Translate this page into:
A case of ultraviolet B-induced linear IgA bullous dermatosis
Correspondence Address:
Ying Wang
Department of Dermatology, Changhai Hospital, Second Military Medical University, Shanghai 200433
China
| How to cite this article: Gong Y, Bi XL, Wang Y, Gu J. A case of ultraviolet B-induced linear IgA bullous dermatosis. Indian J Dermatol Venereol Leprol 2014;80:67-68 |
Sir,
Linear IgA bullous dermatosis (LABD) may be induced by infections, malignancies and especially medications, although most cases are idiopathic. [1] However LABD induced by ultraviolet (UV) radiation has been reported rarely.
A 51-year-old man presented with a 3-month history of generalized pruritic papules, vesicles and bullae, involving his scalp, trunk and both dorsal lower extremities. Three months ago, he first noticed pruritic eruption on his scalp and shoulder-back after a period of intense sun-exposure when traveling abroad. Then the patient was treated as eczema in a hospital with oral mizolastine and topical clobetasol for 3 weeks, without any improvement in the lesions. A month later, grouped papules, vesicles and crusts appeared. The patient was healthy without any other disease or any drug exposure. Physical examination revealed combination of annular and grouped papules, vesicles, and bullae that were scattered symmetrically on the scalp, trunk and extremities including elbows scapular, and sacral areas. In addition there were multiple confluent vesicles, bullae, and crusts on the dorsal surfaces of both legs [Figure - 1]b. On the back, some blisters were seen to cluster around a resolving lesion [Figure - 1]a.
 |
| Figure 1: (a) Erythematous plaques with grouped vesicles, bullae and crusts which coalesce in a ring around resolving lesions on the back, before treatment; (b) erythematous plaques with grouped vesicles and bullae on extensor surfaces of the lower leg; (c and d) the lesions on the back and legs after 2 weeks of treatment |
Biopsy specimens were obtained from lesions on the dorsal aspect of the right leg, and histopathological examination showed sub-epidermal blisters with a dermal inflammatory cell infiltrate, composed predominantly of eosinophils, neutrophils [Figure - 2]a. Direct immunofluorescence studies revealed a continuous strong linear deposition of IgA along the basement membrane zone [Figure - 2]b. Nothing abnormal was detected on routine laboratory examination. After the diagnosis of LABD was established, the patient was administered methylprednisolone intravenously (1 mg/kg/d) for 14 days. The lesions improved significantly [Figure - 1]c and d. Thereafter, the patient reduced the dosage slowly for 2 months and all the lesions resolved.
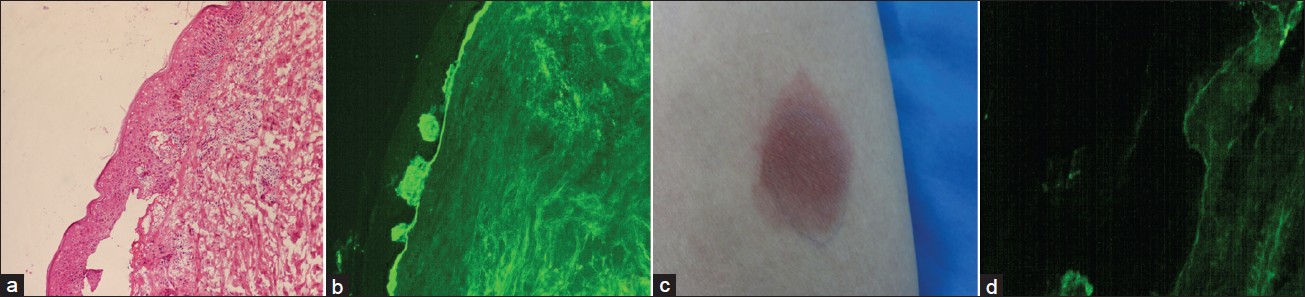 |
| Figure 2: (a) Histopathologic examination showing subepidermal blisters with dermal inflammatory cell infiltrate (H and E, ×20); (b) direct immunofluorescence of perilesional skin showing continuous linear deposits of immunoglobulin A at the basement membrane zone (×40); (c) the lesions of the extensor forearm skin after suberythematogenic photoprovocation with ultraviolet B (UVB) radiation for 4 days; (d) direct immunofluorescence fi ndings of the lesions induced by UVB radiation (×40) |
