Translate this page into:
Type D personality is associated with poor quality of life, social performance, and psychological impairment in patients with moderate to severe psoriasis: A cross-sectional study of 130 patients
2 Department of Dermatology, University of Granada, Granada, Spain
Correspondence Address:
Alejandro Molina-Leyva
Department of Dermatology, Virgen de las Nieves Hospital, Madrid Avenue, 15, PC 18014 Granada
Spain
| How to cite this article: Aguayo-Carreras P, Ruiz-Carrascosa JC, Molina-Leyva A. Type D personality is associated with poor quality of life, social performance, and psychological impairment in patients with moderate to severe psoriasis: A cross-sectional study of 130 patients. Indian J Dermatol Venereol Leprol 2020;86:375-381 |
Abstract
Background: Psoriasis is a systemic autoinflammatory disease that is related to an increased risk of organic and psychological comorbidities. Type D personality has been related to poor quality of life and worse physical and psychological outcomes in different diseases.
Aims: The aim of this study is to explore whether type D personality is associated with an increased risk of presenting physical and/or psychological comorbidities, their relationship with the capacity of social adaptation, and health-related quality of life (HRQOL) in patients with psoriasis.
Methods: This was a cross-sectional study. In all, 130 patients with moderate to severe psoriasis were included in this study. Participants completed the DS14 test and different validated questionnaires regarding quality of life and psychological morbidities.
Results: Type D personality was present in 38.4% (50/130) of the participants of the study. Patients with psoriasis and type D personality presented a higher risk of depression and anxiety. We observed that type D personality was associated with a lower educational level. These patients also presented a worse HRQOL in different dimensions of the Short Form Health Survey-36 questionnaire, more sleep problems, poor social adaptation, and a higher frequency of sexual disturbances.
Limitations: Due to the cross-sectional design of the study, we could not confirm causality. Selection of sample was not random. Diagnoses of physical comorbidity were collected through clinical interview of patients under active treatment, which may imply a classification bias.
Conclusion: Type D personality could represent a frequent personality profile in patients with psoriasis that could identify subjects with poor coping abilities to the disease with poorer levels of quality of life, increased psychological comorbidities, and inadequate social adaptation mechanisms.
Introduction
Psychological factors including perceived health, perceptions of stigmatization, and depression are more important determinants of disability in patients with psoriasis than the severity of the disease, location, and duration.[1] How each individual faces his illness and establishes mechanisms of adaptation or coping is a complex process that depends on many factors, and one of the most important factors is personality.[2]
Personality effect, defined as a relatively permanent feature, is a measure of the stress produced by the environment and the onset, development, and course of somatic diseases.[3] It affects the process of stress management in two ways: directly, by restricting or helping coping strategies and indirectly, by influencing how the individual experiences the types and intensity of the stress factors.[4]
Type D personality consists of a tendency to inhibit the expression of emotions or behavior to avoid negative reactions from others [social inhibition (SI)], in combination with a stable tendency to experience negative affectivity (NA).[5] High NA individuals experience more feelings of dysphoria, anxiety, and irritability; have a negative view of self; and scan the world for signs of impending trouble. High SI individuals tend to feel inhibited, tense, and insecure when with others. Individuals who are high in both NA and SI have a distressed or type D personality, given their vulnerability to chronic distress.[1] The prevalence of type D personality in healthy subjects in several studies ranges between 20% and 23%.[2] This type of personality has been associated with an increase in cardiovascular risk and a worse health-related quality of life (HRQOL) in different types of pathologies, viz. in patients with cancer, atrial fibrillation, and acute myocardial infarction.[6],[7],[8],[9],[10],[11],[12] Recent studies have shown that people with type D personality have high levels of tumor necrosis factor-alpha (TNF-α), one of the key proinflammatory cytokines in the etiopathogenesis of psoriasis and in the development of cardiometabolic and psychological comorbidities.[8],[9],[10],[11],[12],[13]
The aim of this study is to evaluate the association between the presence of type D personality and the risk of presenting physical and/or psychological comorbidities and their relationship with their HRQOL.
