Translate this page into:
Coexistence of two types of clinical lesions in childhood-onset mastocytosis
2 Department of Pathology, University Complex Hospital of Vigo, Spain
Correspondence Address:
Lidia P�rez-P�rez
Department of Dermatology, University Complex Hospital of Vigo, C/ Porri�o 5, 36209 Vigo (Pontevedra)
Spain
| How to cite this article: P�rez-P�rez L, Allegue F, Caeiro JL, Fabeiro JM, Rodr�guez AP, Zulaica A. Coexistence of two types of clinical lesions in childhood-onset mastocytosis. Indian J Dermatol Venereol Leprol 2011;77:184-187 |
Abstract
The vast majority of mastocytosis appear in childhood, urticaria pigmentosa (UP) and mastocytomas being the most common types. Terms such as "xanthelasmoid mastocytosis", "pseudoxanthomatous mastocytosis" or "nodular mastocytosis" have been introduced in the literature to describe the presence of yellowish papular or nodular lesions. We describe two children with cutaneous mastocytosis showing yellowish lesions in combination with other skin lesions. A 10-year-old girl presented with asymptomatic lesions in her vulva at birth, and developed brownish macules on her trunk years after. An eight- year-old boy presented with multiple yellowish papular lesions on his trunk, neck and limbs coexisting with a few clinically anetodermic lesions. No systemic involvement was found and the skin biopsy confirmed a cutaneous mastocytosis in both cases. The two patients are currently asymptomatic and are being periodically followed up. Mastocytoses may show a variety of clinical lesions, sometimes leading to misdiagnosis. Although there are previous reports, involvement of the mucosae and secondary anetoderma are not common findings in cutaneous mastocytoses. We consider that cutaneous manifestations of mastocytoses compose a clinical spectrum, thus explaining the coexistence of different clinical lesions and the development of uncommon presentations.Introduction
Cutaneous mastocytoses are uncommon infiltrative diseases of the skin. Urticaria pigmentosa (UP) and mastocytomas are the most frequent types of mastocytoses in childhood. [1],[2] Secondary anetoderma and genital lesions are rare clinical presentations. The latter can be difficult to distinguish from histiocytoses and other xanthomatous diseases and therefore these disorders must be also considered in the differential diagnosis. We report two children who presented with yellowish lesions in conjunction with other cutaneous manifestations.
Case Reports
Case 1
An otherwise healthy 10-year-old girl came to our clinic with a history of asymptomatic vulval lesions since birth, which had been growing in size and number. On clinical examination, she presented several firm, well-defined, round to oval, yellowish plaques in the labia majora [[Figure - 1]a], with a negative Darier′s sign. Brownish macules were evident on her neck and upper trunk [[Figure - 1]b], with a positive Darier′s sign. The general physical examination was otherwise normal.
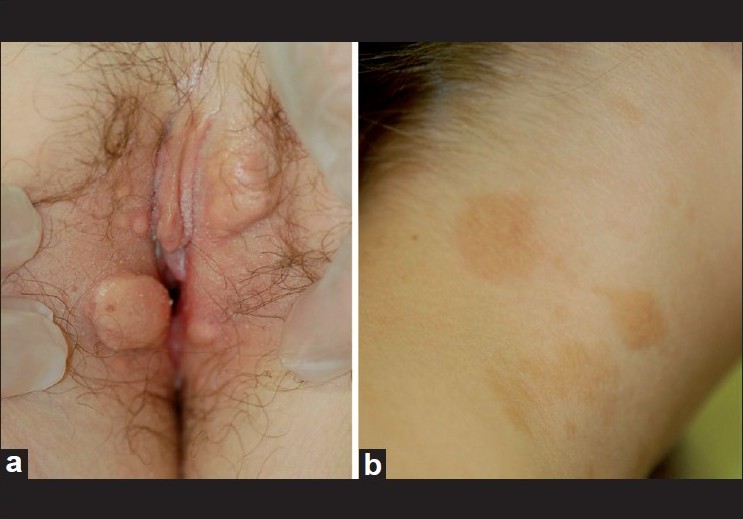 |
| Figure 1: (a) Well-defined, yellowish plaques on the labia majora, (b) brownish macules on the right lateral aspect of the neck |
A blood examination including serum tryptase and serum lipid levels was within the normal ranges. Urinary histamine was normal.
