Translate this page into:
Confocal laser microscope
Correspondence Address:
Sushil Pande
Department of Dermatology, Sent GS Medical College and KEM Hospital, Parel, Mumbai - 12
India
| How to cite this article: Misri R, Pande S, Khopkar U. Confocal laser microscope. Indian J Dermatol Venereol Leprol 2006;72:394-397 |
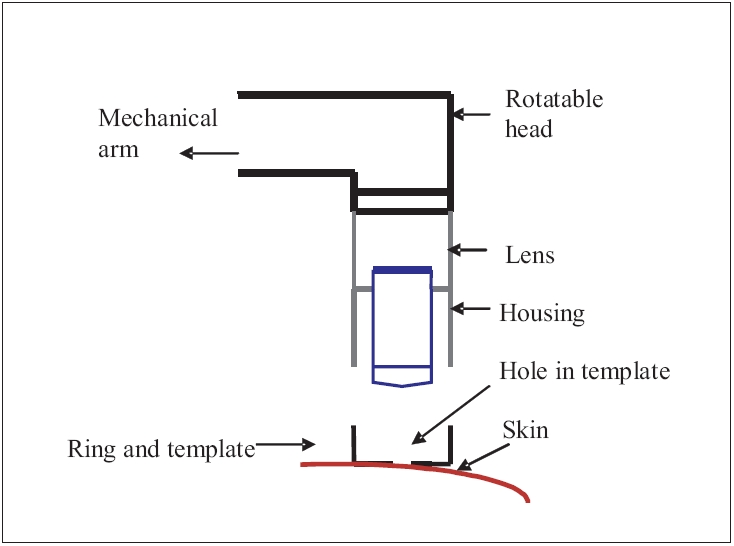 |
| Line diagram showing the structure of skin contact device of confocal laser microscope |
 |
| Line diagram showing the structure of skin contact device of confocal laser microscope |
 |
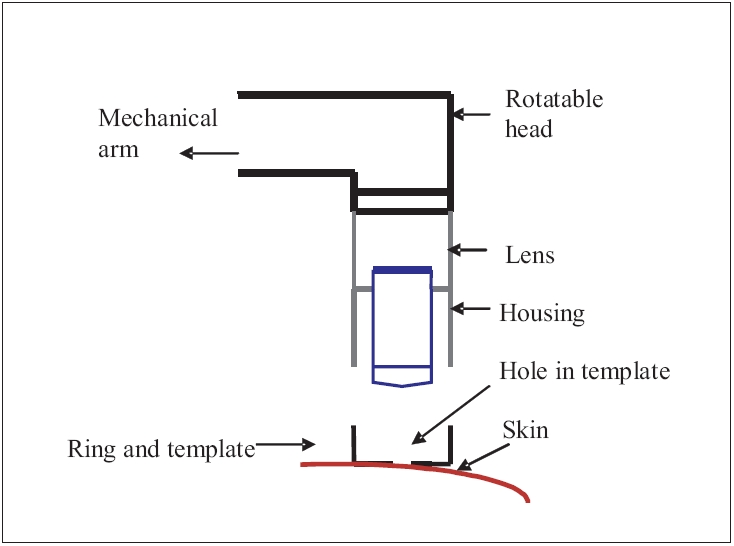
| Diagrammatic representation of principle of confocal microscopy |
 |
| Diagrammatic representation of principle of confocal microscopy |
 |
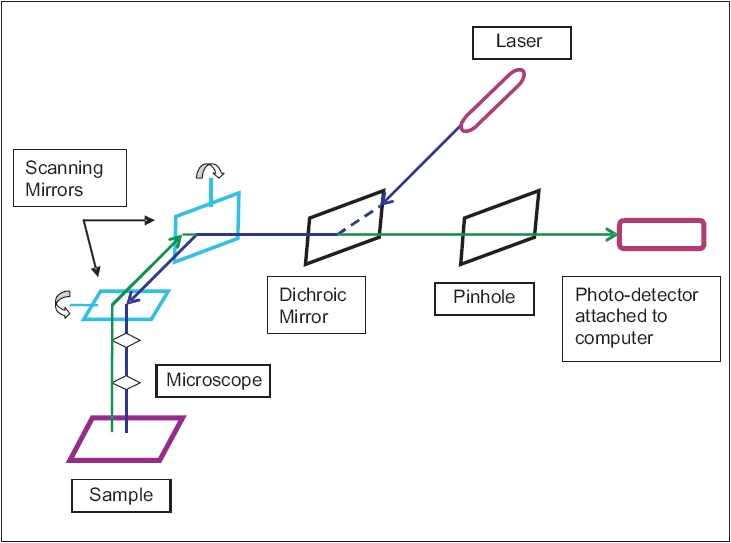
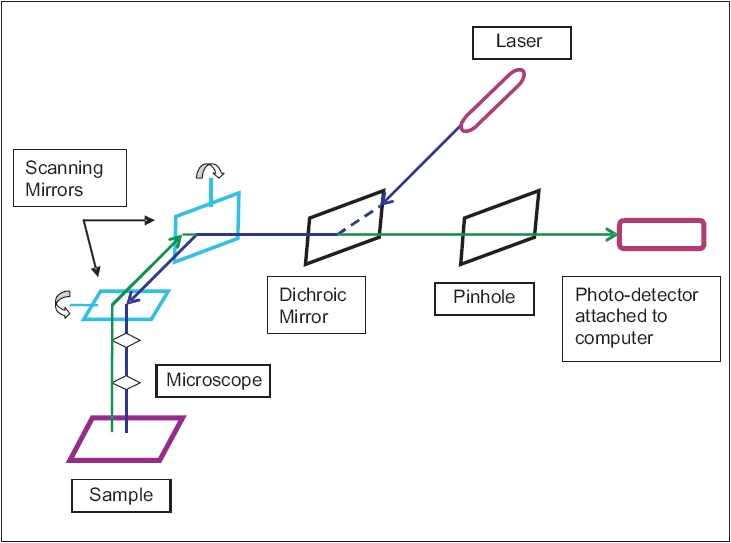
| Confocal microscope without skin contact device |
 |
| Confocal microscope without skin contact device |
Introduction
In vivo imaging of human epidermis and superficial dermis is a matter of interest for the dermatologist. The pursuit started with a magnifying glass, continues with a dermoscope and aims towards reaching new heights with the confocal laser microscope.
The confocal laser microscope is a novel and interesting noninvasive tool for imaging skin lesions and subsurface skin lesions that are not visible to the naked eye or even by dermoscopy. Skin can be imaged in vivo or freshly biopsied ( in vitro ) skin specimens can be visualized immediately without the processing that is required for routine histopathology.[1] Dynamic events (real time imaging) in the epidermis, papillary dermis and superficial reticular dermis to a maximum depth of 350 mm below the stratum corneum can also be visualized.[2] It has potential for diagnosing skin lesions with precision and could also become a tool for monitoring treatments in some cases.
The confocal microscope was invented by Marvin Minsky in 1955.[3] Since the advent of lasers there has been considerable improvement in the resolution, contrast, depth of imaging and field of view [Figure - 1]. Over the years a small, portable confocal microscope similar to a dermoscope has been developed.
