Translate this page into:
Comparison of direct microscopic methods using potassium hydroxide, periodic acid Schiff, and calcofluor white with culture in the diagnosis of onychomycosis
2 Department of Microbiology, Safdarjang Hospital and VMMC, New Delhi, India
Correspondence Address:
Sachin Yadav
Department of Dermatology and STD, Safdarjang Hospital and VMMC, New Delhi
India
| How to cite this article: Yadav S, Saxena A K, Capoor MR, Ramesh V. Comparison of direct microscopic methods using potassium hydroxide, periodic acid Schiff, and calcofluor white with culture in the diagnosis of onychomycosis. Indian J Dermatol Venereol Leprol 2013;79:242-243 |
Sir,
Onychomycosis is the most common cause of abnormal nails (more than 50%). [1] Given the differential diagnosis of dystrophic nails, it is important to obtain a definitive diagnosis of fungal infection before initiation of therapy. Potassium hydroxide (KOH), which is routinely used for staining mycological specimens, often yields false-negative results. [2] It has been reported that periodic acid Schiff (PAS) and calcofluor white (CW) might be useful stains in diagnosing fungal elements with high positivity rate. [2],[3] The purpose of this study was to compare KOH preparation, KONCPA (KOH-treated nail clippings + periodic acid Schiff) technique, and fluorescent microscopy using CW, with culture in the diagnosis of onychomycosis.
An open prospective study was conducted on patients attending outpatient department of dermatology in our hospital, between November 2009 and October 2010. Patients with clinical features of onychomycosis were evaluated. Those who had taken systemic antifungal treatment within last 9 months or who did not demonstrate fungal elements in direct microscopy and/or culture, in repeat sample also, were excluded.
After disinfecting with 70% alcohol, nail scrapings and subungual debris were obtained from affected areas with the sterile no. 15 scalpel blade. In KOH mount, a portion of nail specimen was incubated in 20% KOH overnight at room temperature. The softened nail material was gently crushed with cover slip to form a thin film over a clean glass slide and was examined microscopically for fungal elements. In KONCPA method, specimens were treated with 20% KOH at 56°C for 30 min and washed with isotonic sodium chloride solution. Specimens were then centrifuged at 3000 rpm for 5 min and sediment was crushed to form a thin film over the slide. Then, the film was stained with PAS and visualized under microscope. In fluorescent microscopy, KOH treated nail material was stained with fluorescent brightener, CW, on a glass slide and fungal elements were examined under fluorescent microscope. The rest of nail specimens were inoculated on Sabouraud′s dextrose agar medium with 0.05% chloramphenicol, with and without 0.5% cycloheximide for 4 weeks. The growth was identified by its cultural characteristics on media and sporulation pattern on lactophenol cotton. For pathogenic non-dermatophyte mold, the diagnosis required presence of hyphae in direct microscopy and isolation of same mold in primary and repeat nail sample.
Sixty-two patients had at least one of the four diagnostic methods positive for the presence of fungal elements. The positive rates of KOH preparation, KONCPA, fluorescent microscopy, and culture were 66.1%, 61.3%, 79.0%, and 75.8%, respectively. Considering culture as gold standard, sensitivity, specificity, positive predictive value, and negative predictive value were calculated for each microscopic method. The results are shown in [Table - 1].
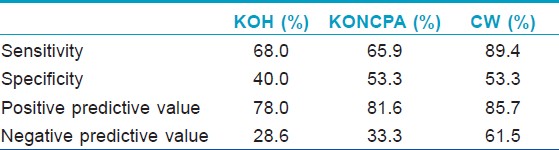
The common methods used for the diagnosis of onychomycosis are fungal culture on Sabouraud′s dextrose agar and KOH staining of nail sample. Culture was taken as gold standard test because of its high specificity and ability to identify species of invading pathogens. [2],[4],[5] The isolation rate of fungus on culture can be improved by taking enough nail sample from the most proximal affected area. KOH mount is a rapid, simple, and inexpensive method for diagnosis of fungal infections. The sensitivity of KOH preparations was 68% in this study. The different sensitivity rates reported earlier are 80%, [2] 55%, [4] 92%, [5] and 32%. [6] The false-negative results occur because of low visibility of scattered scanty fungal material obtained from the nail scraping and inadequate skill of observer in detection of fungal element. [4] Specificity of KOH preparations was found to be lower (40%). Artifacts including lipid vesicles, air bubbles, textile fibers, and mosaic fungus result in false-positivity. [7]
In KONCPA technique, PAS stain demonstrates the presence of certain polysaccharides, specifically glycogen and mucoproteins, as reddish structures which are present in the walls of the fungal hyphae. KONCPA showed sensitivity of 65.9% in our laboratory, which is lower than that reported in previous studies. [2],[4],[5] The lower detection was due to loss of major portion of KOH treated nail sample while washing with sodium chloride solution during the procedure. The false-positive results occur due to red staining of non-fungal structures like starch particles, serum remnants, and parakeratotic cells. [8]
Fluorescent microscopy showed high sensitivity of 89.4%, which was also noted in earlier reports. [2],[3],[5] This method is rapid and easy to perform. Fluorescent brighteners like CW specifically bind to cellulose and chitin, which are the major components in the cell wall of fungi. The dye then fluoresces as it is exposed to UV radiation on fluorescent microscopy. This helps in easy visualization of fungal elements. The constraint with this method is availability of fluorescent microscope and fluorescent dye. To conclude, the present study shows that CW microscopy gives significantly higher rates of detection of onychomycosis compared to the other microscopic methods using KOH and PAS stain.
| 1. |
Welsh O, Vera-Cabrera L, Welsh E. Onychomycosis. Clin Dermatol 2010;28:151-9.
[Google Scholar]
|
| 2. |
Weinberg JM, Koestenblatt EK, Tutrone WD, Tishler HR, Najarian L. Comparison of diagnostic methods in the evaluation of onychomycosis. J Am Acad Dermatol 2003;49:193-7.
[Google Scholar]
|
| 3. |
Kwon KS, Yim CS, Jang HS, Oh CK, Chung TA. A Comparative Study for Diagnosing Onychomycosis Using KOH Smear, Fungal Culture, KONCPA and Fungi-Fluor(R) Stain. Korean J Med Mycol 1998;3:125-131.
[Google Scholar]
|
| 4. |
Panasiti V, Borroni RG, Devirgiliis V, Rossi M, Fabbrizio L, Masciangelo R, et al. Comparison of diagnostic methods in the diagnosis of dermatomycoses and onychomycoses. Mycoses 2006;49:26-9.
[Google Scholar]
|
| 5. |
Haghani I, Fathi M, Abedian S, Shokouhi T, Yazdani J. Comparison of diagnostic methods in the evaluation of onychomycosis. Cell J 2011;12:29-30.
[Google Scholar]
|
| 6. |
Lawry MA, Haenke E, Strobeck K, Martin S, Zimmer B, Romano PS. Methods for diagnosing onychomycosis: A comparative study and review of literature. Arch Dermatol 2000;136:1112-6.
[Google Scholar]
|
| 7. |
Baran R, Hay R, Haneke E, Tosti E, editors. Onychomycosis: The current approach to diagnosis and therapy. 2 nd ed. London: Informa Healthcare; 2006.
[Google Scholar]
|
| 8. |
Pierard GE, Quatresooz P, Arresse JE. Spot light on histomycology. Dermatol Clin 2006;24:371-4.
[Google Scholar]
|
Fulltext Views
2,934
PDF downloads
1,049





