An unusual case of co-localization of proliferating trichilemmal tumor and seborrheic keratosis
Corresponding author: Dr. Geeti Khullar, Department of Dermatology and Sexually Transmitted Diseases, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi - 110 029, India. geetikhullar@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Lakhani R, Khullar G, Sharma S. An unusual case of co-localization of proliferating trichilemmal tumor and seborrheic keratosis. Indian J Dermatol Venereol Leprol 2021;87:551-4.
Sir,
The incidence of benign and malignant lesions associated with seborrheic keratosis is about 9% and is proportionately linked with sun exposure.1 Trichilemmal keratinization is the abrupt transition of nucleated epithelium of outer root sheath of the hair follicle to anucleated keratin without the formation of granular layer. Trichilemmal tumors arising in seborrheic keratosis are rare.2-4 We report a case of proliferating trichilemmal tumor that developed in a longstanding seborrheic keratosis on the abdomen.
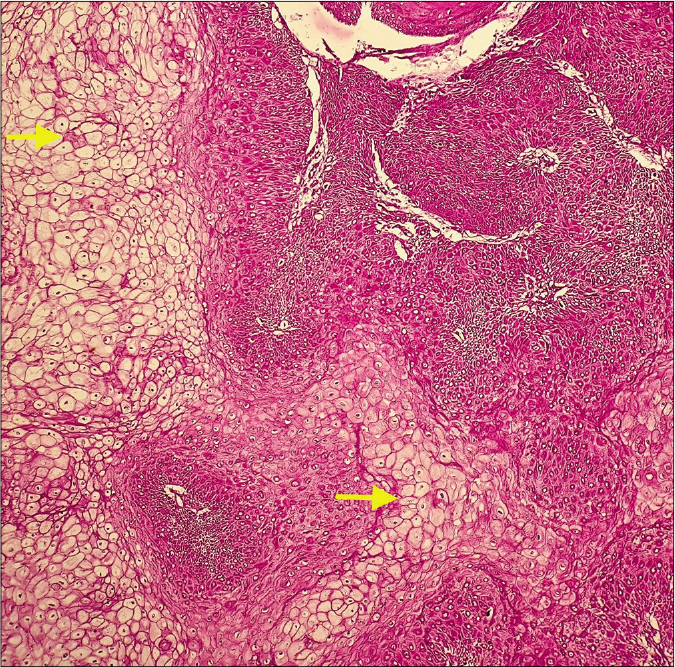
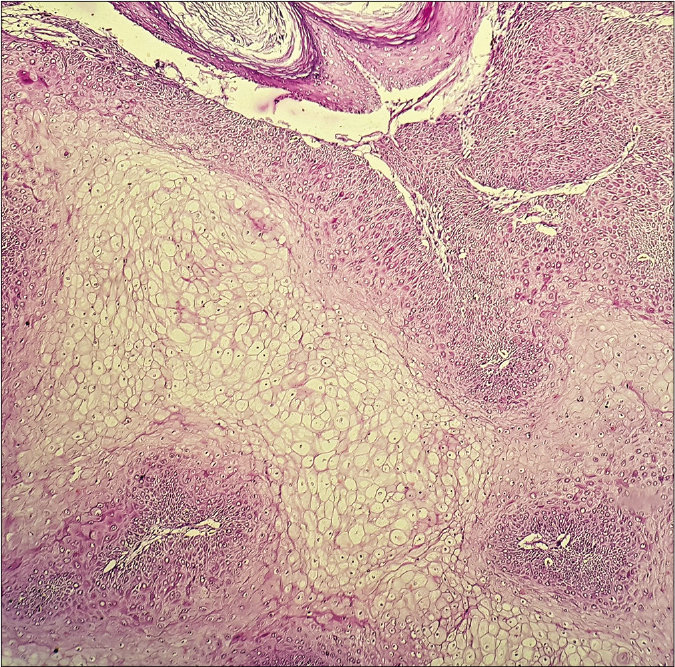
A 52-year-old woman presented with a progressively enlarging conical growth of five months duration arising from a raised black lesion on her lower abdomen that had been present for 20 years. Physical examination revealed a well-demarcated black colored verrucous plaque, measuring 5.7 cm × 3.5 cm in size, with a stuck-on appearance on the left iliac region . Arising from the edge of the plaque, was a hyperkeratotic scaly cutaneous horn-like growth of size 1.5 x 0.5 cm with an erythematous base [Figure 1]. There was no lymphadenopathy. Wide excision with 1 cm margin was performed, with the differential diagnosis of seborrheic keratosis for the black plaque and cutaneous horn versus keratoacanthoma for the overlying growth. Histopathological examination revealed two distinct components . One showed hyperkeratosis, papillomatosis, acanthotic proliferation of basaloid cells with pseudo-horn cysts and abundant melanin pigment, suggestive of acanthotic seborrheic keratosis [Figures 2a and b] and the other component had well-defined proliferating lobules of pale to clear squamous epithelium with amorphous debris and abrupt keratinization lacking granular layer, a histology resembling outer root sheath of the hair follicle, signifying trichilemmal keratinization [Figures 2c and d]. There was no cellular atypia, mitosis or necrosis within the tumor. The lowermost part of the epithelial lobules in the underlying dermis was surrounded by inflammatory infiltrates. Morphologically, there was an obvious distinction between the two tumor components. Clear cells seen in the deeper layers showed presence of glycogen on periodic acid-Schiff staining [Figure 2e] with sensitivity for diastase [Figure 2f]. Hence, a final diagnosis of proliferating trichilemmal tumor arising in seborrheic keratosis was made. After two years of follow-up, there was no evidence of recurrence.

