Translate this page into:
A study of the histopathology of palmo-plantar psoriasis and hyperkeratotic palmo-plantar dermatitis
Correspondence Address:
Sujay Khandpur
4th Floor, Teaching Block, All India Institute of Medical Sciences, New Delhi - 110 029
India
| How to cite this article: Rao A, Khandpur S, Kalaivani M. A study of the histopathology of palmo-plantar psoriasis and hyperkeratotic palmo-plantar dermatitis. Indian J Dermatol Venereol Leprol 2018;84:27-33 |
Abstract
Background and Objectives: Palmo-plantar psoriasis and dermatitis show several overlapping clinical features. We undertook this retrospective study to elucidate and compare the histological findings in these two dermatoses.Materials and Methods: Biopsies of 31 clinically diagnosed cases of palmo-plantar psoriasis and 24 cases of hyperkeratotic palmo-plantar dermatitis, with concomitant presence of representative lesions at other body sites, were retrieved and analysed.
Results: Histologically, confluent parakeratosis, suprapapillary thinning and dermal edema were observed in significantly greater number of palmo-plantar psoriasis biopsies while an inflammatory infiltrate confined to the papillary dermis only, was a significant feature in palmo-plantar dermatitis. The two conditions could not be differentiated on the basis of features like focal parakeratosis, presence of neutrophils and fibrin globules in the stratum corneum, hypogranulosis, acanthosis, spongiosis, rete ridge pattern, or vascularity.
Conclusion: Histopathology of palmo-plantar psoriasis and dermatitis can have several overlapping features. In our study, we found only few features as strong pointers towards psoriasis.
Introduction
Psoriasis is a common relapsing chronic inflammatory dermatosis that affects about 1.53% of the general population and produces significant morbidity.[1] Palmo-plantar psoriasis is its localized form that can exist alone in the absence of other typical psoriatic lesions or may accompany psoriatic lesions elsewhere.[2],[3],[4],[5] A close clinical differential diagnosis of palmo-plantar psoriasis is hyperkeratotic palmo-plantar dermatitis. In situ ations when palmo-plantar sites are solely involved, diagnosis becomes particularly challenging. Both palmo-plantar psoriasis and dermatitis are recurrent diseases which interfere with daily activities.
The presence of sharply demarcated and symmetrically distributed erythematous plaques, silvery nature of scales, involvement of the thenar and hypothenar eminences and knuckles of hands and insteps of feet, with associated regular and coarse nail pits in the absence of nail-fold lesions, can be taken as features in favour of psoriasis, while ill-defined, usually asymmetrically distributed plaques, with history of prior exudation, suggest dermatitis.[6] However, there can be tremendous clinical overlap between the two conditions. Many a times, the histopathological findings are also similar.[7] A few histological features have been indicated in the literature as clues to the diagnosis of psoriasis in general, including neutrophilic abscesses-containing parakeratosis, thinning of the granular cell layer, neutrophils in the spinous layer and presence of tortuous capillaries in the papillary dermis.[7],[8],[9],[10] However there is paucity of literature comparing the histopathological features of palmo-plantar psoriasis and hyperkeratotic palmo-plantar dermatitis.
We undertook this study to elucidate and compare the histological findings in these two dermatoses.
Materials and Methods
We undertook a retrospective analysis of all biopsies obtained between 2012-2014 from patients diagnosed with palmo-plantar psoriasis and hyperkeratotic palmo-plantar dermatitis, who had attended the outpatient department of our institute. Group 1 included biopsies from palmo-plantar psoriasis cases who also had concomitant plaque psoriasis [Figure 1a] and [Figure 1b], [Figure 2a]. Presence of sharply demarcated erythematous plaques on palms and soles and similar erythematous plaques elsewhere on the body, covered with whitish semi-adherent scales without prior history of exudation from the plaques were the clinical criteria for psoriasis.