Methods
Design and study population
This was a cross-sectional study. The study sample was consecutively recruited among patients with moderate to severe psoriasis who attended their scheduled follow-up visits at the psoriasis unit of the Hospital Universitario San Cecilio, Granada, Spain. The psoriasis unit serves all patients with moderate to severe psoriasis in our dermatology clinic. All participants provided informed consent to participate in the study. The ethics committee of the Hospital Universitario San Cecilio, Granada, Spain approved the study the 23th March 2013.
Our sample in the study is a representative sample of patients with psoriasis that we can find in a dermatology consultation, since it has been extracted from the psoriasis unit that attends all patients with moderate to severe psoriasis in the dermatology clinic with a reference population of 450,000 inhabitants.
Inclusion and exclusion criteria
The inclusion criteria were as follows: diagnosis of moderate to severe cutaneous psoriasis, age 18 years or older, and granted informed consent.
The severity of psoriasis was assessed according to the most recent version of the consensus document of the Spanish Academy of Dermatology.[14]
“Moderate to severe psoriasis: requires (or has previously required) systemic treatment (including conventional drugs, biological agents or photochemotherapy). Systemic treatment is indicated in patients with psoriasis in the following situations: (a) disease not controlled with topical treatments; (b) extensive disease (BSA >5%–10%); (c) PASI >7–15; (d) rapid worsening; (e) involving visible areas; (f) functional impairment (palmoplantar, nail, genital or scalp involvement); (g) subjective perception of severity (DLQI >6–10); (h) extensive erythroderma or pustular psoriasis; and (i) disease associated with psoriatic joint disease.”
Exclusion criteria were as follows: refusal to participate in the study, active dermatological diseases other than psoriasis, treatment with psychoactive drugs, intellectual disability, active malignant disease, and alcohol abuse.
Main endpoints of interest and sources of information
Our main variable of interest was the presence of type D personality assessed by the questionnaire DS14, validated in Spanish population and widely used for this purpose.[5] It consists of 14 items, 7 in relation to negative affection and 7 in relation to SI. Each item is scored from 0 to 4. The presence of type D personality is defined as scores equal to or greater than 10 in both subscales. DS14 has been translated into different languages and has demonstrated high reliability and internal consistency. The Spanish version of DS14 presents adequate psychometric properties with alpha coefficient of Cronbach values higher than 0.80 in the scale of negative affection and SI.[15]
Sociodemographic data and biometric parameters were collected through clinical interviews and physical examinations. Three physical comorbidities were considered for the analysis: arterial hypertension, dyslipidemia, and diabetes mellitus. For the purposes of this study. the diagnoses were only considered when the patient received active treatment. A trained dermatologist assessed the severity of psoriasis by clinical interview, physical examination, review of medical records, calculation of body surface area (BSA) affected by psoriasis, and Psoriasis Area and Severity Index (PASI).[16]
The Hospital Anxiety and Depression Scale (HADS) was used to evaluate anxiety and depression levels.[17] HADS is a self-administered questionnaire that has been validated in the Spanish population.[18] The questionnaire consists of 14 items divided into two scales of seven items each. The strength of the symptom is evaluated on a 4-point Likert scale from 0 to 3. Scores on the subscales higher than 7 are considered to indicate signs of anxiety or depression, and scores higher than 10 are considered to indicate a clinical problem. Using these cut-offs, we consider the prevalence of anxiety and/or depression for scores above 7.
The Self-Applied Scale of Social Adaptation (SASS) evaluates the perspective of the individual about himself/herself and the environment, as well as his/her behavior and social motivation. This scale consists of 21 items, with four response levels (from 0 to 3), which evaluate motivation and social behavior. The items explore the functioning of the individual in different areas: work, family, leisure, social relations, and motivation/interests. The total score range is between 0 and 60.[19] Since it is a binary scale, levels under 2 were considered as poor social adaptation.