- Hyperkeratotic scaly cutaneous horn-like growth arising from a verrucous black colored plaque on the left iliac region
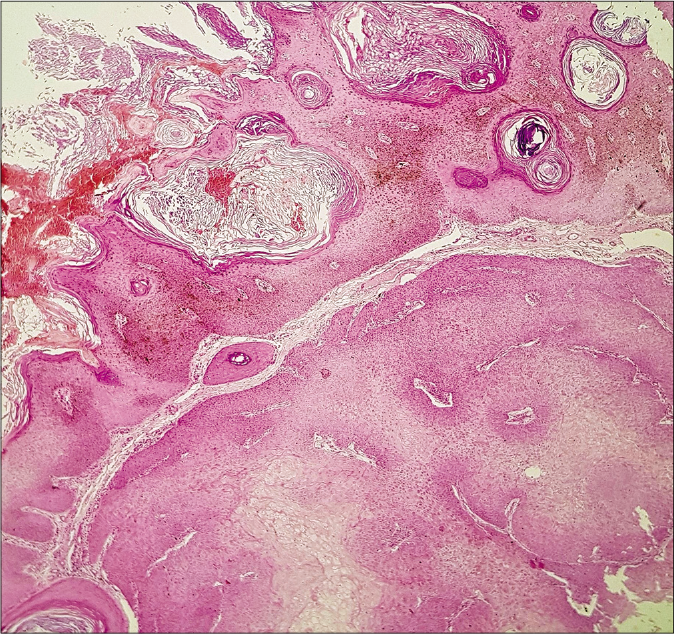
- Tumor with hyperkeratosis, dark basaloid cells and dense melanin in the upper part and squamoid pale clear cells in the lower part (hematoxylin and eosin, ×40)
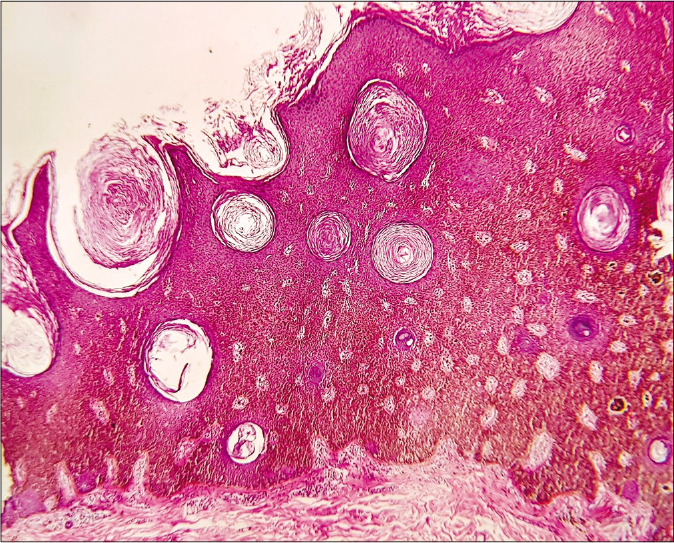
- Verrucous black plaque showing acanthotic epidermis with basaloid cells, abundant melanin and numerous pseudo-horn cysts, suggestive of acanthotic seborrheic keratosis (hematoxylin and eosin, ×100)
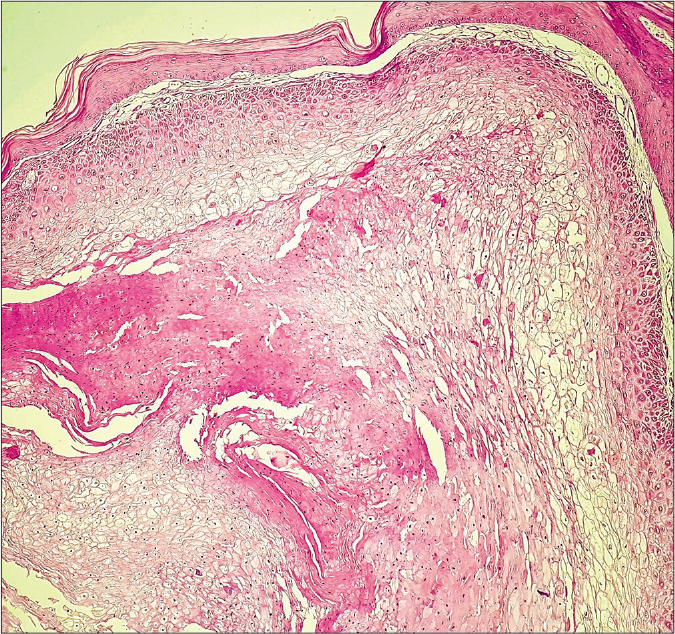
- Cutaneous horn-like growth revealing invaginating epithelial lobules of proliferating pale keratinocytes showing trichilemmal keratinization and lacking granular layer. (hematoxylin and eosin, ×100)
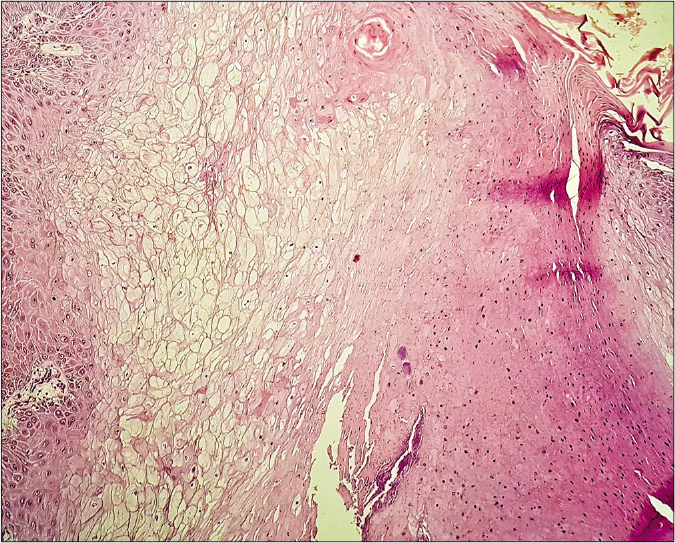
- Proliferating trichilemmal tumor showing clear keratinocytes in the centre and trichilemmal keratinization on the right (hematoxylin and eosin, ×100)
- Clear cells showing dark pink staining (arrows) depicting the presence of glycogen (periodic acid -Schiff, ×100)
- Loss of periodic acid -Schiff positivity in clear cells with diastase (×100)
Seborrheic keratosis is one of the most common benign epidermal tumors that may rarely be associated with secondary malignancies. Associated lesions arising within or adjacent to seborrheic keratosis include basal cell carcinoma as the most frequent , followed by squamous cell carcinoma, melanoma, melanocytic nevi, solar keratosis and Bowen’s disease.1 It is proposed that these tumors could occur either as a chance association with seborrheic keratosis or seborrheic keratosis may be a precursor lesion for them.1 Proliferating trichilemmal tumor is an uncommon benign adnexal tumor that arises from the outer root sheath of the hair follicle. It presents as a slowly enlarging exophytic mass of size ranging from 1-25 cm, that may ulcerate, bleed or discharge purulent material.5 The commonest site is scalp in 90% of the cases, though rarely it may occur on the face, neck, trunk, extremities and genitalia. It usually