Translate this page into:
Annular lichenoid dermatitis of youth in a 15-year-old boy: Topical tacrolimus as a treatment option
2 Department of Pathology, Okmeydani Training and Research Hospital, Istanbul, Turkey
Correspondence Address:
Pelin Kuteyla �lk�men
Department of Dermatology, Okmeydani Training and Research Hospital, Kaptanpasa Mah, Darülaceze Cad, No: 27, 34384 Okmeydani - Şişli, Istanbul
Turkey
| How to cite this article: �lk�men PK, Kocat�rk E, G�ng�r S, Erzurumluoglu N. Annular lichenoid dermatitis of youth in a 15-year-old boy: Topical tacrolimus as a treatment option. Indian J Dermatol Venereol Leprol 2016;82:467 |
Sir,
Annular lichenoid dermatitis of youth is a recently described clinicopathological entity.[1],[2],[3] The clinical presentation of this lichenoid dermatosis changes according to the duration of the lesions. Initially, sharply demarcated, 1–5 cm sized erythematous macules appear which then enlarge to form annular, reddish-brown, non-scaling patches with hypopigmented centres and slightly raised borders. In older lesions, the erythema fades and leaves behind a complete or incomplete hyperpigmented ring.[1],[3]
A 15-year-old boy presented with a 1-year history of annular skin lesions which had begun as small macules and then slowly enlarged. They had not responded to 0.1% mometasone furoate cream applied twice daily for a month. Dermatological examination revealed 4–5 cm sized reddish-brown, annular plaques with non-atrophic, clear centres and indurated borders on the left flank and right side of the abdomen [Figure - 1]. A punch biopsy from the border of a plaque on the abdomen showed elongated rete ridges and hydropic degeneration in the basal layer with apoptotic keratinocytes and perivascular lympho-plasmacytic infiltrates in the superficial dermis [Figure - 2]. In view of these histopathological and clinical findings, annular lichenoid dermatitis of youth was diagnosed.
 |
| Figure 1: Reddish-brown annular plaque on the left flank |
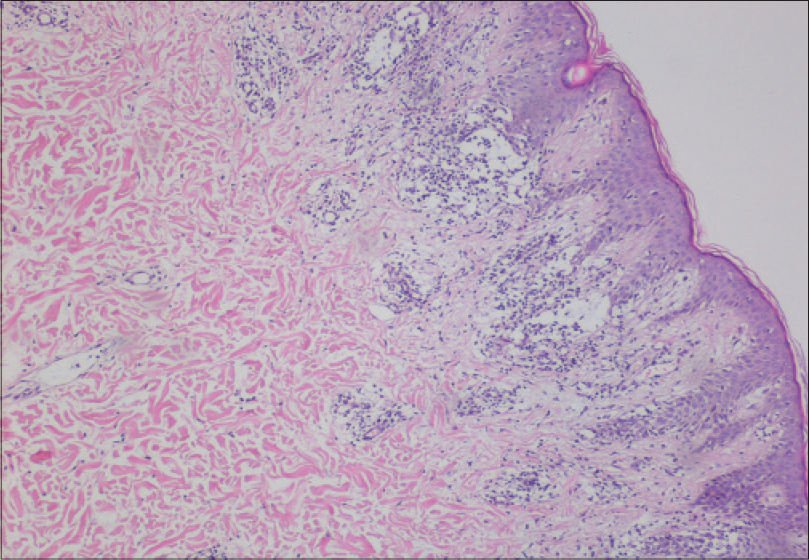 |
| Figure 2: Elongated rete ridges, exocytosis, spongiosis and hydropic degeneration in the basal layer, as well as apoptotic keratinocytes and perivascular lymphoplasmacytic infilltrates in the superficial dermis (H and E, ×400) |
Laboratory results were within normal limits including complete blood counts, routine biochemistry, urinalysis, antistreptolysin titer, rheumatoid factor, erythrocyte sedimentation rate and C-reactive protein. Indirect immunofluorescence for antinuclear antibody was weakly positive at 1:100 with a mottled pattern. An extensive infectious disease workup including serological testing for Epstein–Barr virus, cytomegalovirus, Borrelia, hepatitis B and C and stool examination for parasites and ova was negative. Patch testing with standard series antigens to exclude contact hypersensitivity was also negative. We could thus not identify any etiological or triggering factors in this case, underlining the idiopathic nature of annular lichenoid dermatitis of youth.[1]
Annular lichenoid dermatitis of youth was first described in 2003 in 23 patients.[1] Similar to the present case, the lesions were primarily located on the trunk and especially in the groin and flank regions; periumbilical, axillary and neck lesions have also been reported.[1],[3],[4] The mean age of onset has been reported to be approximately 11 years with no sex predilection noted.[1],[3],[4] There are usually no symptoms except for the appearance of new macules; our patient too denied any symptoms throughout the evolution of the lesions.[1],[3]
