Translate this page into:
Acrodermatitis enteropathica in an infant with normal zinc levels
2 Department of Dermatology, Father Muller Medical College, Mangalore, Karnataka, India
Correspondence Address:
M Ramesh Bhat
Department of Dermatology, Father Muller Medical College, Mangalore - 575 002, Karnataka
India
| How to cite this article: Pinto M, Bhat M R, Dandekeri S, Kambil SM. Acrodermatitis enteropathica in an infant with normal zinc levels. Indian J Dermatol Venereol Leprol 2015;81:70-71 |
Sir,
Acrodermatitis enteropathica is a rare, autosomal recessive disorder classically characterized by zinc deficiency due to defective absorption. It is associated with ocular, gastrointestinal, and mucocutaneous symptoms with variable frequency, and can be fatal without zinc therapy. [1] We report a case of acrodermatitis enteropathica in a full-term, breastfed infant with normal zinc levels, who showed marked improvement on initiation of zinc therapy.
An exclusively breastfed 4-month-old male infant presented with multiple well-defined erythematous, oozy, crusted plaques around the mouth and eyes, the perineal and perianal regions, scalp, and extremities [[Figure - 1]a-c]. The baby, born by full term normal delivery to non-consanguineous parents, had developed these lesions a month earlier. He had normal anthropometric measurements, but was irritable and febrile. There was no history of diarrhea or photophobia in the infant or of similar complaints among the parents. Based on the characteristic distribution of the rash, we arrived at a working diagnosis of acrodermatitis enteropathica.
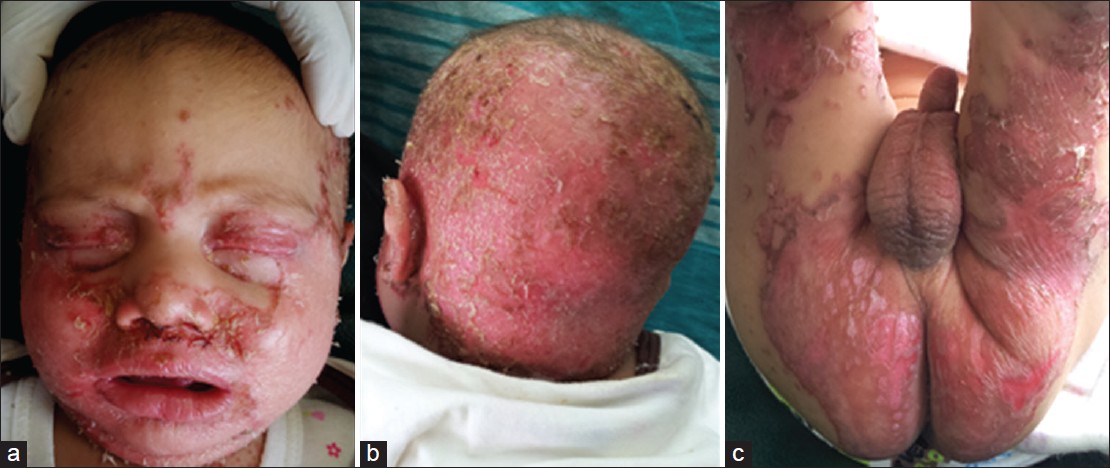 |
| Figure 1: Multiple erythematous oozy, crusted plaques distributed periorificially: (a) face; (b) posterior scalp; (c) perineal and perianal regions |
Hemogram, liver and renal function tests were normal. Serum zinc estimation was performed at the Metropolis Laboratory, Bangalore using inductively coupled plasma mass spectrometry and was found to be 107 μg/dl (normal: 70-110 μg/dl). Serum alkaline phosphatase level was low (45 U/l; normal: 115-360 IU/l). The mother′s serum zinc level was also found to be within normal limits. While testing for zinc levels, collection of fasting blood samples in trace element-free collection tubes, preventing hemolysis of samples, usage of disposable polyethylene gloves free of talc or other coatings while handling the samples, and processing of samples in a clean, dust- and smoke-free laboratory were the important measures taken to avoid zinc contamination. Biopsy of the skin lesions revealed parakeratosis with neutrophilic microabscesses in the stratum corneum [[Figure - 2]a]. The remainder of the epidermis and dermis were unremarkable [[Figure - 2]b].
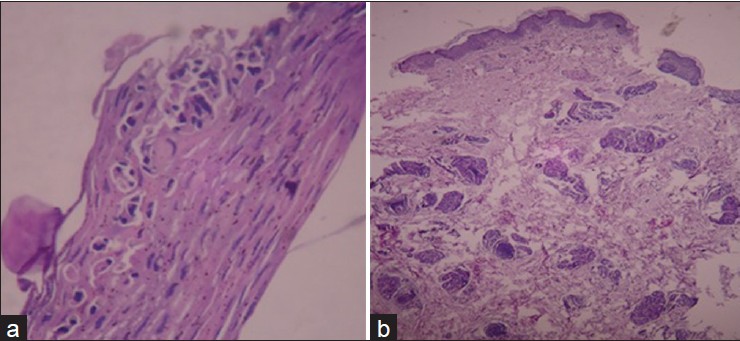 |
| Figure 2: (a) Parakeratosis with neutrophilic microabscess in the stratum corneum (H and E, ×40) and (b) unremarkable dermis |
The patient was started on 5 mg/kg of oral zinc therapy, parenteral antibiotics based on pus culture and sensitivity report, and supportive measures. Within 48 h of initiation of treatment, there was subsidence of erythema and scaling of the skin lesions, with complete clearance of lesions after 10 days of treatment [[Figure - 3]a and b]. Serum zinc level was re-measured after starting zinc supplementation and the zinc level was found to be elevated (190 μg/dl). At discharge, lifelong continuation of oral zinc supplementation was advised.
