Translate this page into:
Acquired dermal macular hyperpigmentation secondary to bangles – an unusual encounter
Corresponding author: Dr. M Sendhil Kumaran, Department of Dermatology Venereology and Leprology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. drsen_2000@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta H, Subburaj K, Dogra S, Bishnoi A, Vinay K, Chatterjee D, et al. Acquired dermal macular hyperpigmentation secondary to bangles – an unusual encounter. Indian J Dermatol Venereol Leprol. 2024;90:506-8. doi: 10.25259/IJDVL_908_2022
Dear Editor,
Acquired dermal macular hyperpigmentation (ADMH) is a chronic disorder characterised by asymptomatic hyperpigmentation of varying shades of brown-to-slate-grey without antecedent inflammatory lesions. ADMH includes disorders of hyperpigmentation, namely, lichen planus pigmentosus, Riehl’s melanosis (pigmented contact dermatitis) and ashy dermatosis (erythema dyschromicum perstans).1 Various allergens have been implicated in the etiopathogenesis of these conditions, with evidence of relevant patch tests in the literature.2 We report a series of unique cases with ADMH secondary to bangles or “chooras” worn as a tradition by newly married women in North India.
Ten women presented with complaints of asymptomatic hyperpigmentation of forearms. Mean age of patients was 26.7 ± 1.9 years (23–30 years). There was no history of previous inflammatory dermatosis or history of use of cosmetics, fragrances, or any other topical