Translate this page into:
Congenital absence of skin and an absent twin
Correspondence Address:
Sivaprakasam Karthika
9, Thirumalaisamy Street, Namakkal, Tamil Nadu
India
| How to cite this article: Karthika S, Balaji G. Congenital absence of skin and an absent twin. Indian J Dermatol Venereol Leprol 2016;82:444-446 |
Sir,
A 1-day-old male baby weighing 2.25 kg was referred to the dermatology department for peculiar skin lesions on the abdomen. Vital signs, APGAR score and neonatal reflexes of the baby were normal. On examination, there were two bilaterally symmetrical, arcuate, atrophic scars on the abdomen. The scar on the right was 8 cm × 3 cm in size and that on the left 5 cm × 4 cm in size, both were interconnected by a fibrous band, forming an “M” shape [Figure - 1]. There were a few areas of depigmentation, hyperpigmentation and erythema within the scars. There were no ulcers or scars on the scalp or other parts of the body. Other systems were normal.
 |
| Figure 1: Bilaterally symmetrical arcuate, atrophic scars on the abdomen of a 1-day-old male baby |
The mother was a primigravida and had undergone treatment for infertility. There was no history of trauma, maternal infections or drug intake during pregnancy. An ultrasound study done at 7 weeks of pregnancy showed a viable twin intrauterine gestation that was monochorionic and monoamniotic [Figure - 2]a. The second study at 23 weeks showed a single intrauterine gestation with a live fetus [Figure - 2]b and the other twin was seen in the in the lower pole of the uterus as fetus papyraceus [Figure - 2]c. The last study at 33 weeks showed only one viable fetus with the other fetus totally resorbed [Figure - 2]d. The surviving baby was delivered by an emergency cesarean section 2 weeks before the expected date of confinement due to premature rupture of membranes and fetal distress. Macroscopic examination of the placental surface had showed no abnormalities. A skin biopsy was not performed as the mother did not consent to the procedure. Ultrasound study of the neonate's abdomen was unremarkable.
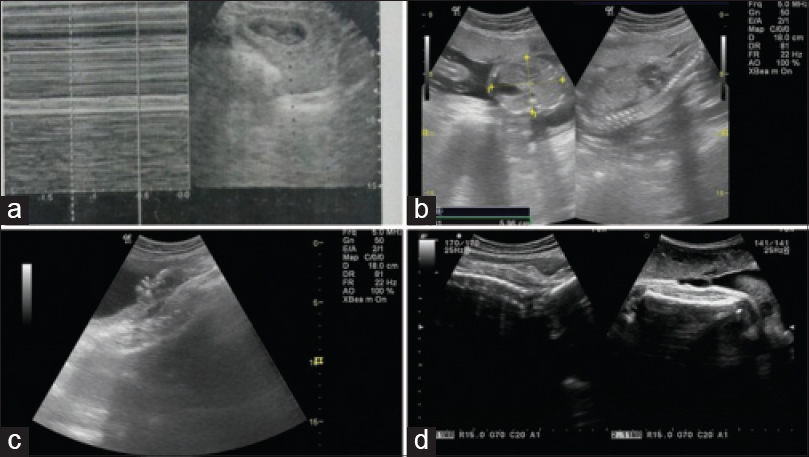 |
| Figure 2: (a) Ultrasound image showing monochorionic, monoamniotic intrauterine twin gestation at 7 weeks of pregnancy. (b) Ultrasound image showing single intrauterine gestation at 23 weeks of pregnancy. (c) Ultrasound image showing fetus papyraceus in the lower pole of the uterus at 23 weeks of pregnancy. (d) Ultrasound image showing single intrauterine fetus at 33 weeks of pregnancy |
Atrophic scars on the surviving fetus in a twin pregnancy along with documented fetus papyraceus and vanishing twin fits in with a diagnosis of group 5 aplasia cutis congenita in the present case. The baby was conservatively managed with gentle cleansing and bland emollients.
Aplasia cutis congenita or congenital absence of skin indicates a localized or widespread absence of skin at birth. While the term aplasia cutis congenita denotes a failure of skin development, congenital absence of skin is a broader term which includes conditions where the skin had developed initially but was lost later due to various causes.[1] Congenital absence of skin or aplasia cutis congenita accompanied by the delivery of fetus papyraceus (intrauterine fetal death with the stillborn fetus mummified or pressed flat by the growing live fetus) or vanishing twin (identification of multiple gestation with subsequent disappearance of one or more fetuses) or placental infarction has been classified under group 5 aplasia cutis congenita by Frieden.