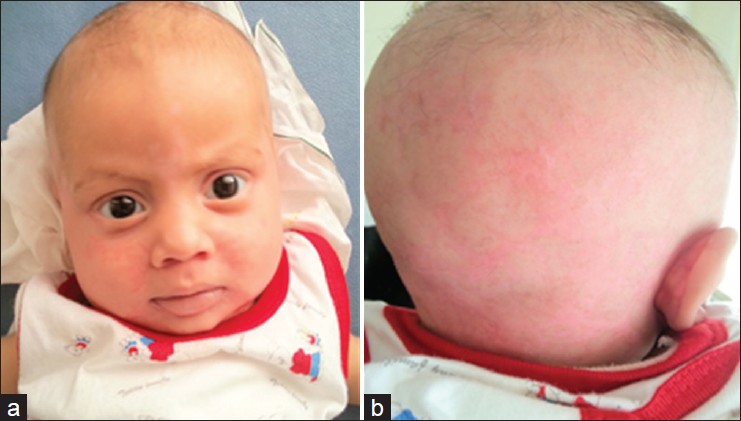 |
| Figure 3: Resolution of skin lesions in 1 week duration: (a) face and (b) posterior scalp |
Acrodermatitis enteropathica is usually reported in premature babies due to insufficient body stores of zinc as well as high zinc requirements, and at the time of weaning. However, it is rare in breastfed infants, as seen in our patient. The presence of a zinc-binding ligand in breast milk generally protects breastfed infants against this condition by increasing zinc bioavailability. It is clinically characterized by periorificial and acral dermatitis, diarrhea, and alopecia, with the complete triad being reported in only 20% of patients. [2] Our patient did not present with diarrhea.
The clinical diagnosis is confirmed by serum zinc levels <50 μg/dl. A low plasma zinc level is not indispensable for the diagnosis; in rare variants, although plasma zinc concentration is normal, defective release of zinc to different tissues produces a similar clinical picture. [3] Low levels of serum alkaline phosphatase, as seen in our case, can be a valuable indicator of zinc deficiency even when plasma zinc levels are normal, as it is a zinc-dependent enzyme. [4] Histopathological examination of the skin is non-specific and not diagnostic. In case of patients presenting with acrodermatitis enteropathica-like skin lesions in the perioral and diaper area, not responding to oral zinc or antimicrobials, conditions like biotin deficiency, essential fatty acid deficiency, phenylketonuria, organic acidemias such as methylmalonic acidemia, propionic acidemia, maple syrup urine disease, and metabolic disorders of the urea cycle like glutaric aciduria type I, ornithine transcarbamylase deficiency, and citrullinemia should be considered.
Treatment with oral zinc in a dose of 3-5 mg/kg/day in children results in rapid improvement of diarrhea within 24 h and subsidence of skin lesions within 1-2 weeks. Lifelong zinc supplementation and a diet rich in zinc, in the form of unmilled cereals, beans, cheese, whole wheat bread, and animal proteins like lean red meat are necessary to prevent recurrences. [5] This case emphasizes the fact that when a patient presents with the characteristic periorificial and acral rash, even in the absence of decreased zinc levels, acrodermatitis enteropathica should be suspected and treated appropriately.
| 1. |
Moynahan EJ, Barnes PM. Zinc deficiency and a synthetic diet for lactose intolerance. Lancet 1973;1:676-7.
[Google Scholar]
|
| 2. |
Maverakis E, Fung MA, Lynch PJ, Draznin M, Michael DJ, Ruben B, et al. Acrodermatitis enteropathica and an overview of zinc metabolism. J Am Acad Dermatol 2007;56:116-24.
[Google Scholar]
|
| 3. |
Lee SY, Jung YJ, Oh TH, Choi EH. A case of acrodermatitis enteropathica localized on the hands and feet with a normal serum zinc level. Ann Dermatol 2011;23:S88-90.
[Google Scholar]
|
| 4. |
Lee MG, Hong KT, Kim JJ.Transient symptomatic zinc deficiency in a full term breast fed infant. J Am Acad Dermatol 1990;23:375-9.
[Google Scholar]
|
| 5. |
Sehgal VN, Jain S. Acrodermatitis enteropathica. Clin Dermatol 2000;18:745-8.
[Google Scholar]
|
Fulltext Views
8,293
PDF downloads
2,242