Mechanism of confocal microscopy
It is based on the principle[4] that when a diode laser beam is passed through the skin, reflected light is used to construct detailed images of optical sections through the tissue [Figure - 2].
A laser provides excitation light of high intensity. The laser light is reflected from a dichroic mirror. From there, it hits two mirrors which scan the laser across the sample. Emitted light from the sample gets descanned by the dichroic mirror and is focused onto the pinhole after which it gets measured by a detector, i.e., a photomultiplier tube.
At any moment, only one point of the sample is observed, a complete image of the sample is never formed. The detector attached to a computer helps in building up the image, one pixel at a time. The detection of backscattered light along with differences in tissue refractive index help in high resolution of cellular detail and contrast when examining thin sections thus making staining unnecessary.
Confocal microscopy and high resolution
Ordinarily, in fluorescence microscopy, the entire sample on being completely illuminated by the excitation light is fluorescing. The highest intensity of the excitation light is at the focal point of the lens; however, other parts of the sample do get some of this light and fluoresce. This leads to a background haze in the resulting image. This problem is solved by adding a pinhole/screen. The pinhole being conjugate to the focal point of the lens is a confocal pinhole and hence this is known as confocal microscopy. The image is formed from a thin section of the sample. Thus by scanning many thin sections of the sample, a very clear three-dimensional image of the sample is formed. It has better resolution horizontally, as well as vertically.
The imaging depth is directly proportional to the wavelength, the epidermis is imaged with visible 400-700 nm wavelengths; the superficial papillary dermis and blood cells (erythrocytes and leukocytes) in the deeper capillaries are imaged with the near infrared 800-900 nm wavelengths.[5]
Types of lasers that are used in confocal microscopy are Argon ion laser, Helium-Neon laser and Xenon laser.