In monochorionic monoamniotic twin pregnancies, as in our case, cutaneous infarction due to release of thromboplastin into the shared placenta after an intrauterine death could be a possible pathomechanism in the development of the skin lesions.[1] Temporary hypotension in the surviving fetus at the time of co-twin death can also lead to poor perfusion and skin necrosis.[2] Thus, the skin that is present at an early stage gets damaged and is subsequently lost.[1]
As in group 5 of Frieden's proposed classification of aplasia cutis congenita, initially normal skin is affected in-utero due to various factors in group 6 (associated with epidermolysis bullosa) and group 8 (caused by teratogens), also. Hence, these three groups could be segregated and preferably termed as congenital absence of skin instead of aplasia cutis congenita.
Congenital absence of skin associated with fetus papyraceus presents with a clinically distinct pattern of skin lesions characterized by single or multiple, almost symmetrical, linear, stellate or arcuate shaped ulcers or atrophic scars on the trunk and extremities. If the co-twin fetal death occurs early in gestation, the lesions tend to be smaller and the pattern may be linear, arcuate or triangular, involving the trunk predominantly. Late fetal demise is associated with larger, stellate or angular lesions and location on extremities.[2] Also, it is more likely that lesions that form in early gestation may heal before delivery and appear as fibrotic scars whereas less mature defects may present as ulcers or erosions at birth.[3] Therefore, the truncal, arcuate-shaped atrophic scars in our case represent early fetal demise of the co-twin.
Aplasia cutis congenita has to be differentiated from epidermolysis bullosa and bullous dermolysis of the newborn as they also present with skin erosions at birth. However, in these entities, fresh bullae appear even after birth on exposure to trivial trauma.
Mazza et al. had diagnosed aplasia cutis congenita group 5, in-utero, by detecting smaller abdominal circumference on prenatal ultrasound in a case that fulfilled other criteria.[4] However, in our case, the abdominal circumference of the live fetus was 166 mm at 22 weeks of gestation, which almost corresponded to the gestational age.
Recently, there is an increasing trend of multiple pregnancies as a result of infertility treatment by ovulation induction. Moreover, the selective feticide that is sometimes performed to safeguard a precious pregnancy and avoid multiple births results in iatrogenic fetus papyraceus. Hence, more cases of congenital absence of skin in surviving co-twins following selective feticide are being reported.[1]
Prognosis depends on the size of the lesions and the associated organ malformations such as congenital pulmonary anomalies and duodenal and biliary atresia which have been reported in aplasia cutis congenita group 5.[5] Early diagnosis and management will prevent complications such as infection and bleeding. Dermatologists and neonatologists should be aware of this rare condition in multigestational pregnancies associated with the death of a co-twin or fetus papyraceus or vanishing twin.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Atherton DJ. Naevi and other developmental defects.In: Burns T, Breathnach, Editors. Rook's Textbook of Dermatology. 8th ed. Oxford: Blackwell Publishing Ltd; 2010, p. 18.98-01.
[Google Scholar]
|
| 2. |
Qureshi UA, Ahmed N. Type V aplasia cutis congenita. Ann Saudi Med 2010; 30:171-2.
[Google Scholar]
|
| 3. |
Ustüner P, Dilek N, Saral Y, Ustüner I. Coexistence of aplasia cutis congenita, faun tail nevus and fetus papyraceus. J Dermatol Case Rep 2013;7:93-6.
[Google Scholar]
|
| 4. |
Mazza JM, Klein JF, Christopher K, Silverberg NB. Aplasia cutis congenita in a setting of fetus papyraceus associated with small fetal abdominal circumference and high alpha-fetoprotein and amniotic acetylcholinesterase. Pediatr Dermatol 2015;32:138-40.
[Google Scholar]
|
| 5. |
Ramachandran S, Mishra K, Batra VV. Aplasia cutis congenita: A rare case with extensive symmetrically distributed lesions. J Assoc Physicians India 2014;62:274-6.
[Google Scholar]
|
Fulltext Views
4,662
PDF downloads
2,745