 |
| Figure 1a: A case of palmar psoriasis with well circumscribed keratotic plaques over bilateral palms |
 |
| Figure 1b: A case of palmar psoriasis with erythematous, scaly fissured plaques symmetrically distributed over both thenar and hypothenar eminences and palmar aspect of fingers |
 |
| Figure 2a: A case of plantar psoriasis showing erythematous scaly plaques on sole extending to lateral aspect of foot and with psoriatic plaques on dorsum of foot |
Group 2 included biopsies from hyperkeratotic palmo-plantar dermatitis lesions in patients with associated dermatitic plaques manifesting as exudative and lichenified pruritic lesions, involving other body sites [Figure 2b].
 |
| Figure 2b: A case of plantar dermatitis with erythematous scaly fissured plaque on left sole |
Other dermatological conditions that manifest with papulo-squamous lesions on the palms and soles such as hyperkeratotic tinea pedis/tinea mannum, pityriasis rubra pilaris or palmo-plantar keratoderma were excluded. Hematoxylin and eosin (H and E) stained sections were examined without looking at clinical information and details of histological findings were recorded. The histopathological findings of both the groups were compared.
Statistical analysis was carried out using Stata 11.0 (College station, Texas, USA). Data was presented as number (%) or Mean ± SD/Median (min-max) as appropriate. Continuous variables were compared between the groups using independent t- test/Wilcoxon Rank-sum test and categorical variables were compared between the group using Chi square test and Fischer's exact test. P value <0.05 was considered statistically significant.
Results
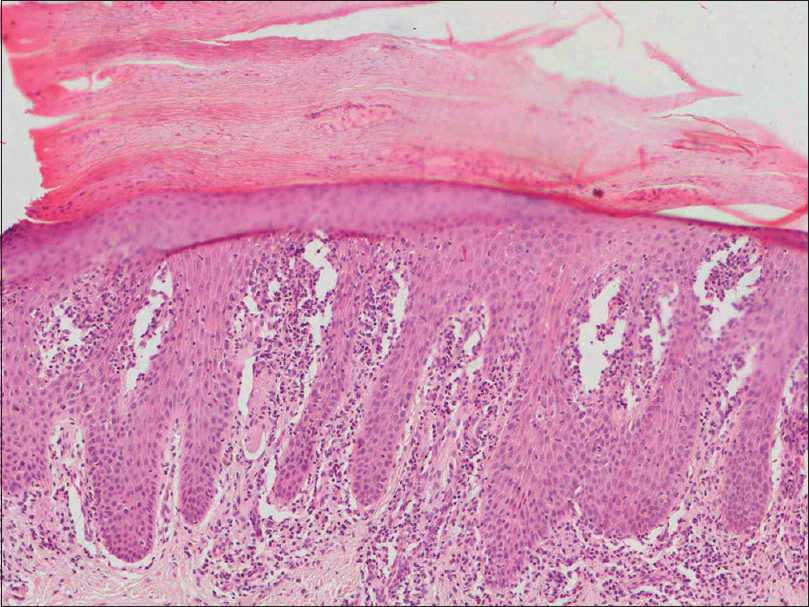
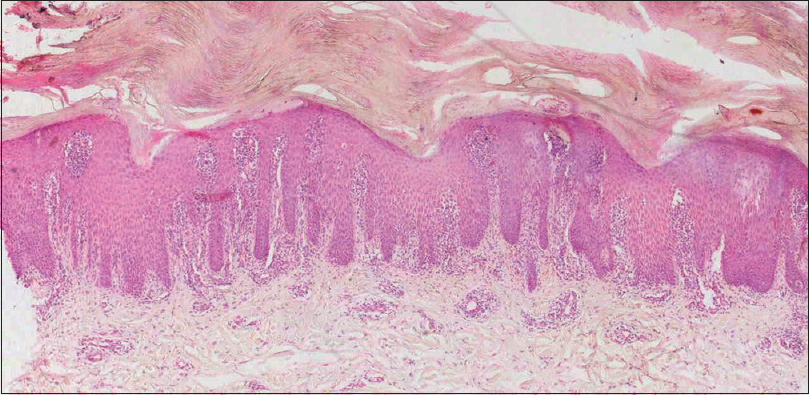
The results are summarized in [Table - 1]. A total of 55 biopsies were reviewed, which included 31 (56.4%) of palmo-plantar psoriasis {Group 1, mean age 40.03 ± 2.83 years (range 12-67 years) 21 men and 10 women} and 24 biopsies (43.6%) of hyperkeratotic palmo-plantar dermatitis {Group 2, mean age 33.6 ± 2.76 years (range 11-70 years), 8 men and 16 women}. On histological analysis, parakeratosis was present in 90.3% of palmo-plantar psoriasis and 62.5% of dermatitis biopsies [Figure 3a]. The difference was statistically significant (P = 0.021). Parakeratosis was focal in 22 (71%) and 15 cases (62.5%) in psoriasis [Figure 3b] and dermatitis respectively (P = 0.5) and confluent in 6 psoriasis cases only (19.4%) (P = 0.022) [Figure 4a] and [Figure 4b].