Fagerström (FT) test is used to evaluate the degree of physical dependence on nicotine. It consists of six items with two or four response alternatives. The score oscillates between 0 and 10. High scores in the FT test (6 or more) indicate a high degree of dependence.[20]
The Short Form Health Survey (SF-36) in its standard version was used to determine HRQOL.[21],[22],[23] The SF-36 consists of 36 items that conform eight domains: physical function, physical role, body pain, general health, vitality, social function, emotional role, and mental health.[24] Scores range from 0 to 100, 100 being the best possible state of health and 0 the worst. The questionnaire has been validated in several populations, including the Spanish one.[25]
The SF-36 questionnaire does not collect information on sexual function, for which reason the Massachusetts General Hospital-Sexual Functioning Questionnaire (MGH-SFQ) was used. MGH-SFQ is a self-administered questionnaire designed to detect sexual dysfunction and has been validated in the Spanish population.[26] The questionnaire consists of five items that address the different phases of the sexual cycle: sexual interest, sexual arousal, erection (only male), orgasm, and global sexual satisfaction. Each item is rated from 0 (completely reduced) to 4 (normal). High scores indicate better sexual functioning. Sexual dysfunction is considered when at least one item yields a score <4.
The Psoriasis Disability Index (PDI) is a specific questionnaire to assess HRQOL of patients with psoriasis.[27] It consists of 15 items divided into five dimensions: daily activities (five items), work/studies (three items), relationships (two items), leisure (four items), and treatment (one item). The response category ranges from 0 (no interference of psoriasis) to 3 (maximum interference of psoriasis), and the total score range is from 0 to 45 (the higher the score, the greater the impact on the quality of life). The results can be transformed into a percentage scale from 0 to 100, where 100 indicates a maximum involvement of the HRQOL for psoriasis.[28]
Sample size
The study size was calculated to determine the proportion of patients with psoriasis and type D personality with an alpha error of 5% and a power of 20%; considering a reference population of 450,000 inhabitants, an estimated prevalence of psoriasis in general population of 3%,[19] and a prevalence of type D personality in patients with psoriasis of 38.7%,[3] the estimated sample size was 125 patients.
Data analysis
Descriptive statistics were used to explore the characteristics of the patients. Continuous data are expressed as mean and standard deviation. The absolute and relative frequency distributions were estimated for qualitative variables. Mann–Whitney U-test was performed to compare quantitative data between psoriatic patients with type D personality and without type D personality. Chi-square test or Fisher's exact test when necessary was used for qualitative variables. Significance was set at P < 0.05. Odds ratios with 95% confidence intervals were computed by logistic regression to explore factors associated with type D personality. The main outcome of interest, type D personality, was binary codified as either type D personality (DS14 score equal to more than 10 on both scales, SI and NA) or no type D personality (DS14 score <10).[5]
Results
A total of 154 patients with moderate to severe psoriasis were invited to join the study. Twenty-one patients did not meet the inclusion criteria and were excluded. Three questionnaires were excluded because they were incomplete. Therefore, all analyses were performed in 130 patients. [Table - 1] summarizes the main sociodemographic and clinical characteristics of the study participants.