Instrument and method of use
Continued research has led to the development of a user-friendly confocal microscope with flexible operating systems unlike earlier models that were large, immobile and unstable and hence only limited areas of the body could be imaged. For stable imaging at different sites on the body, a skin-to-confocal microscope contact device was developed. The microscope is supported on a stand that can be raised or lowered according to the skin site to be imaged.[1] An extended arm (attached to the microscope) with a rotatable head allows easier access to different sites on the arms, legs, back, trunk, face, neck and head [Figure - 3].
The skin-contact device encloses the objective lens, a ring and template in housing. The ring and template is attached to the skin with double-sided tape or liquid. The ring forms a well on the skin which holds the immersion medium. The template has a hole which is centered over the site. The subject is placed either directly below or next to the objective lens and the stand is lowered or raised as necessary. The arm is oriented in such a way as to cause the ring and template to get engaged and thus lock into the housing. The skin within the template hole then remains laterally stable relative to the objective lens even though the subject may be moving.
Recent advances have led to the development of a handheld instrument. Skin is swabbed with a fluorescent dye.[6] After pressing the microscope′s handheld probe against the skin one can study the resulting images displayed on a computer monitor.
Uses in dermatology
- Microscopic analysis of skin structures (including hairs and nails) and components at different anatomic sites and in different conditions both physiological and pathological.[7],[8],[9]
- In vivo imaging of skin lesions and their margins minimizing the need for skin biopsy.
- To detect malignant changes in actinic keratoses and other premalignant conditions[10] and to study morphological differences between benign and malignant pigmented skin lesions leading to diagnosis of melanoma in situ .[11],[12]
- For diagnosis of dermatophyte infections, to identify fungal hyphae within the stratum corneum after potassium hydroxide application.[13]
- For in vivo noninvasive visualization of mite, Sarcoptes scabiei.[14]
- To monitor treatment for skin disorders e.g., in psoriasis to assess reduction in activity of T-cells after steroid thrapy.[6]
- Confocal laser microscope has been used to visualize dynamic events at the cellular level in conditions like allergic contact dermatitis, folliculitis etc.[15],[16]
- In vivo imaging of intradermal tattoos for accurate laser treatment.[17]
- To study the hair abnormalities in trichothiodystrophy.[18]
- To characterize Merkel cells on vellus hair follicles of the facial region and study Merkel cell carcinoma.[19]
- To study the influence of liphophilicity and vehicle composition on permeation of a drug in a hair follicle.[20]
- To quantify the number of Langerhans cells and other epidermal cell nuclei per volume unit in skin biopsies. A study has found a single Langerhans cell to be present per 53 epidermal cells.[21]
Many other uses are being explored for dermatological indications.
Pros and cons of confocal laser microscope
Advantages of confocal microscopy include rapid, noninvasive technique allowing early diagnosis and management and high resolution images[2] as compared to CT scan, MRI and USG for dermatological use. Disadvantages of confocal microscopy include its high cost and relatively smaller field of vision.
Confocal microscopy is currently in a stage of development. Newer modifications in the technique are taking place by leaps and bounds. At present, though its use is limited for the purpose of research, the confocal laser microscope may have enormous clinical implications for dermatology in future.
Acknowledgement
We thank Dr. K. Ghosh, Director, Indian Council of Medical Research, Mumbai and Dr. Aruna Pawar, In-charge, Confocal laser microscope, Institute of Immunohematology, Indian Council of Medical Research, Mumbai for providing the photograph of Confocal laser microscope.
| 1. |
Rajadhyaksha M, Gonzalez S, Zavislan JM, Anderson RR, Webb RH. In vivo confocal scanning laser microscopy of human skin II: Advances in instrumentation and comparison with histology. J Invest Dermatol 1999;113:293-303.
[Google Scholar]
|
| 2. |
Selkin B, Rajadhyaksha M, Gonzalez S, Langley RG. In vivo confocal microscopy in dermatology. Dermatol Clin 2001;19: 369-77.
[Google Scholar]
|
| 3. |
Post-gazette.com. PG News. Seeing skin deep: Special microscope gives live views of cells http://www. pittsburghpostgazette.com/healthscience/20000110confocal1.asp, Jan 10, 2000. Last accessed: July 13, 2006.
[Google Scholar]
|
| 4. |
Emory's Physics Department. Department of Physics. http://www.physics.emory.edu/~weeks/confocal/. Last update:6/7/06
[Google Scholar]
|
| 5. |
Rajadhyaksha M, Grossman M, Esterowitz D, Webb RH, Anderson RR. In vivo confocal scanning laser microscopy of human skin: Melanin provides strong contrast. J Invest Dermatol 1995;104:946-52.