A biopsy taken from a vulval lesion [Figure - 2] showed a dermal proliferation of epithelioid cells, showing homogeneus rounded nuclei and cytoplasmatic granules, which stained positive with toluidin blue and CD117 [Figure - 3]. Staining with cytokeratin AE 1- AE3, CD68, S-100, CD 1a and CD 138 was negative. Abdominal ultrasound and bone X-ray were normal. Since the patient had no symptoms, no systemic treatment was started.
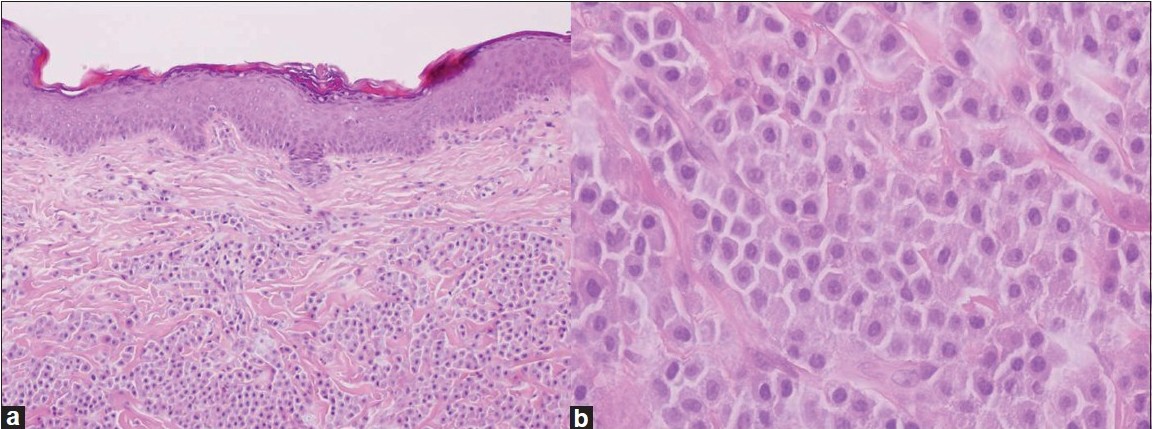 |
| Figure 2: Dermal proliferation of epithelioid cells, with clear and granular cytoplasms. (a) (H and E, ×100), (b) (H and E, ×400) |
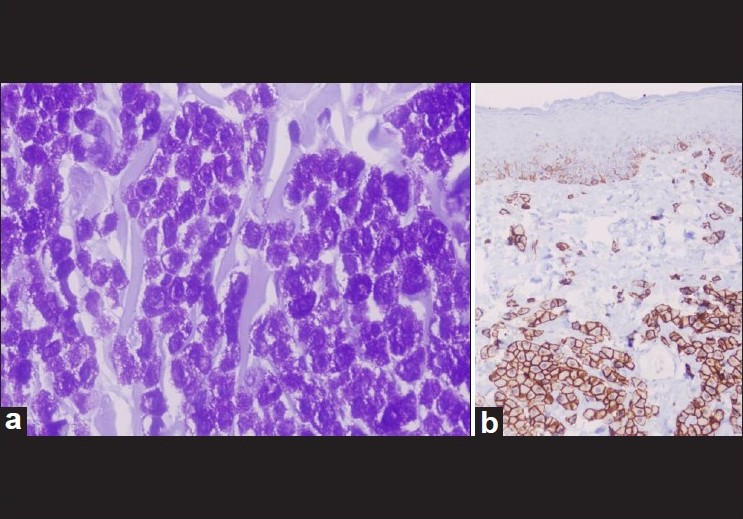 |
| Figure 3: Positive staining with toluidin blue (a) and CD117 (KIT) (b) ×400 both |
Case 2
An eight-year-old boy came to our clinic for assessment of multiple brownish macules, ranging in size from several millimetres to 1 cm, located on his trunk and limbs [[Figure - 4]a]. Some of these lesions were nodular and showed a yellowish color, firm consistency and a positive Darier′s sign [[Figure - 4]b]. He also presented a small number of clinically anetodermic lesions, mainly on the right lateral aspect of his neck [[Figure - 4]c]. A skin biopsy taken from one of the yellowish lesions showed a dense dermal infiltrate constituted mainly by fusiform cells with rounded nuclei and eosinophilic cytoplasms. Giemsa and toluidin blue staining showed abundant cytoplasmic metachromatic granules. Skull X-ray, chest X-ray, abdominal ultrasound, complete hemogram and serum biochemistry were all normal. Serum tryptase levels were slightly raised (14.2 mcg/l; normal limit: 13.5 mcg/l). Serum histamine and adrenaline metabolites were within the normal ranges. General recommendations (avoidance of physical and chemical stimuli such as scratching of the skin, sudden changes in temperature and codeine) were provided and treatment with antihistamines (dexchlorpheniramine maleate, 0.35 mg/kg given in divided doses in every 6 h) was started. Control of the symptoms was obtained one month later. The patient was sent for assessment to our mastocytosis referral center in Spain (Mastocytoses Studies Center; Virgen del Valle Hospital, Toledo, Spain). He is currently asymptomatic and on follow-up.