develops from a trichilemmal cyst subsequent to trauma or inflammation and infrequently may arise de novo.5 The tumor is well-circumscribed, located in the dermis or subcutis with squamoid cytological features and trichilemmal keratinization. Features pointing to trichilemmal keratinization include presence of clear cells and absence of granular layer. It can be classified into three groups: benign, locally aggressive and malignant.6 Surgical excision is the mainstay of treatment. A local recurrence rate of 3.7% was seen in a meta-analysis of 185 cases.5
Trichilemmal tumor developing in seborrheic keratosis is a rare phenomenon. Nakayasu et al. reported trichilemmal differentiation in a nodule that appeared in the centre of seborrheic keratosis.2 Proliferating trichilemmal tumor along with features of Bowen’s disease has been described in seborrheic keratosis.3 Kitagawa et al. reported a case of trichilemmal tumor with malignant tendency that developed in seborrheic keratosis.4 All these previous cases were reported in Japanese population and developed in longstanding seborrheic keratosis.2-4
Histopathological differentials of proliferating trichilemmal tumor are squamous cell carcinoma and trichilemmoma. Proliferating trichilemmal tumor is differentiated from squamous cell carcinoma by trichilemmal keratinization, presence of clear cells, absence of marked atypia and lack of infiltration into surrounding structures.5 Trichilemmoma shows one or more tumor lobules oriented around a central hair follicle, with palisading columnar cells in the periphery and a thickened basement membrane.2 Rarely proliferating trichilemmal tumor can undergo malignant transformation, sequentially starting from the adenomatous stage of trichilemmal cyst to epitheliomatous stage of proliferating trichilemmal tumor into the carcinomatous stage.6 Malignant proliferating trichilemmal tumor shows invasion, nuclear atypia, necrosis and abnormal mitotic figures.6 The detailed histopathological differences between proliferating trichilemmal tumor, squamous cell carcinoma and trichilemmoma are delineated in Table 1.