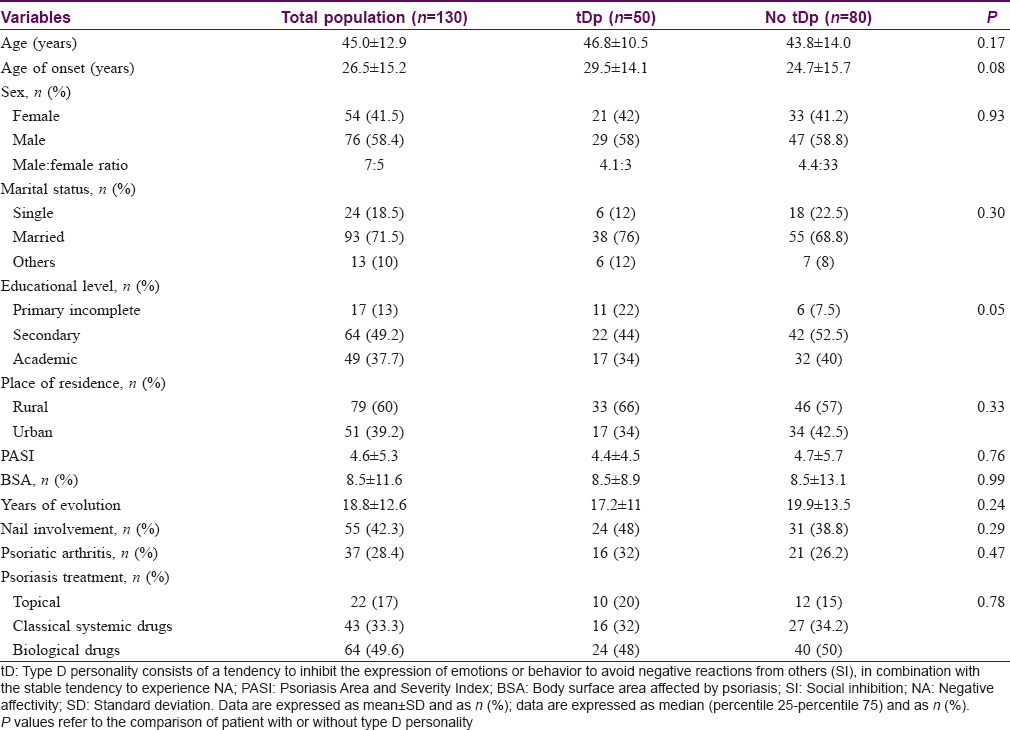
According to DS14 questionnaire, 38.4% (50/130) of the patients presented with type D personality. The median of the SI scale was 9[6],[7],[8],[9],[10],[11],[12],[13] and the median of NA was 13.[8],[9],[10],[11],[12],[13],[14],[15],[16],[17] Abnormal SI scores were present in 48.5% (63/130) of the patients and 66.9% (87/130) showed abnormal NA scores. In relation to sociodemographic characteristics, we noted that type D personality was associated with a lower education level [Table - 1]. There were no differences regarding gender, marital status, or place of residence. No difference was observed as to the severity of psoriasis assessed by PASI and BSA, the type of treatment, or the presence of joint or nail involvement [Table - 1]. The components of the metabolic syndrome i.e. hypertension, obesity, dyslipidemia, and diabetes mellitus were not significantly different in patients with type D personality. The percentage of smokers was similar between the two groups, but the degree of dependence on nicotine was higher in patients with psoriasis and type D personality [Table - 2].
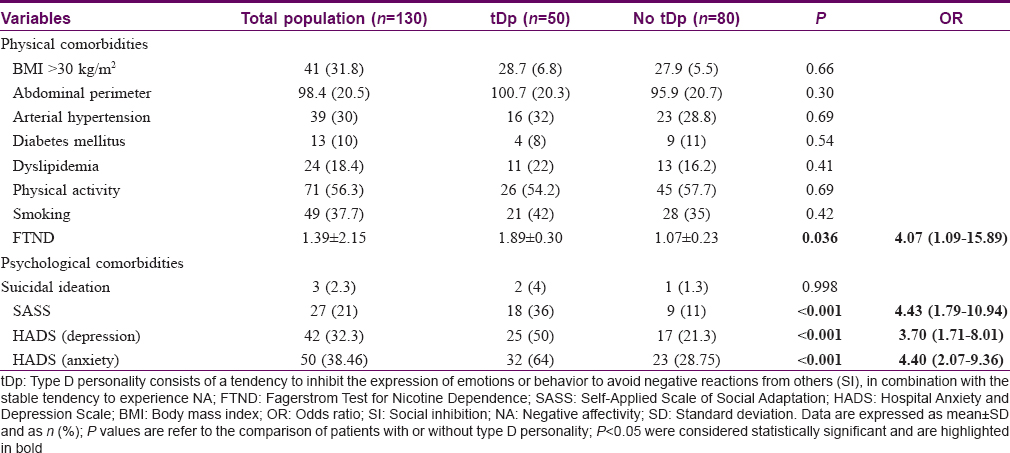
Regarding psychological and social features, patients with type D personality and psoriasis had a higher risk of anxiety and depression, and a higher frequency of insomnia of early awakening [Table - 2]. Social adaptation was poor in more than a third of patients with type D personality.