 |
| Figure 3a: Case of plantar dermatitis showing focal parakeratosis, fibrin globules in stratum corneum, irregular acanthosis, mild to moderate spongiosis, focal suprapapillary thinning, mild chronic infiltrate in dermal papilla and papillary dermis (H and E, ×40) |
 |
| Figure 3b: Case of palmar psoriasis showing focal parakeratosis, fibrin globules in stratum corneum, regular acanthosis, moderate focal spongiosis, focal suprapapillary thinning, dilated dermal vasculare and moderately dense chronic inflammation in superficial dermis (H and E, ×100) |
 |
| Figure 4a: Case of palmar psoriasis showing confluent parakeratosis, fibrin globules in stratum corneum, mild spongiosis, and moderate chronic infiltrate in dermal papilla (H and E, ×100) |
 |
| Figure 4b: Case of plantar psoriasis showing compact hyperkeratosis with confluent parakeratosis, hypogranulosis, moderate spongiosis, many dilated and ecstatic vessels in upper dermis (H and E, ×100) |

Fibrin globules in the stratum corneum were seen in 12 patients (38.7%) in the psoriasis group [Figure 4a], [Figure 5a] and [Figure 5b] and 8 patients (33.3%) in dermatitis group [Figure 3a]. The difference was not statistically significant (P = 0.78). Neutrophils in the stratum corneum in the absence of fibrin globules were present in 2 psoriasis biopsies but none in dermatitis biopsies (P = 0.5).
 |
| Figure 5a: A case of palmoplantar psoriasis showing massive compact hyperkeratosis, focal parakeratosis, irregular acanthosis with narrow tapered rete ridges, suprapapillary thinning, dilated tortuous dermal vasculature, moderate chronic inflammation in dermal papilla (H and E, ×40) |
 |
| Figure 5b: Palmoplantar psoriasis with many fibrin globules in stratum corneum and moderate spongiosis (H and E, ×100) |
In palmo-plantar psoriasis, granular layer was normal in 24 biopsies (77.42%), with hypogranulosis seen in 7 biopsies (22.6%) [Figure - 4]b. In dermatitis, granular layer was normal in 23 patients (95.8%) while hypogranulosis was seen in one biopsy (4.2%). Although hypogranulosis was noted in greater number of psoriasis than dermatitis biopsies, it did not reach statistical significance (P = 0.12).
Regular acanthosis was observed in 8 (27.6%) and 2 (9.1%) patients of psoriasis [Figure - 3]b and dermatitis respectively while it was irregular in 21 psoriasis (72.4%) and 20 dermatitis cases (90.9%). The acanthosis pattern in 2 patients each in both groups could not be commented on as these were oblique sections. This finding was not statistically significant (P = 0.16).
Neutrophils in the stratum spinosum were seen in 3 biopsies (10%) in the psoriasis group and none in dermatitis group (P = 0.25).