[Google Scholar]
|
| 6. |
Post-gazette.com. PG News. http://www.pittsburghpostgazette. com/healthscience/20000110conside2.asp Jan 10, 2000
[Google Scholar]
|
| 7. |
Corcuff P, Bertrand C, Leveque JL. Morphometry of human epidermis in vivo by real-time confocal, microscopy. Arch Dermatol Res 1993;285:475-81.
[Google Scholar]
|
| 8. |
Huzaira M, Rius F, Rajadhyaksha M, Anderson RR, Gonzalez S. Topographic variations in normal skin, as viewed by in vivo reflectance confocal microscopy. J Invest Dermatol 2001;116: 846-52.
[Google Scholar]
|
| 9. |
Hadjur C, Daty G, Madry G, Corcuff P. Cosmetic assessment of the human hair by confocal microscopy. Scanning 2002;24:59-64.
[Google Scholar]
|
| 10. |
Aghassi D, Anderson RR, Gonzalez S. Confocal laser microscopic imaging of actinic keratoses in vivo : A preliminary report. J Am Acad Dermatol 2000;43:42-8.
[Google Scholar]
|
| 11. |
Gerger A, Koller S, Kern T, Massone C, Steiger K, Richtig E, et al . Diagnostic applicability of in vivo confocal laser scanning microscopy in melanocytic skin tumors. J Invest Dermatol 2005;124:493-8.
[Google Scholar]
|
| 12. |
Busam KJ, Charles C, Lohmann CM, Marghoob A, Goldgeier M, Halpern AC. Detection of intraepidermal malignant melanoma in vivo by confocal scanning laser microscopy. Melanoma Res 2002;12:349-55.
[Google Scholar]
|
| 13. |
Markus R, Huzaira M, Anderson RR, Gonzalez S. A better potassium hydroxide preparation? In vivo diagnosis of tinea with confocal microscopy. Arch Dermatol 2001;137:1076-8.
[Google Scholar]
|
| 14. |
Longo C, Bassoli S, Monari P, Seidenari S, Pellacani G. Reflectance-mode confocal microscopy for the in vivo detection of Sarcoptes scabiei. Arch Dermatol 2005;141:1336.
[Google Scholar]
|
| 15. |
Gonzalez, S, Gonzalez, E, White, et al . Allergic contact dermatitis: Correlation of in vivo confocal imaging to routine histology. J Am Acad Dermatol 1999a;40:708-13.
[Google Scholar]
|
| 16. |
Gonzalez S, Rajadhyaksha M, Gonzalez-Serva A, White WM, Anderson RR. Confocal reflectance imaging of folliculitis in vivo : Correlation with routine histology. J Cutan Pathol 1999;26: 201-5.
[Google Scholar]
|
| 17. |
O'goshi K, Suihko C, Serup J. In vivo imaging of intradermal tattoos by confocal scanning laser microscopy. Skin Res Technol 2006;12:94-8.
In vivo imaging of intradermal tattoos by confocal scanning laser microscopy. Skin Res Technol 2006;12:94-8.'>[Google Scholar]
|
| 18. |
Liang C, Morris A, Schlucker S, Imoto K, Price VH, Menefee E, et al . Structural and molecular hair abnormalities in trichothiodystrophy. J Invest Dermatol 2006 May 25; [Epub ahead of print].
[Google Scholar]
|
| 19. |
Uchigasaki S, Suzuki H, Inoue K. Merkel cells in the vellus hair follicles of human facial skin: A study using confocal laser microscopy. J Dermatol 2004;31:218-22.
[Google Scholar]
|
| 20. |
McElwee KJ, Kissling S, Wenzel E, Huth A, Hoffmann R. Cultured peribulbar dermal sheath cells can induce hair follicle development and contribute to the dermal sheath and dermal papilla. J Invest Dermatol 2003;121:1267-75.
[Google Scholar]
|
| 21. |
Bauer J, Bahmer FA, Worl J, Neuhuber W, Schuler G, Fartasch M. A strikingly constant ratio exists between Langerhans cells and other epidermal cells in human skin. A stereologic study using the optical disector method and the confocal laser scanning microscope. J Invest Dermatol 2001;116:313-8.
[Google Scholar]
|
Fulltext Views
6,314
PDF downloads
2,877