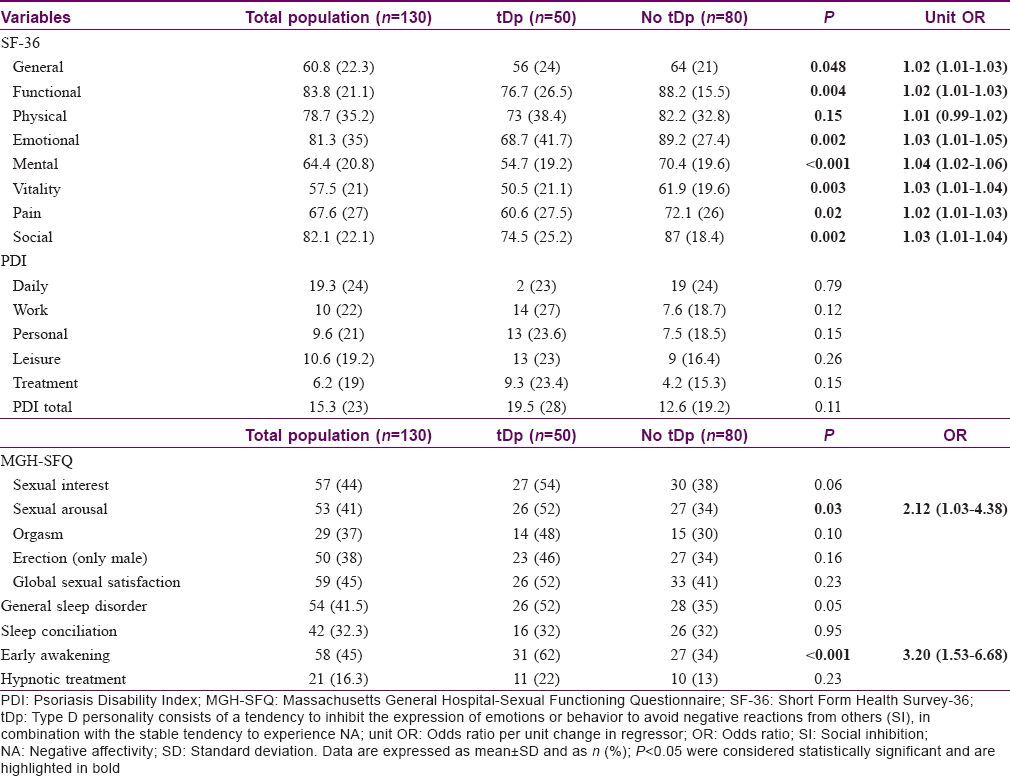
We noted in patients with psoriasis that type D personality was associated with a worse HRQOL in different dimensions of the SF-36, such as physical functionality, physical role, body pain, vitality, social functionality, emotional role, and mental health [Table - 3]. Finally, in relation to sexual health, patients with type D personality had a higher frequency of alterations in sexual interest than patients without type D personality.
Discussion
This study explores the relationship between type D personality in patients with moderate to severe psoriasis and its relationship with psychological and cardiovascular comorbidities, social adaptation, and impact on various aspects of HRQOL.
Recent investigations have shown an increased prevalence of type D personality in patients with psoriasis compared with healthy population being in a range of 25%–38.7%.[3],[20],[29] The results of our study show that type D personality could be more prevalent among patients with moderate to severe psoriasis and may impact different aspects of life and health.