In the psoriasis group, spongiosis was absent in 12 cases (38.7%), mild in 11 patients (35.5%), moderate in 5 (16.1%) and severe, with formation of spongiotic vesicles, in 3 cases (9.7%) while in the dermatitis group, it was absent in 7 cases (29.2%), mild in 7 (29.2%), moderate in 5 (20.8%) and severe with formation of spongiotic vesicles in 5 cases (20.8%). Spongiosis was thus present in 19 cases (61.3%) in the psoriasis group [Figure - 4]b, [Figure - 5]b and [Figure - 6] and 17 cases (70.8%) in dermatitis group. Although greater number of dermatitis lesions showed spongiosis including presence of spongiotic vesicles [Figure - 6], it was not statistically significant.
 |
| Figure 6: A case of palmoplantar dermatitis showing compact hyperkeratosis, irregular acanthosis, moderate to severe focal spongiosis with spongiotic vesicle formation and normal dermis (H and E, ×40) |
Suprapapillary thinning could not be commented upon in 2 biopsies in each group due to oblique sections This feature was seen in 15 cases (51.7%) in psoriasis group [Figure 5a] and only 5 cases (22.73%). in the dermatitis group [Figure 3a] (P = 0.04).
There was no statistically significant difference in the rete ridge pattern between the two groups. Dermo-epidermal junction was normal in all the biopsies in both groups.
Dermal vasculature was normal in 19 psoriasis biopsies (61.3%) and 12 dermatitis biopsies (50%). Vessels were dilated and ectatic in 38.7% and 50% of the biopsies in the two groups respectively [Figure 4b] (P = 0.402).
An inflammatory infiltrate was present in 26 psoriasis biopsies (84%) and 24 dermatitis biopsies (75%) (P = 0.505). There was no significant difference in the type of inflammatory infiltrate.
In the two groups, although majority of the biopsies showed an inflammatory infiltrate in both dermal papilla and papillary dermis [Figure 5a] (P = 0.45), inflammatory infiltrate in the papillary dermis alone was observed in significantly greater proportion of dermatitis cases (P = 0.021).
Dermal edema was not a conspicuous finding in both psoriasis and dermatitis biopsies, although 19% of psoriasis lesions showed some edema compared to none in the dermatitis group (P = 0.03).
Discussion
The difficulty in differentiating psoriasis from dermatitis at palmo-plantar sites is well known, given the similarity of clinico-histopathologic features of the two diseases. In our study, a total of 55 palmo-plantar skin biopsies were studied which included 31 of clinically confirmed palmo-plantar psoriasis (Group 1) and 24 of hyperkeratotic palmo-plantar dermatitis. (Group 2). Since the two conditions show considerable clinical overlap, only cases with associated classic lesions of the primary disease elsewhere were included to make the diagnosis and inclusion criteria very robust. Only hematoxylin and eosin (H and E) stained sections were evaluated. Staining of slides with special stains such as periodic acid Schiff (PAS) stain or gomori methenamine silver (GMS) was not undertaken because cases with suspicion/evidence of other papulo-squamous conditions by clinical examination and bed-side investigations (KOH examination for fungus to rule ot tinea mannum/pedis etc.) were excluded.
In this retrospective study, significantly greater number of psoriatic lesions had features of parakeratosis including confluent parakeratosis, suprapapillary thinning and dermal edema. Features such as hypogranulosis, regular acanthosis and presence of neutrophils in the stratum corneum and spinosum were more often seen in psoriasis, but did not reach statistical significance. Both psoriasis and dermatitis biopsies showed spongiosis (61% vs 71% respectively), although severe spongiosis with formation of spongiotic vesicles was more often seen in dermatitic lesions. Other histological features like focal parakeratosis, presence of fibrin globules within stratum corneum, irregular acanthosis, dilated and ectatic vessels, type and location of the inflammatory infiltrate were comparable between the two groups.