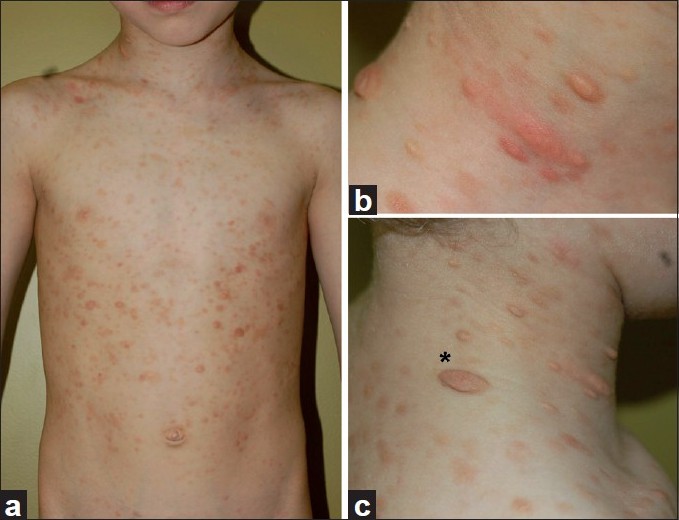 |
| Figure 4: (a) Multiple brownish macules and yellow papules on trunk and limbs, (b) Yellowish nodular lesions with a positive Darier's sign, (c) anetodermic lesions (asterisk) on the right lateral aspect of the neck |
Discussion
Up to 65% of the mastocytosis are found in children, UP and mastocytomas being the most common types. [1],[2],[3] UP is characterized by the presence of widespread monomorphic brownish-reddish macules or papules that mainly appear on the trunk and limbs and typically show a positive Darier′s sign. This sign is considered as pathognomonic of cutaneous mastocytosis, although it is not 100% specific [4] and may be negative in some cases. Mastocytomas generally appear as solitary or a few well demarcated red, yellowish or pink lesions that usually involute in a few years.
The introduction of different descriptive terms regarding cutaneous mastocytoses [5],[6],[7],[8],[9],[10],[11] has contributed to create some confusion among physicians. The term "xanthelasmoid mastocytosis" ("xanthelasmoidea") was coined by Fox in 1875 [5] to describe the presence of yellowish papules or nodules which resembled xanthelasma (he stated "acute general xanthelasma" would be a term that "would roughly describe the disease" in the cases he reported). Several years later, Thomas Colcott Fox [6] provided a summary of 19 similar cases reported until 1883. All of them were seen in children with ages ranging from three days to five months and some of them presented also "brown or tawny olive stains" ("pigmented spots, patches or macules" or "brownish-drab rounded areas") similar to those seen in UP, as observed in patient 1.
The term "nodular mastocytosis" has been used by some authors to describe nodular yellow-cream lesions, which can appear as localized or disseminated. Griffiths and Daneshbod [11] described in 1975 a patient with disseminated yellow nodules with a negative Darier′s sign and coined the term "pseudoxanthomatous mastocytosis" in allusion to the similarity of the lesions to xanthomas and pseudoxanthoma elasticum. The authors considered this descriptive term more appropriate than "xanthelasmoid mastocytosis" although they assumed that their case only differs from that described by Tilbury Fox in the persistence of their patient′s lesions. However, in view of the clinical pictures published to date, the terms "xanthelasmoid", "nodular" and "pseudoxanthomatous" [mastocytosis] describe all the same clinical condition with slight variations and therefore could be considered as synonyms.
Although genital yellowish papulo-nodular lesions have been already reported, they are a rarely seen feature in mastocytoses [7],[8],[12] and must be distinguished from other similar disorders, including xanthogranuloma, Langerhans cell histiocytosis, pseudoxanthoma elasticum and xanthoma. Vulval xanthelasmoid lesions in patient 1 preceded the development of brownish papules and macules and were the only cutaneous feature of mastocytosis for years.
