Translate this page into:
Benign penile melanosis: A linear variant
2 Department of Pathology, Kannur Medical College, Kerala, India
Correspondence Address:
Vijayeeta Jairath
11-J/2 UH Medical Enclaves, Pandit Bhagwat Dayal Sharma, Post Graduate Institute of Medical Sciences, Rohtak - 124 001, Haryana
India
| How to cite this article: Jairath V, Jindal N, Sehrawat M, Jain V K, Kaur S, Priyadarshini M M. Benign penile melanosis: A linear variant. Indian J Dermatol Venereol Leprol 2015;81:655 |
Sir,
Penile melanosis is a rare benign hyperpigmentation of the glans and shaft of the penis usually affecting men of age between 15–72 years. Apart from melanin, other pigmentary deposits such as hemosiderin, lipofuscin, lipofuscin-like pigment and ferrous sulfate also contribute to the discoloration in penile melanosis.[1] Besides genetic and racial factors playing an important role in its pathogenesis, studies have reported it to be associated with previous injury, treatment with anthralin or psoralen and ultraviolet A (PUVA) therapy.[2]
Penile melanotic macules are a matter of concern to both the treating physician as well as the patient. Presence of large or enlarging macules with irregular edges and multifocal or variegated pigmentary patterns may arouse concern about atypical melanocytic proliferation and acral lentiginous melanoma.[3] It can be of cosmetic concern and embarrassment to the patient due to its unsightly appearance. Though a number of reports about penile melanosis are available,[2],[3] a linear variant of penile melanotic macule appears to be uncommon.
A 21-year-old man presented to the outpatient department of our hospital with complaints of an asymptomatic, grayish-black discoloration of glans penis since childhood. There was no history of genital infection, trauma or any previous treatments including PUVA therapy. No family or personal history of systemic disorder associated with hyperpigmentation was present. The reason for his visit to our department was his rejection from admission to the naval services due to this hyperpigmentation. The patient gave no history of increase in size or change in the colour of lesion. He was otherwise healthy and had no history of a previous skin problem. Examination revealed a line of uniform hyperpigmentation on the glans measuring about 1 × 0.2 cms with no surrounding inflammation or erythema [Figure - 1]. The rest of the physical and systemic examination was normal with no other abnormal pigmentation on his skin, mucosa or nails. Histologic examination of a 2.5-mm punch biopsy specimen revealed mild acanthosis, hyperpigmentation of basal keratinocytes and pigmentary incontinence with scattered melanophages in the dermis [Figure - 2].
 |
| Figure 1: Linear uniform hyperpigmentation on the glans measuring about 3 × 0.2 cm with no surrounding inflammation or erythema |
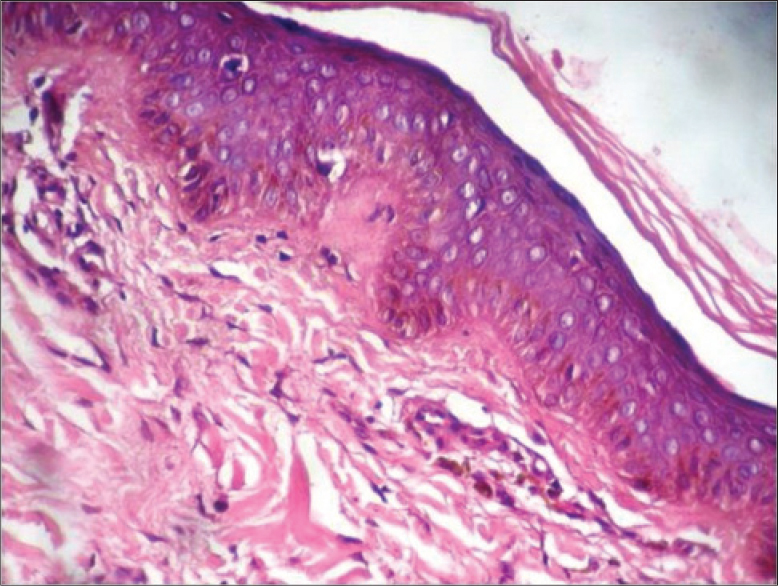 |
| Figure 2: Mild acanthosis, hyperpigmentation of basal keratinocytes, and pigmentary incontinence with scattered melanophages in the dermis (H and E, ×40) |
Absence of contiguous melanocytic proliferation and significant atypia differentiated it from melanoma. Furthermore, the immunohistochemical staining with human melanoma black 45 (HMB45) antibody was negative. The patient was assured about the benign nature of the lesion and was advised to report back in case of any significant change. The patient is on follow up for 2 years with no change in morphology of the existing lesion.
Genital melanotic macules are not uncommon. Most lesions go unnoticed by the patients due to the asymptomatic nature and its site. In a study of 10 000 men by Barnhill et al., the prevalence was reported to be 14.2%. This benign disorder has been labelled differently by various authors. Lenane et al., coined the term genital melanotic macule for penile melanosis. In 1982, Kopf and Bart described variegated macular hyperpigmentation on the glans and penile shaft in a 37-year-old white male as “penile lentigo”.[4] They emerge either as isolated lesions or as an important element of a syndrome with multisystem anomalies.[5] Because there was no history of any drug intake or any other systemic manifestations, disorders such as Peutz–Jegher syndrome, LAMB syndrome, LEOPARD syndrome, Ruvalcaba–Myhre syndrome, and Laugier–Hunziker syndrome were ruled out. An array of benign conditions must be considered in the differential diagnosis of these hyperpigmented genital lesions. The key features that discriminated our case from lichen planus were the absence of papular eruptions prior to onset of the hyperpigmentation along with a non-supportive histopathology.
Morphologically they vary from diffuse to irregular well-demarcated macules. The unique feature in our case was the linear presentation resembling a “sketch mark”; we were unable to find any previous reports of a similar presentation.
| 1. |
Rosai J. Rosai and ackerman's surgical pathology. 9th ed. New York: Mosby; 2004.
[Google Scholar]
|
| 2. |
Barnhill RL, Rabinovitz H. Benign Melanocytic Neoplasms. Dermatology In: Bolognia JL, Jorizzo JL, Rapini RP, editors. 2nd ed. British Library Cataloguing in Publication Data. 2008. p. 1717-20.
[Google Scholar]
|
| 3. |
Newton Bishop JA. Lentigos, Melanocytic Naevi and Melanoma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Vol. 54. A John Wiley and Sons Ltd, Publication; 2010. p. 54-6.
[Google Scholar]
|
| 4. |
Recuz J, Clerici T. Penile melanosis. J Am Acad Dermatol 1989;20:567-70.
[Google Scholar]
|
| 5. |
Lenane P, Keane CO, Connell BO, Loughlin SO, Powell FC. Genital melanotic macules: Clinical, histological, immunohistochemical, and ultrastructural features. J Am Acad Dermatol 2000;42:640-4.
[Google Scholar]
|
Fulltext Views
20,661
PDF downloads
1,694