Previous studies have shown that features helpful in differentiating dermatitis from psoriasis are the presence of mostly intact granular layer, spongiosis, sometimes evolving to vesiculation, irregular epidermal hyperplasia and presence of eosinophils in dermatitis, while neutrophils in the stratum corneum, hypogranulosis, regular acanthosis and suprapapillary thinning favour psoriasis [Table - 2].[11]
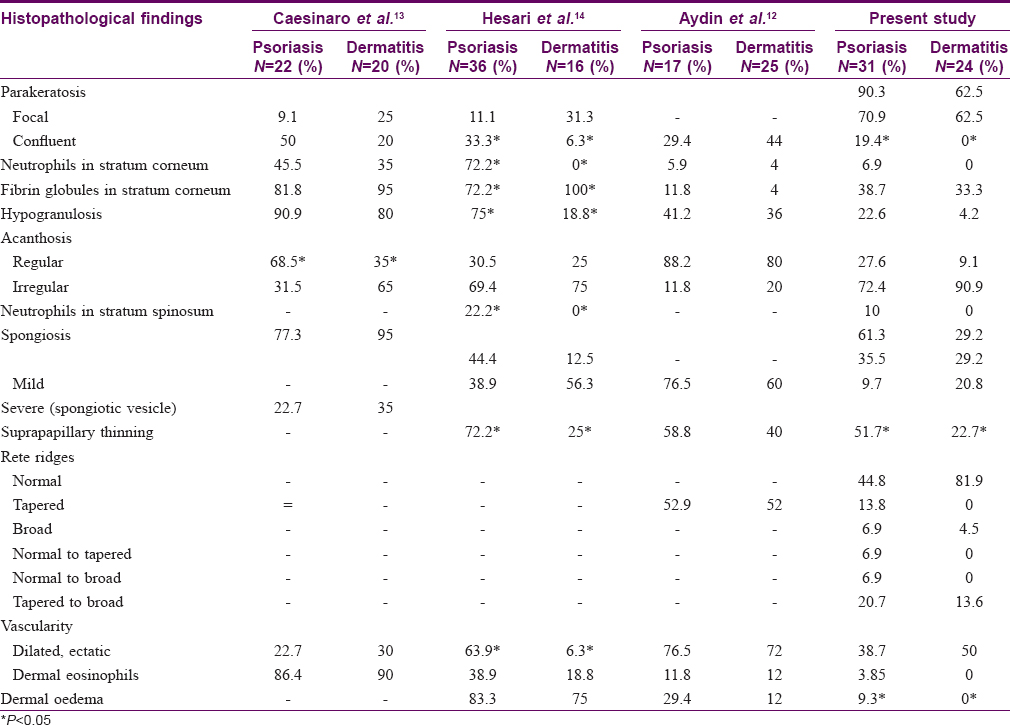
Aydin et al.[12], on comparing histological parameters of palmo-plantar psoriasis and dermatitis, found parakeratosis at multiple foci, more commonly in palmo-plantar psoriasis (70.6%), than palmo-plantar dermatitis (44%). They observed confluent parakeratosis in 29.4% of psoriasis and 44% of dermatitis biopsies. The only significant parameter in their study was vertical alternation of parakeratosis and orthokeratosis in psoriasis. In the study by Cesinaro et al.,[13] marked parakeratosis, i.e., occurrence of multiple parakeratotic foci vertically alternating with hyper-orthokeratosis, was seen with increased frequency in psoriasis as compared to allergic contact dermatitis of palms and soles, though it did not reach statistical significance. In the study by Hesari et al.,[14] confluent parakeratosis was significantly higher in palmo-plantar psoriasis than eczema (P = 0.044). In our study, majority of the biopsies of both conditions showed focal parakeratosis, without any specific pattern being discerned [Table - 2]. Confluent parakeratosis was observed only in the psoriasis group (19%).
We found fibrin globules in the stratum corneum in about equal number of cases in both groups (39% vs 33% in psoriasis and dermatitis respectively). In fact, a wet stratum corneum was seen in a slightly greater proportion of psoriasis cases than dermatitis. Hesari et al.[14] documented plasma mounds in all their palmo-plantar eczema cases and 72.2% of psoriasis cases.