preparations over the affected area. However, all 10 patients had a similar history of use of traditional bangles, commonly worn by newlywed women in North India. The bangles were made of lac and dyed with red colour, and worn on both forearms. The onset of hyperpigmentation was after a mean duration of 7 months (range: 4–11 months) following the use of bangles. All patients were right-handed.
Clinical examination revealed well to ill-defined, blotchy, slate-grey patches localised strictly to forearms only, predominantly affecting the right forearm (dominant hand) [Figures 1a to 1e]. Dermoscopy showed multiple pigment dots and globules sparing the eccrine and sebaceous gland openings [Figure 2a]. Histopathology demonstrated focal basal layer vacuolisation, melanin incontinence and dermal melanophages with minimal upper dermal infiltrate [Figure 2b]. Patch testing performed with Indian standard series was negative in all patients. However, the individual components of the bangles like dye, plastic resin, adhesives, etc., could not be separately patch tested as the methodology for the same has not been formulated.
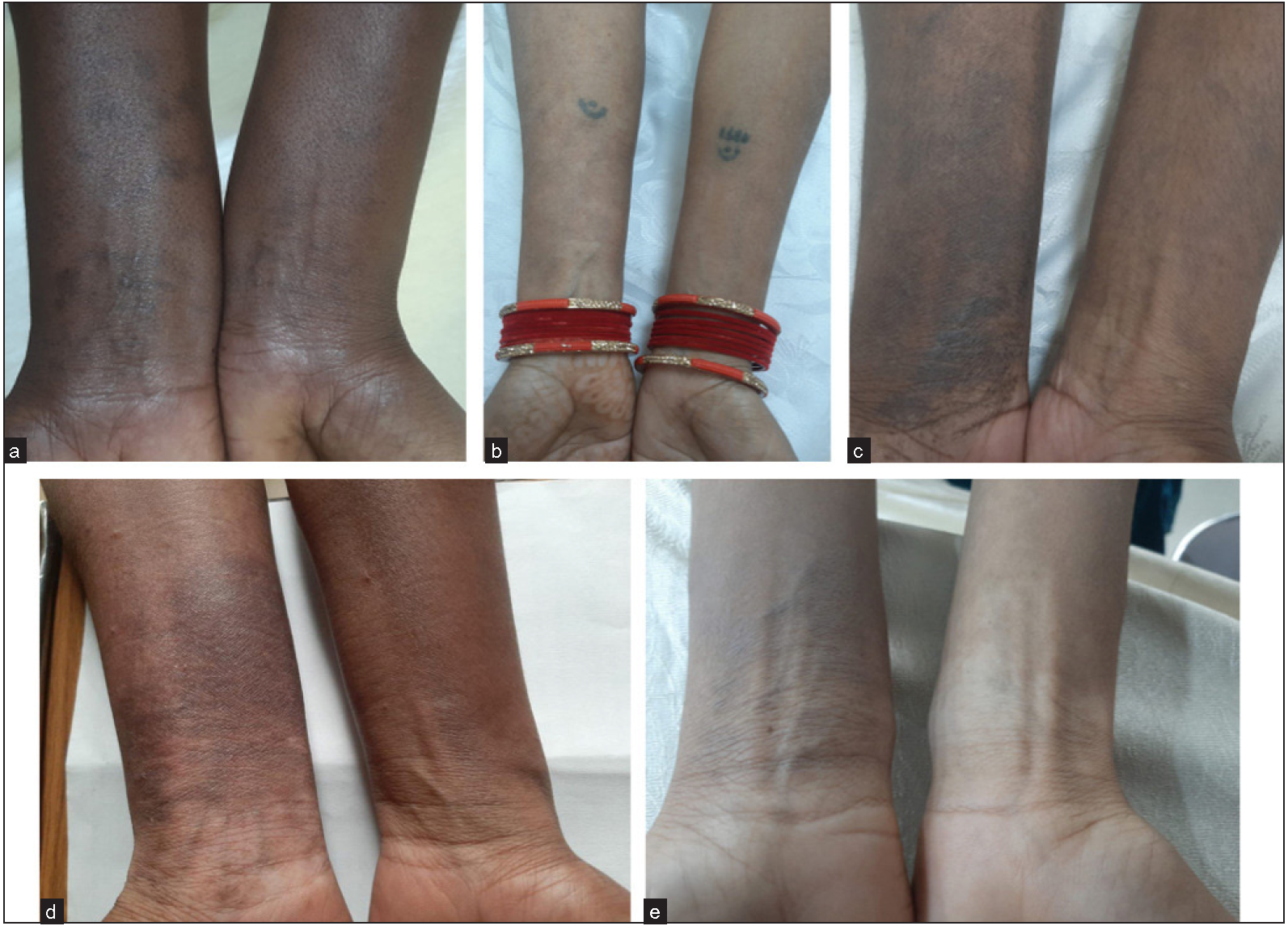
- Ill-defined slate-grey pigmentation over wrists and forearms in five patients. Predominance of lesions on right forearm is evident in all cases.
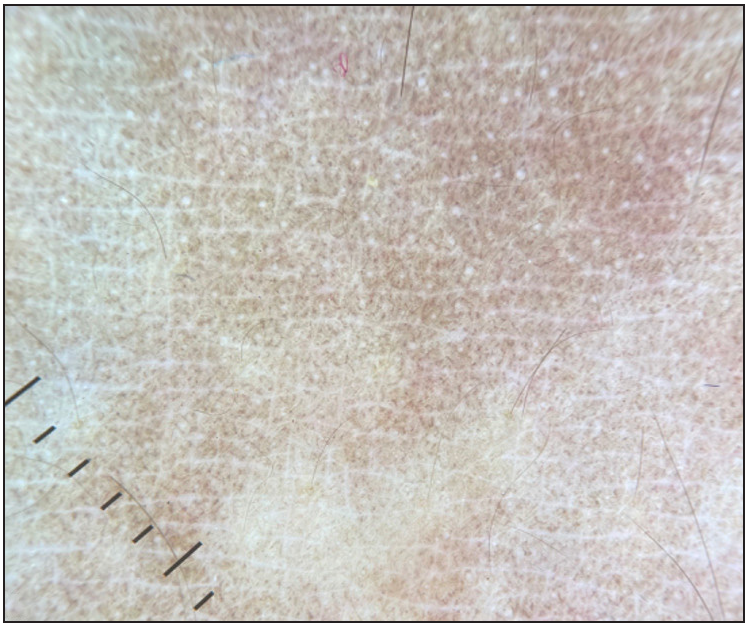
- Dermoscopy of lesion showing multiple pigment dots and globules sparing the eccrine and sebaceous gland openings (Dermlite DL4, 10×).