First of all, according to the results of previous studies,[3],[30],[31] we found a significant increase in anxiety and depression in subjects with psoriasis and type D personality. Anxiety, stress, and cortisol, interrelated by the hypothalamus–pituitary–adrenal axis, are well-known aggravating factors for psoriasis. Subjects with type D personality and in particular their negative affection subcomponent are more likely to experience negative emotions, depression, anxiety, hostility, irritability, lower levels of self-confidence, and more use of resignation or withdrawal coping.[2] The presence of type D personality could increase the impact of perceived stigmatization due to psoriasis and is related to a greater feeling of impotence regarding the disease.[29] In line with this observation, the results of SASS showed worse social abilities in patients with psoriasis and type D personality, and these could have important implications. Poor social adaptation leads to poor psychological health and emotional status and makes patients more prone to sedentarism and unhealthy lifestyles. In fact, we observed a higher nicotine dependence in patients with type D personality. Smoking is a frequent toxic habit in patients with psoriasis that impairs cardiovascular health. Nicotine alters a wide range of immunologic functions that can affect the pathogenesis of psoriasis. Innate and adaptive immune responses can be altered through activation of T cells and excessive production of inflammatory cytokines, including several interleukins and TNF-α.[30],[31]
Type D personality also contributes to worse sleep quality probably linked to disturbances in mood status. Personality has been determined as a significant predictor of sleep disturbance.[32] Literature concerning personality concurs that individuals with insomnia exhibit increased neuroticism, internalization, anxious concerns, and negative components of perfectionism.[33] Also, early awakening insomnia has been associated with depression. Quality of sleep is crucial to general health, not only essential for the optimal performance of physical, cognitive, and emotional process but also a vital biological determinant of everyday health and well-being.[34]
With regard to HRQOL, we noted that type D personality was associated with lower levels of HRQOL. Although no differences were found in the scores of the PDI scale, worse scores were obtained in physical function, physical role, body pain, vitality, social function, emotional role, and mental health in type D personality patients. In relation to sexual health, patients with psoriasis and type D personality had up to two times lower sexual desire without significant differences with regard to sexual interest, erectile dysfunction, orgasm, or global sexual satisfaction in MGH-SFQ. Therefore, type D personality could be a major determinant of HRQOL, regardless of mood.
Type D personality has been proposed as an independent risk factor of cardiovascular disease among different diseases and healthy population.[9],[10],[11],[35] We did not assess major cardiovascular events in our sample. We did not find any association between type D personality and metabolic syndrome in our sample, which has been proposed as a major contributor to cardiovascular risk in patients with psoriasis. Whether type D personality independently influences the cardiovascular risk of patients with psoriasis should be assessed in larger studies.
A proinflammatory state in the cytokine network plays an important role in the pathogenesis of psoriasis, and within them, mediators such as TNF-α and IL-17 play key roles. Type D personality has been associated with elevated levels of TNF-α, TNF-α receptors, and sTNFR2.[3],[13] This study found no difference in the severity of the disease or in the proportion of patients with biological treatment in the group of patients with type D personality. Both type D personality and psoriasis, depending on elements such as the age of onset of psoriasis, could be cause and consequence of each other. Personality is a complex construct, modulated by genes and life experiences. Because of the design of this study, we were unable to test this hypothesis. Future studies in the field of neuropsychology and dermatology are needed to explore these complex relationships.
The methodological limitations of this study can be summed up as follows: (i) Due to the cross-sectional design of the study, we included prevalent psoriasis cases and could not confirm causality. (ii) Selection of sample was not random. (iii) Diagnoses of physical comorbidity were collected through clinical interview of patients under active treatment, which may imply a classification bias.
Conclusion
Type D personality is a frequent type of personality among patients with psoriasis. It increases the risk of anxiety and depression, favors poor social adaptation, and confers a worse quality of life related to the health of these patients. Type D personality could represent a trait associated with poor coping abilities in patients with psoriasis and its screening could be helpful to identify subgroups that may benefit from interdisciplinary interventions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Acknowledgement
The results of this study are part of PhD work of Paula Aguayo-Carreras.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Basavaraj KH, Navya MA, Rashmi R. Stress and quality of life in psoriasis: An update. Int J Dermatol 2011;50:783-92.
[Google Scholar]
|
| 2. |
Borkoles E, Kaiseler M, Evans A, Ski CF, Thompson DR, Polman RC. Type D personality, stress, coping and performance on a novel sport task. PLoS One 2018;13:e0196692.