A decrease or absence of granular layer in the suprapapillary area is an important finding in psoriasis. However in our study, hypogranulosis, although observed more often in psoriasis than dermatitis (22.6% vs 4%), did not reach statistical significance (P = 0.12).
In our study, irregular acanthosis was more common than regular acanthosis in both conditions although regular acanthosis was found more often, in psoriasis (28% vs 9%). In the study by Cesinaro et al., regular acanthosis was significantly more common in palmo-plantar psoriasis than eczema P = 0.03.[13] Aydin et al., also demonstrated regular acanthosis more commonly in psoriasis of the palms and soles than eczema though it was not statistically significant.[12] The study by Hesari et al. showed results similar to ours where irregular acanthosis was the predominant feature in both psoriasis (69.4%) and eczema. (75%).[14]
Our study did not support the previous view of presence of neutrophils in the stratum corneum as a consistent finding in psoriasis. In fact neutrophils were present in the stratum corneum in only 2 psoriasis biopsies and in stratum spinosum in 10% of psoriasis cases. This feature was absent in dermatitis. Spongiosis, mostly in the lower half of the epidermis, has been observed to be a prominent finding in palmo-plantar psoriasis and may be so prominent that it can resemble dermatitis.[7] In our study, spongiosis was detected in 61% of palmo-plantar psoriasis and to a slightly greater extent (71%) in palmo-plantar dermatitis, although severe spongiosis with formation of spongiotic vesicles was seen in just 9.7% of psoriasis as against 20.8% of dermatitis biopsies. These findings are in accordance with previous studies which have stated that spongiosis is not a useful feature to differentiate between these two conditions occurring on palmo-plantar aspects.[8]
Suprapapillary thinning, mainly focal, was present in a significantly greater proportion of psoriasis biopsies. This is in agreement with the Hesari et al. study who found suprapapillary thinning to be a strong pointer towards the diagnosis of psoriasis.[14]
Abnormal vascularity (dilated, ectatic vessels) was seen in 38.7% of our palmo-plantar psoriasis and 50% of dermatitis biopsies, suggesting that this important histological manifestation of psoriasis may not be useful in the diagnosis of psoriasis of the palms and soles. This was concordant with the observations of Cesinaro and Aydin et al., although Hesari et al. demonstrated dilated vessels in 64% of palmo-plantar psoriasis as against just 6.3% of dermatitis, and considered this finding to be a strong pointer towards psoriasis.[12],[13],[14] The nature of dermal inflammation was similar in the two groups. The infiltrate was predominantly lymphocytic, but neutrophils in association with chronic inflammation were seen in 11.5% of psoriasis cases. Eosinophils interspersed with chronic inflammation were seen in an occasional case in both conditions. A feature noted in this study was exclusive presence of inflammatory infiltrate in the papillary dermis without associated involvement of the dermal papilla in significantly greater proportion of palmo-plantar dermatitis than psoriasis (P = 0.021)
Dermal oedema was seen in 19% of psoriasis and none of the dermatitis biopsies (P = 0.03). Aydin and Hesari et al. also observed dermal oedema more commonly in their palmo-plantar psoriasis cases than eczema, but the results were not statistically significant.[12],[14]
In conclusion, differentiation between palmo-plantar psoriasis and dermatitis may be difficult in view of significant clinico-histopathological overlap, necessitating a close follow-up of these cases. In our study, features such as confluent parakeratosis, suprapapillary thinning and dermal oedema were observed in a significantly greater number of psoriasis biopsies, while presence of an inflammatory infiltrate confined to the papillary dermis only without associated involvement of the dermal papilla was the only finding that reached statistical significance in dermatitis.
In view of the tremendous difficulty in differentiating these two conditions both clinically and histologically, recently, the two-gene test has been proposed, which can precisely discriminate between the two entities by identifying two best classifier genes, NOS2 and CCL27.[15] In a cohort of eczema (n = 28) and psoriasis patients (n = 25), these genes diagnosed all patients correctly and also identified initially misdiagnosed or clinically undifferentiated patients.