One month later, phototesting of clinically unaffected skin on the right arm was performed for UVA and UVB to determine the individual minimal erythema dose (MED) and to identify whether the UVA or UVB light was responsible for induction blister formation. The skin was exposed to a sunlight system (SUV-1000, sigma, Shanghai) and the MED was tested. The MED for UVA was more than 40 J/cm 2 , and the MED for UVB was 18.45 mJ/cm 2 , which showed that UVA-MED, was within the normal ranges, but the UVB-MED was not. We used photo-provocation with UVB radiation on 4 consecutive days with 18.45 mJ/cm 2 each day, which caused erythema in the irradiated areas [Figure - 2]c. On DIF examination, the UVB-induced erythema had features identical to those of the biopsy specimen from the perilesional skin on the dorsal aspect of the right leg, which also showed a linear deposition of IgA along the BMZ [Figure - 2]d.
LABD is a chronic acquired autoimmune sub-epidermal blistering disease characterized by a linear deposition of IgA along the BMZ. It is not a very common disease and occurs predominantly in children (<5 years old) and seniors (>60 years old). In adults, LABD mainly affects extensor surfaces, trunk, buttocks, and face (mostly the perioral area). [2]
LABD may be triggered by drugs, infections, malignancies, and autoimmune diseases in some cases. However, the role of UV radiation in LABD has been reported rarely. [3],[4] Our patient was not exposed to trauma, infection, tumors or radiation. But he had a period of intense sun exposure while traveling abroad. The blisters initially appeared on sun-exposed areas of the body. Suberythematogenic photo provocation with UVB radiation on 4 consecutive days caused erythema at the UVB-MED irradiated areas. Furthermore, the result of DIF of the erythema induced by UVB was similar to the lesions of LABD. Hence, we think the cause of LABD in our case is closely associated with UVB though the possible mechanisms of action are not understood.
Though dapsone is the best option for systemic therapy, [5] in our country, dapsone can be prescribed only for those who are suffering from leprosy. Our patient improved with methylprednisolone 1 mg/kg/d for 2 weeks. He had been in remission for 9 months, but the lesions reappeared after a period of intense sun-exposure, so we used hydroxychloroquine 200 mg/d and methylprednisolone 30 mg/d for treatment and advised the patient to keep out of the sun. His lesions improved and he is still being followed-up.
| 1. |
Dellavalle RP, Burch JM, Tayal S, Golitz LE, Fitzpatrick JE, Walsh P. Vancomycin-associated linear IgA bullous dermatosis mimicking toxic epidermal necrolysis. J Am Acad Dermatol 2003;48:S56-7.
[Google Scholar]
|
| 2. |
Fortuna G, Marinkovich MP. Linear immunoglobulin a bullous dermatosis. Clin Dermatol 2012;30:38-50.
[Google Scholar]
|
| 3. |
Salmhofer W, Soyer HP, Wolf P, Födinger D, Hödl S, Kerl H. UV light-induced linear IgA dermatosis. J Am Acad Dermatol 2004;50:109-15.
[Google Scholar]
|
| 4. |
He C, Xu H, Xiao T, Geng L, Chen HD. Localized linear IgA dermatosis induced by UV light-treatment for herpes zoster. Int J Dermatol 2007;46:500-2.
[Google Scholar]
|
| 5. |
Wojnarowska F. Linear IgA dapsone responsive bullous dermatosis. J R Soc Med 1980;73:371-3.
[Google Scholar]
|
Fulltext Views
2,904
PDF downloads
3,094