[Google Scholar]
|
| 3. |
Molina-Leyva A, Caparros-delMoral I, Ruiz-Carrascosa JC, Naranjo-Sintes R, Jimenez-Moleon JJ. Elevated prevalence of type D (distressed) personality in moderate to severe psoriasis is associated with mood status and quality of life impairment: A comparative pilot study. J Eur Acad Dermatol Venereol 2015;29:1710-7.
[Google Scholar]
|
| 4. |
Bolger N, Zuckerman A. A framework for studying personality in the stress process. J Pers Soc Psychol 1995;69:890-902.
[Google Scholar]
|
| 5. |
Denollet J. DS14: Standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med 2005;67:89-97.
[Google Scholar]
|
| 6. |
Mols F, Holterhues C, Nijsten T, van de Poll-Franse LV. Personality is associated with health status and impact of cancer among melanoma survivors. Eur J Cancer 2010;46:573-80.
[Google Scholar]
|
| 7. |
Mols F, Thong MS, de Poll-Franse LV, Roukema JA, Denollet J. Type D (distressed) personality is associated with poor quality of life and mental health among 3080 cancer survivors. J Affect Disord 2012;136:26-34.
[Google Scholar]
|
| 8. |
Hausteiner C, Klupsch D, Emeny R, Baumert J, Ladwig KH; KORA Investigators. Clustering of negative affectivity and social inhibition in the community: Prevalence of type D personality as a cardiovascular risk marker. Psychosom Med 2010;72:163-71.
[Google Scholar]
|
| 9. |
Mols F, Martens EJ, Denollet J. Type D personality and depressive symptoms are independent predictors of impaired health status following acute myocardial infarction. Heart 2010;96:30-5.
[Google Scholar]
|
| 10. |
Romppel M, Herrmann-Lingen C, Vesper JM, Grande G. Type D personality and persistence of depressive symptoms in a German cohort of cardiac patients. J Affect Disord 2012;136:1183-7.
[Google Scholar]
|
| 11. |
Svansdottir E, Denollet J, Thorsson B, Gudnason T, Halldorsdottir S, Gudnason V, et al. Association of type D personality with unhealthy lifestyle, and estimated risk of coronary events in the general Icelandic population. Eur J Prev Cardiol 2013;20:322-30.
[Google Scholar]
|
| 12. |
Son YJ, Song EK. The impact of type D personality and high-sensitivity C-reactive protein on health-related quality of life in patients with atrial fibrillation. Eur J Cardiovasc Nurs 2012;11:304-12.
[Google Scholar]
|
| 13. |
Conraads VM, Denollet J, De Clerck LS, Stevens WJ, Bridts C, Vrints CJ. Type D personality is associated with increased levels of tumour necrosis factor (TNF)-alpha and TNF-alpha receptors in chronic heart failure. Int J Cardiol 2006;113:34-8.
[Google Scholar]
|
| 14. |
Llamas-Velasco M, de la Cueva P, Notario J, Martínez-Pilar L, Martorell A, Moreno-Ramírez D. Moderate psoriasis: A proposed definition. Actas Dermosifiliogr 2017;108:911-7.
[Google Scholar]
|
| 15. |
Alcaraz SH, Godoy C, Fernández E. Spanish validation of the type D personality scale (DS14). Behav Psychol 2018;26:195-209.
[Google Scholar]
|
| 16. |
Robinson A, Kardos M, Kimball AB. Physician global assessment (PGA) and psoriasis area and severity index (PASI): Why do both? A systematic analysis of randomized controlled trials of biologic agents for moderate to severe plaque psoriasis. J Am Acad Dermatol 2012;66:369-75.
[Google Scholar]
|
| 17. |
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70.
[Google Scholar]
|
| 18. |
Navinés R, Castellví P, Moreno-España J, Gimenez D, Udina M, Cañizares S, et al. Depressive and anxiety disorders in chronic hepatitis C patients: Reliability and validity of the patient health questionnaire. J Affect Disord 2012;138:343-51.