Secondary anetoderma as shown in patient 2 is seldom seen in mastocytosis. [13],[14] Mast cells are considered to play a relevant role in the development of anetodermic lesions, as they release different mediators which can interfere in the synthesis of collagen and promote the fragmentation of the elastic fibers. Moreover, the chemotactic substances released during the mastocyte degranulation induce the accumulation of eosinophils, neutrophils and macrophages which might also promote elastase activity. [14] Epithelioid cells with metachromatic granules as seen in the dermal infiltrate in our first patient have been described in other patients with cutaneous mastocytoses. [15]
The importance of the two cases presented herein relies on the fact that both patients developed different presentations of childhood mastocytosis and showed coexistence of different and well-defined types of lesions.
We consider that the clinical variety of cutaneous lesions, as described herein, reveals the wide and dynamic clinical spectrum of mastocytosis. Whether or not the presence of yellowish papules/nodules deserves to be considered as an independent type of mastocytosis has not been yet firmly established, but it seems more sensible to interpret these lesions in the context of the aforementioned clinical spectrum.
Acknowledgements
We are very grateful to Dr. Joaquνn Gonzαlez-Carrerσ Fojσn (Department of Pathology, University Hospital Complex of Vigo, Spain), who kindly provided the histopathological figures of patient 1.
| 1. |
Inamadar AC, Palit A Cutaneous mastocytosis: report of six cases. Indian J Dermatol Venereol Leprol 2006;72:50-3.
[Google Scholar]
|
| 2. |
Ritambhra, Mohan H, Tahlan A. Urticaria pigmentosa. Indian J Dermatol Venereol Leprol 2001;67:33-4.
[Google Scholar]
|
| 3. |
Kiszewski AE, Duran-Mckinster C, Orozco-Covarrubias L, Gutiérrez-Castrellón, P, Ruiz-Maldonado R. Cutaneous mastocytosis in children: A clinical analysis of 71 cases. J Eur Acad Dermatol 2004;18:285-90.
[Google Scholar]
|
| 4. |
Surjushe A, Jindal S, Gote P, Saple DG. Darier's sign. Indian J Dermatol Venereol Leprol 2007;73:363-4.
[Google Scholar]
|
| 5. |
Fox T. On xanthelasmoidea (an undescribed eruption). Trans Clin Soc London 1875;8:53-7.
[Google Scholar]
|
| 6. |
Fox TC. On urticaria pigmentosa or xanthelasmoidea. Med Chir Trans 1883;66:329-47.
[Google Scholar]
|
| 7. |
Revert A, Jordá E, Ramón D, Vergdeguer JM, Torres V, Pitarch A. Xanthelasmoid mastocytosis. Pediatr Dermatol 1991;8:152-4.
[Google Scholar]
|
| 8. |
Serarslan G, Atik E, Zeteroglu S. Nodular mastocytosis of the vulva: an unusual localisation. Aust N Z J Obstet Gynaecol 2005;45:335-36.
[Google Scholar]
|
| 9. |
Kasprowicz S, Chan I, Wall DJ. Nodular mastocytosis. J Am Acad Dermatol 55;2:347-9.
[Google Scholar]
|
| 10. |
Srivastava N, Chand S, Singh S. Pseudoxanthomatous mastocytosis. Int J Dermatol 2008;47:50-1.
[Google Scholar]
|
| 11. |
Griffiths WAD, Daneshbod K. Pseudoxanthomatous mastocytosis. Br J Dermatol 1975;93:91-5.
[Google Scholar]
|
| 12. |
Shuangshoti S, Shuangshoti S, Pintong J, Piyayotai V, Sukpanichnant S. Solitary mastocytoma of the vulva: Report of a case. Int J Gynecol Pathol 2003;22:401-3.
[Google Scholar]
|
| 13. |
Del Pozo J, Pimentel MT, Paradela S, Almagro M, Martínez W, Fonseca E. Anetodermic mastocytosis: Response to PUVA therapy. J Dermatolog Treat 2007;18:184-7.
[Google Scholar]
|
| 14. |
Kalogeromitros D, Gregoriou S, Makris M, Georgala S, Kempuraj D, Theoharides T. Secondary anetoderma associate with mastocytosis. Int Arch Allergy Immunol 2007;142:86-8.
[Google Scholar]
|
| 15. |
Dunst KM, Huemer GM, Zelger BG, Zelger B. A new variant of mastocytosis: Report of three cases clinicopathologically mimicking histiocytic and vasculitic disorders. Br J Dermatol 2005;153:642-6.
[Google Scholar]
|
Fulltext Views
4,606
PDF downloads
2,258