Triggering factors described in lichenoid dermatoses include persistent viral reactions, immunological changes, neoplastic diseases, contact with chemicals, ultraviolet exposure and drugs. However, no definite etiological factors or triggers have been reported in annular lichenoid dermatitis of youth barring one case that occurred following the third dose of hepatitis B vaccination.[1],[3] No association with Borrelia burgdorferi infection has been found[2] and patch testing with standard and textile series has also been reported negative in these patients.[1],[3]
The characteristic histology helps to differentiate annular lichenoid dermatitis of youth from other clinical diagnoses such as erythema migrans, morphea, vitiligo, patch-type granuloma annulare, interstitial granulomatous dermatitis, annular erythemas and mycosis fungoides.[1],[2],[4] Histological features also vary with the stage of the lesions in this condition. In the early macular lesions, band-like lymphocytic infiltrates occur in the papillary dermis and dermo-epidermal junction where vacuolar alteration is also seen. Then some of the lymphocytes move to the tips of the rete ridges leading to massive keratinocyte necrosis/ apoptosis. Epidermis shows quadrangular rete ridges, a basket-weave horny layer, and a normal thickness of granular layer. Intense keratinocyte damage leads to rete ridge loss in late lesions. Some lymphocytic infiltration and melanophages in the papillary dermis are also seen at the late stages. The infiltrate is primarily composed of CD4+ polyclonal T cells with some B cells and macrophages.[1]
The disease runs a chronic course. Treatment options include topical and/or systemic corticosteroids, photo(chemo)therapy, natural ultraviolet light exposure and topical tacrolimus. However, relapses are common with discontinuation of treatment.[1],[2],[4],[5] Keeping in mind the side effects of long-term potent steroid use, we preferred to treat our patient with topical tacrolimus 0.1%, twice daily. The lesions faded in 1 week and completely resolved following 3 months of this therapy. Cessation of the treatment resulted in a recurrence of the lesions but they again responded rapidly to topical tacrolimus (0.1%) twice daily [Figure - 3]a and [Figure - 3]b. Tacrolimus worked in this case probably due to its supressive effects on T lymphocytes. Although it appears to be effective, only one case without recurrence has been reported following treatment with tacrolimus (0.03%).[5]
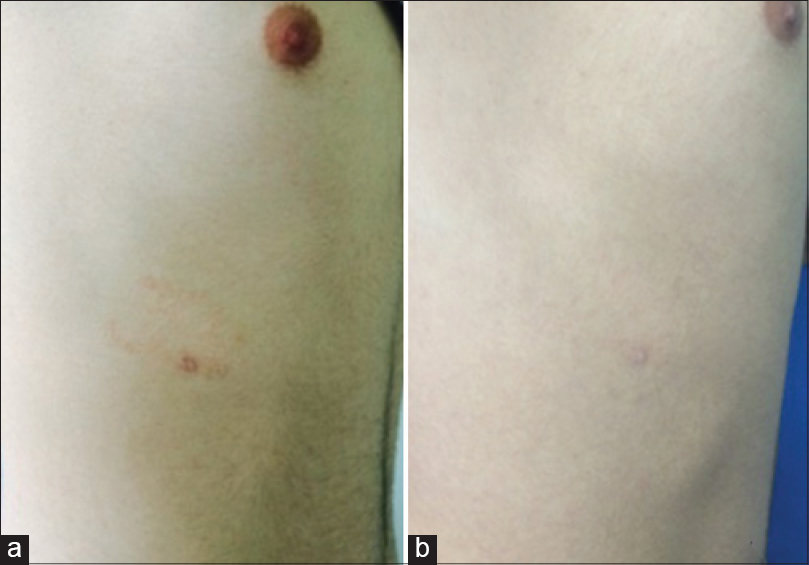 |
| Figure 3: Annular reddish-brown patch on the right side of the abdomen (a) before treatment, and (b) fading after treatment with topical tacrolimus |
Annular lichenoid dermatitis of youth must be considered in the differential diagnosis of annular plaques on the trunk of young patients and topical tacrolimus may be considered as a treatment option in this condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Annessi G, Paradisi M, Angelo C, Perez M, Puddu P, Girolomoni G. Annular lichenoid dermatitis of youth. J Am Acad Dermatol 2003;49:1029-36.
[Google Scholar]
|
| 2. |
Leger MC, Gonzalez ME, Meehan S, Schaffer JV. Annular lichenoid dermatitis of youth in an American boy. J Am Acad Dermatol 2013;68:e155-6.
[Google Scholar]
|
| 3. |
Sans V, Leaute-Labreze C, Vergier B, Taieb A. A further case of annular lichenoid dermatitis of youth: Role of the anti-hepatitis B immunization? Pediatr Dermatol 2008;25:577-9.
[Google Scholar]
|
| 4. |
Fabroni C, Salvini C, Piana S, Lo Scocco G. Annular lichenoid dermatitis. Clin Exp Dermatol 2010;35:921-3.
[Google Scholar]
|
| 5. |
Kleikamp S, Kutzner H, Frosch PJ. Annular lichenoid dermatitis of youth – A further case in a 12-year-old girl. J Dtsch Dermatol Ges 2008;6:653-6.
[Google Scholar]
|
Fulltext Views
4,740
PDF downloads
3,259