[Google Scholar]
|
| 19. |
Springate DA, Parisi R, Kontopantelis E, Reeves D, Griffiths CE, Ashcroft DM. Incidence, prevalence and mortality of patients with psoriasis: A U.K. population-based cohort study. Br J Dermatol 2017;176:650-8.
[Google Scholar]
|
| 20. |
Basińska MA, Woźniewicz A. The relation between type D personality and the clinical condition of patients suffering from psoriasis. Postepy Dermatol Alergol 2013;30:381-7.
[Google Scholar]
|
| 21. |
Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473-83.
[Google Scholar]
|
| 22. |
McHorney CA, Ware JE Jr., Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993;31:247-63.
[Google Scholar]
|
| 23. |
McHorney CA, Ware JE Jr., Lu JF, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 1994;32:40-66.
[Google Scholar]
|
| 24. |
Sampogna F, Tabolli S, Söderfeldt B, Axtelius B, Aparo U, Abeni D. Measuring quality of life of patients with different clinical types of psoriasis using the SF-36. Br J Dermatol 2006;154:844-9.
[Google Scholar]
|
| 25. |
Alonso J, Prieto L, Antó JM. The Spanish version of the SF-36 health survey (the SF-36 health questionnaire): An instrument for measuring clinical results. Med Clin (Barc) 1995;104:771-6.
[Google Scholar]
|
| 26. |
Sierra JC, Vallejo-Medina P, Santos-Iglesias P, Lameiras Fernández M. Validation of Massachusetts general hospital-sexual functioning questionnaire (MGH-SFQ) in a Spanish population. Aten Primaria 2012;44:516-24.
[Google Scholar]
|
| 27. |
Finlay AY, Khan GK, Luscombe DK, Salek MS. Validation of sickness impact profile and psoriasis disability index in psoriasis. Br J Dermatol 1990;123:751-6.
[Google Scholar]
|
| 28. |
Vanaclocha F, Puig L, Daudén E, Escudero J, Hernanz JM, Ferrándiz C, et al. Validation of the Spanish version of the psoriasis disability index questionnaire in assessing the quality of life of patients with moderate-severe psoriasis. Actas Dermosifiliogr 2005;96:659-68.
[Google Scholar]
|
| 29. |
van Beugen S, van Middendorp H, Ferwerda M, Smit JV, Zeeuwen-Franssen ME, Kroft EB, et al. Predictors of perceived stigmatization in patients with psoriasis. Br J Dermatol 2017;176:687-94.
[Google Scholar]
|
| 30. |
La Vecchia C, Gallus S, Naldi L. Tobacco and skin disease. Dermatology (Basel, Switzerland) 2005;211:81-3.
[Google Scholar]
|
| 31. |
Setty AR, Curhan G, Choi HK. Smoking and the risk of psoriasis in women: Nurses' health study II. Am J Med 2007;120:953-9.
[Google Scholar]
|
| 32. |
Schiffer AA, Pedersen SS, Widdershoven JW, Hendriks EH, Winter JB, Denollet J. The distressed (type D) personality is independently associated with impaired health status and increased depressive symptoms in chronic heart failure. Eur J Cardiovasc Prev Rehabil 2005;12:341-6.
[Google Scholar]
|
| 33. |
Akram U, McCarty K, Akram A, Gardani M, Tan A, Villarreal D, et al. The relationship between type D personality and insomnia. Sleep Health 2018;4:360-3.
[Google Scholar]
|
| 34. |
Allen SF, Elder GJ, Longstaff LF, Gotts ZM, Sharman R, Akram U, et al. Exploration of potential objective and subjective daily indicators of sleep health in normal sleepers. Nat Sci Sleep 2018;10:303-12.
[Google Scholar]
|
| 35. |
Svansdottir E, Karlsson HD, Gudnason T, Olason DT, Thorgilsson H, Sigtryggsdottir U, et al. Validity of type D personality in Iceland: Association with disease severity and risk markers in cardiac patients. J Behav Med 2012;35:155-66.
[Google Scholar]
|
Fulltext Views
5,121
PDF downloads
2,402