| Histological feature | PTT | Squamous cell carcinoma | Trichilemmoma |
|---|---|---|---|
| Silhouette | Well-circumscribed tumor with non-infiltrative borders | Invasive, irregular and asymmetric borders | Well-circumscribed with regular and symmetric borders |
| Tumor morphology | Intradermal or subcutaneous lobules of squamous epithelium with solid or solid-cystic components. Absence of granular layer and abrupt transition to trichilemmal keratinization in the central areas | Arises from the surface epidermis and infiltrates as sheets and islands of squamous epithelium. Well-differentiated tumor shows prominent epidermal keratinization | Solid lobule or group of lobules extending from the epidermis and usually connected to the hair follicle. Keratinization is often minimal and trichilemmal. The overlying epidermis shows hyperkeratosis and parakeratosis |
| Clear cells | Present in large numbers | Clear cells may occur as scattered foci or occasionally form tumor bulk in clear cell variant | Small uniform cells with round or oval vesicular nuclei. Many tumor cells have clear cytoplasm and are PAS positive, diastase sensitive |
| Palisading cells | Small basaloid cells are noted palisading at periphery | Absent | Nuclear palisading of peripheral columnar cells is characteristic |
| Thickened basement membrane | May be present | Absent | Individual lobule surrounded by a thickened hyaline eosinophilic mantle, which is PAS positive and diastase resistant |
| Atypia | Absent or mild. Seen in malignant variant | Present | Absent |
| Mitotic figures | Uncommon Atypical mitoses in malignant PTT |
Present | Absent |
| Infiltration into surrounding structures | Absent | Highly invasive, lymphovascular and perineural invasion | Absent |
| Additional findings | Foreign body giant cell reaction to keratinous material and calcification | Dense chronic inflammatory infiltrate | Pigmentation, calcification and necrosis may occur Central sclerotic zone in desmoplastic variant |
PAS: Periodic acid- Schiff, PTT: Proliferating trichilemmal tumor
The present case demonstrates the rare co-localization of proliferating trichilemmal tumor and seborrheic keratosis in an Indian patient. It is enigmatic as to whether proliferating trichilemmal tumor can arise from long-standing seborrheic keratosis in the absence of sun-exposure as a possible trigger or it simply represents a coincidental phenomenon. Since most trichilemmal tumors occur on sun-exposed sites with cumulative solar irradiation as a major cause, our report raises a question about the triggers causing trichilemmal differentiation. In our case as the lesional site was sun-protected, there was no evidence of apparent actinic damage on histology, in the form of atrophic epidermis and degeneration of elastic fibers in the dermis. One may speculate that persistent exogenous stimulus like friction due to the traditional Indian saree tied over lower abdomen by the patient may play a role in carcinogenesis, particularly in a pre-existing seborrheic keratosis. However, the unidentified disease pathophysiology relevant to this rare co-localization needs further exploration.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Seborrhoeic keratoses with associated lesions: A retrospective analysis of 85 lesions. Australas J Dermatol. 2006;47:109-13.
- [CrossRef] [PubMed] [Google Scholar]
- Trichilemmal differentiation in seborrheic keratosis. J Cutan Pathol. 1981;8:256-62.
- [CrossRef] [PubMed] [Google Scholar]
- Trichilemmal neoplasm developing in seborrheic keratosis--report of two cases. J Dermatol. 1985;12:167-73.
- [CrossRef] [PubMed] [Google Scholar]
- Trichilemmal tumor arising in a seborrheic keratosis: Analysis of cell kinetics by BrdU staining. J Dermatol. 1991;18:334-9.
- [CrossRef] [PubMed] [Google Scholar]
- Proliferating trichilemmal tumors: A review of the literature. Dermatol Surg. 2007;33:1102-8.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant proliferating trichilemmal tumour presenting early in life: An uncommon feature. J Cutan Aesthet Surg. 2011;4:51-5.
- [CrossRef] [PubMed] [Google Scholar]