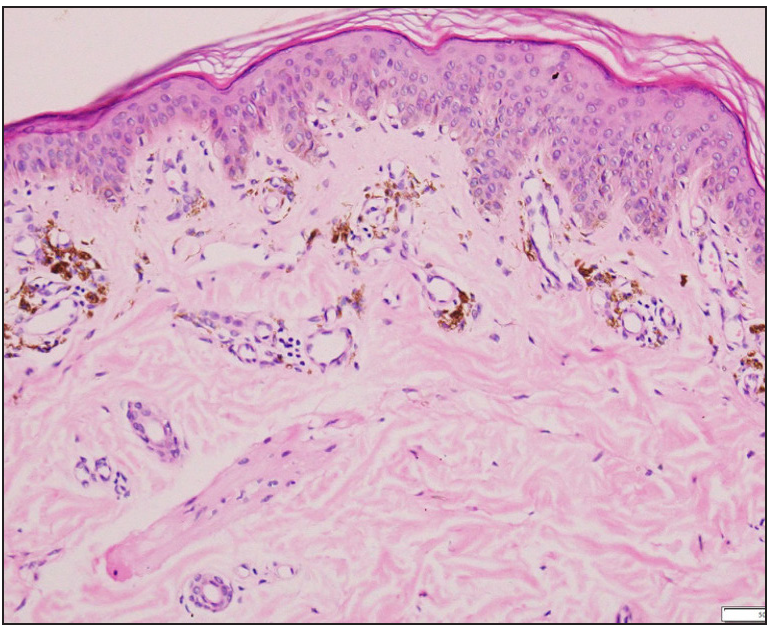
- Histopathological examination showing focal interface dermatitis with pigment incontinence and melanophages (Haematoxylin & Eosin, 400×)
A final diagnosis of ADMH was inferred in all patients based on clinical, dermoscopic and histopathological findings. The hyperpigmentation was hypothesised to be secondary to a hypersensitivity reaction to the bangle. Topical tacrolimus and sunscreen were prescribed along with avoidance of bangles. Eight out of ten patients had significant improvement in hyperpigmentation at follow-up visit after 6 weeks.
The cultural practices of a population can lead to various dermatoses specific to that region; for example, kumkum dermatitis, drawstring dermatitis, henna dermatitis, prayer nodules, bindi leukoderma, mudichood etc., are described in the Indian population.3 We describe a novel dermatoses unique to North Indian women due to the practice of wearing wedding bangles or “chooras”. The brides wear it for an entire year and the bangles are re-painted if the colour fades.
The patho-mechanism of ADMH has been proposed to be due to continuous or interrupted chronic exposure to allergens present in cosmetics, textiles, fragrances or hair dyes leading to a type IV hypersensitivity reaction resulting in interface dermatitis.2 Allergic contact dermatitis to bangles is well-known; however, dermal hyperpigmentation as in these cases likely resulted from a chronic subclinical injury due to an unknown component of the bangles. Mean duration of exposure to bangles prior to onset of pigmentation was 7 months in our series. The latency between exposure to development of pigmentation without any overt eczema points in favour of a diagnosis of ADMH. The right sided predominance of lesions can be explained by the use of the dominant hand for household chores, leading to repeated trauma and leaching of allergens more on the right side compared to the left. Koebnerization resulting in lichen planus pigmentosus-like presentation has been reported in literature.4 The patch test with standard series was negative. Traditionally made with ivory, chooras are now made of “lac” and plated with red paint. “Lac” or “shellac” is a resinous compound prepared from lac insects and is well-known to cause contact allergy to lipsticks and mascaras. Other possible allergenic components of bangles include cobalt, nickel, colophony and red dyes. The extrinsic nature of the inciting agent is also evident by the sparing of creases [Figure 1] which are relatively protected from the exposure to both the allergens and the sun. Sweating in hot and humid weather leads to leaching of the allergens from the bangles resulting in a low grade contact sensitisation.
Extra facial melasma could be considered as a differential in these cases. While extra facial melasma also commonly occurs over forearms, it often involves the outer aspect of forearms and is characterised by well-defined brownish pigmentation with coexistent or preceding facial melasma, unlike the ill-defined, blotchy, slate-grey pigmentation observed over ventral aspect of forearms in our series.5
ADMH can be secondary to chronic exposure to a specific allergen and the temporal correlation between exposure and hyperpigmentation is essential to establish the causality. In our study we found a unique cultural practice resulting in ADMH in a series of patients. The cessation of exposure is crucial in the management of ADMH.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Acquired dermal macular hyperpigmentation: An update. Indian Dermatol Online J. 2021;12:663-73.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Contact sensitization to hair colours in acquired dermal macular hyperpigmentation: results from a patch and photo-patch test study of 108 patients. J Eur Acad Dermatol Venereol. 2019;33:1349-57.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoses due to Indian cultural practices. Indian J Dermatol. 2015;60:3-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Koebnerization and lichen planus pigmentosus: Is it a reality? Pigment International. 2019;6:115-6.
- [Google Scholar]
- Extrafacial melasma: A scenario less explored. Indian Dermatol Online J.. 2022;13:484-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





