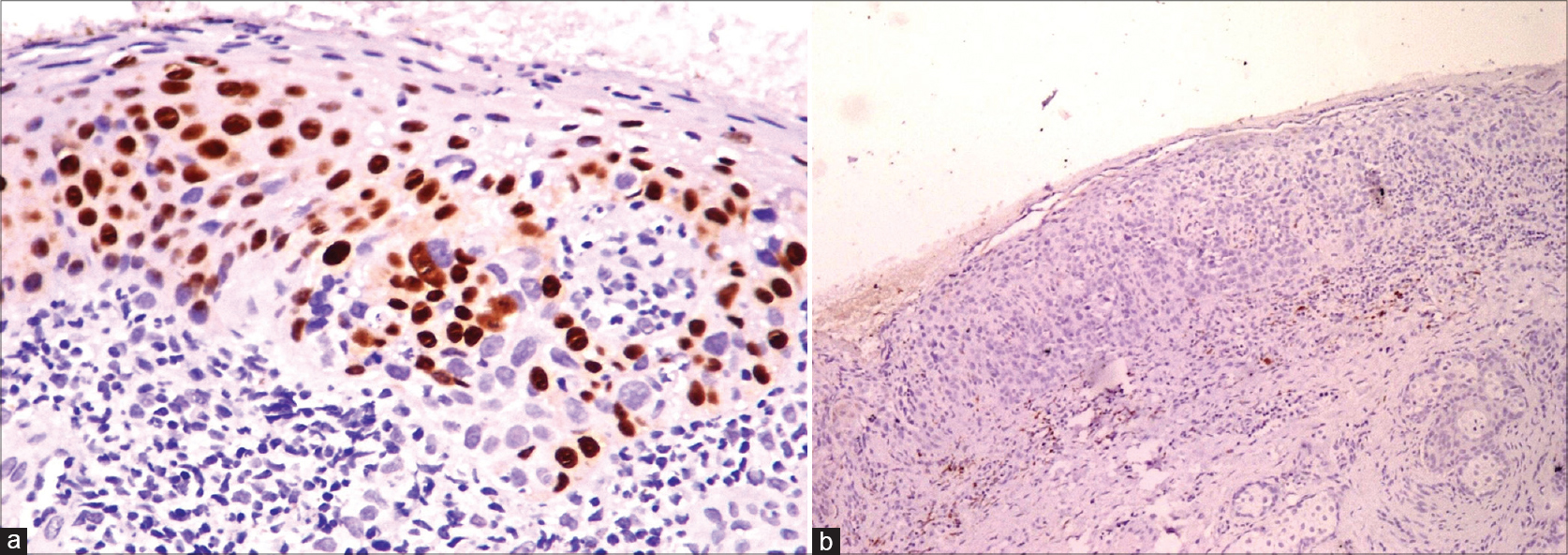 |
| Figure 3: (a) Overexpression of p63 in enlarged nuclei of atypical keratinocytes (brown) throughout the epidermis (×400). (b) Negative carcinoembryonic antigen staining (×100) |
 |
| Figure 4: Improvement after treatment with 5% imiquimod, 6 weeks after treatment |
 |
| Figure 5: Complete resolution after 12 weeks of treatment |
Pagetoid Bowen's disease is a histological variant of Bowen's disease which simulates Paget's disease.[1] There have been many case reports of extragenital pagetoid Bowen's disease but cases involving the genitalia, especially the vulva, have been rarely reported.[2]
Both pagetoid Bowen's disease and extramammary Paget's disease present as well-defined superficial erosions on the vulva associated with itching.[1],[2] These usually present with a long history and can be easily confused with other common conditions such as eczema, intertrigo, pruritus vulvae, erosive lichen planus and seborrheic dermatitis. The diagnosis of intraepidermal neoplasms or carcinoma in situ should be considered when there is lack of clinical response to topical anti-inflammatory and anti-fungal medicines.
Histopathology can help and differentiate extramammary Paget's disease from pagetoid Bowen's disease. Histologically, extramammary Paget's disease is characterized by a collection of large cells with abundant pale cytoplasm and atypical round-to-oval nuclei (Paget's cells) and are sharply demarcated from the surrounding keratinocytes. These cells are arranged in nests located primarily within the lower levels of the epidermis and often demonstrate extension into cutaneous adnexal structures.[3] Pagetoid Bowen's disease demonstrates atypical keratinocytes arranged singly or in groups, present at all levels of the epidermis. Additional histological features include intercellular bridges between nested pagetoid cells, atypical cells and multinucleated cells between the nests of cells.
In many cases, classical histopathology is not seen and immunohistochemistry becomes important to differentiate these two conditions. A study by Raju et al. showed that pagetoid Bowen's disease has a strong positivity for CK7 and keratin 903 and moderate positivity for CK5/6 and CK19, thus showing an overlap between extramammary Paget's disease and Bowen's disease.[2] However, CAM 5.2, carcinoembryonic antigen, gross cystic disease fluid protein 15 and c-erbB2 staining were negative. Syndecan-1 immunoreactivity can be used as an adjunct; its staining in pagetoid Bowen's disease is on the cell membrane whereas extramammary Paget's disease shows cytoplasmic syndecan-1 immunoreactivity.[4]
P63 has also been found to be an important marker for pagetoid Bowen's disease. As the results of immunohistochemistry are also ambiguous, p63 is considered a specific marker to differentiate these two conditions.[5]
The treatment of choice for vulval intraepithelial neoplasia is complete excision of the lesion; however, this is difficult to perform if the lesion is large. Various local treatments have been tried with variable results including 5% imiquimod, 5-fluorouracil, photodynamic therapy, laser vaporization, cryosurgery and sinecatechin. Imiquimod has proven to be very effective, especially in young females who are sexually active, the main drawback being local side effects (itching, burning, pain) which are not tolerated by many patients, thus reducing the compliance.[6] In the present case, there was complete healing of the lesion in 12 weeks.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Armes JE, Lourie R, Bowlay G, Tabrizi S. Pagetoid squamous cell carcinoma in situ of the vulva: Comparison with extramammary paget disease and nonpagetoid squamous cell neoplasia. Int J Gynecol Pathol 2008;27:118-24.
[Google Scholar]
|
| 2. |
Raju RR, Goldblum JR, Hart WR. Pagetoid squamous cell carcinoma in situ (pagetoid Bowen's disease) of the external genitalia. Int J Gynecol Pathol 2003;22:127-35.
[Google Scholar]
|
| 3. |
Fitzpatrick JE. The histologic diagnosis of intraepithelial pagetoid neoplasms. Clin Dermatol 1991;9:255-9.
[Google Scholar]
|
| 4. |
Bayer-Garner IB, Reed JA. Immunolabeling pattern of syndecan-1 expression may distinguish pagetoid Bowen's disease, extramammary Paget's disease, and pagetoid malignant melanoma in situ. J Cutan Pathol 2004;31:169-73.
[Google Scholar]
|
| 5. |
Memezawa A, Okuyama R, Tagami H, Aiba S. p63 constitutes a useful histochemical marker for differentiation of pagetoid Bowen's disease from extramammary Paget's disease. Acta Derm Venereol 2008;88:619-20.
[Google Scholar]
|
| 6. |
Le T, Menard C, Hicks-Boucher W, Hopkins L, Weberpals J, Fung-Kee-Fung M. Final results of a phase 2 study using continuous 5% Imiquimod cream application in the primary treatment of high-grade vulva intraepithelial neoplasia. Gynecol Oncol 2007;106:579-84.
[Google Scholar]
|
Fulltext Views
2,661
PDF downloads
1,667