Conclusion
There is tremendous difficulty in differentiating between palmoplantar psoriasis and dermatitis histologically due to several overlapping histopathological features.
Acknowledgement
We thank Dr. Manoj K Singh and Dr. Sudheer Arava, Department of Pathology, AIIMS, New Delhi, for allowing us access to the glass slides of the study patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Krueger GG, Duvic M. Epidemiology of psoriasis: Clinical issues. J Invest Dermatol 1994; 102:14-8.
[Google Scholar]
|
| 2. |
Pettey AA, Balkrishnan R, Rapp SR, Fleischer AB, Feldman SR. Patients with palmoplantar psoriasis have more physical disability and discomfort than patients with other forms of psoriasis: Implications for clinical practice. J Am Acad Dermatol 2003;49:271-5.
[Google Scholar]
|
| 3. |
Spuls PI, Hadi S, Rivera L, Lebwohl M. Retrospective analysis of the treatment of psoriasis of the palms and soles. J Dermatolog Treat 2003;14:21-5.
[Google Scholar]
|
| 4. |
Chu A. Unusual skin presentations of psoriasis. Practitioner 1998; 242:282-6.
[Google Scholar]
|
| 5. |
Adişen E, Tekin O, Gülekon A, Gürer MA. A retrospective analysis of treatment responses of palmoplantar psoriasis in 114 patients. J Eur Acad Dermatol Venereol 2009;23:814-9.
[Google Scholar]
|
| 6. |
Berth Jones J. Eczema, Lichenification, Prurigo and Erythroderma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Sussex: Wiley-Blackwell; 2010. p. 23.20.
[Google Scholar]
|
| 7. |
Cribier BJ. Psoriasis under the microscope. J Eur Acad Dermatol Venereol 2006; 20:3-99.
[Google Scholar]
|
| 8. |
Weedon D. Skin pathology. 3rd ed. Edinburgh.:Churchill Livingstone; 2010.
[Google Scholar]
|
| 9. |
Ackermann AB, Boer A, Gottlieb GJ, Bennin B. Histopathologic diagnosis of inflammatory skin diseases: An Algorithmic Method Based On Pattern Analysis. 3rd ed. Chatham: Ardor Scribendi; 2005.
[Google Scholar]
|
| 10. |
Murphy M, Kerr P, Grant-Kels JM. The histopathologic spectrum of psoriasis. Clin Dermatol 2007; 25:524-8.
[Google Scholar]
|
| 11. |
Ackerman AB, Troy JL, Rosen RB, Jerasutus S, White CR, Kıng FD. Differential diagnosis in dermatopathology II. Philadelphia: Lea & Febiger; 1982.
[Google Scholar]
|
| 12. |
Aydin O, Engin B, Oguz O, Ilvan S, Demirkesen C. Non-pustular palmo-plantar psoriasis: Is histo- logic differentiation from eczematous dermatitis possible? J Cutan Pathol 2008;35:169-73.
[Google Scholar]
|
| 13. |
Cesinaro AM, Nannini N, Migaldi M, Pepe P, Maiorana A. Psoriasis vs allergic contact dermatitis in palms and soles: A quantitative histologic and immunohisto- chemical study. APMIS 2009;117:629-34.
[Google Scholar]
|
| 14. |
Hesari KK, Naraghi ZS, Nikoo A, Ghanadan A, Sabaghi M. Palmoplantar Psoriasis versus Eczema: Major Histopathologic Clues for Diagnosis. Iranian J Pathol 2014;9:251-6.
[Google Scholar]
|
| 15. |
Quaranta M, Knapp B, Garzorz N, Mattii M, Pullabhatla V, Pennino D. et al. Intraindividual genome expression analysis reveals a specific molecular signature of psoriasis and eczema. Sci Transl Med 2014;6:244-54.
[Google Scholar]
|
Fulltext Views
18,556
PDF downloads
6,134





