Translate this page into:
Congenital erosive and vesicular dermatosis healing with reticulated supple scarring: Report of four cases
2 Department of Dermatology, Cutis Academy of Cutaneous Sciences, Bengaluru, Karnataka, India
Correspondence Address:
Sahana M Srinivas
Department of Pediatric Dermatology, Indira Gandhi Institute of Child Health, Bengaluru, Karnataka
India
| How to cite this article: Srinivas SM, Mukherjee SS, Hiremagalore R. Congenital erosive and vesicular dermatosis healing with reticulated supple scarring: Report of four cases. Indian J Dermatol Venereol Leprol 2018;84:73-75 |
Sir,
Congenital erosive and vesicular dermatosis, first reported by Cohen et al. in 1985, is a rare disorder characterized by erosions and vesicles at birth, which heal within the first month of life leaving scars with a distinctive supple and reticulated texture.[1] There are 32 cases published in literature and none from the Indian scenario. We report four cases of congenital erosive and vesicular dermatosis (two sets of siblings) from two unrelated families who presented to our outpatient department at Indira Gandhi Institute of Child Health with reticulated soft supple scarring on extremities. Two otherwise healthy female siblings of the first family, born at term, of an uneventful pregnancy, 8 years and 4 years with second degree consanguineous parents, presented with multiple scars on the upper and lower limbs since the age of one month. Both siblings had history of erosions on forearms, lower limbs, hands, and feet at birth gradually healing in 20 days to leave behind reticulate scarring. There was no history of vesicles or erosions after the neonatal period or any systemic complications, although hyperthermia was reported in both children. Family history was non-contributory. General physical examination and developmental milestones were normal. Cutaneous examination of both siblings showed linear and reticulate soft and supple areas of hypopigmented and hyperpigmented scarring present symmetrically on the flexor aspect of arms, extensor aspect of lower limbs, dorsum of hands and feet [Figure - 1] and [Figure - 2].
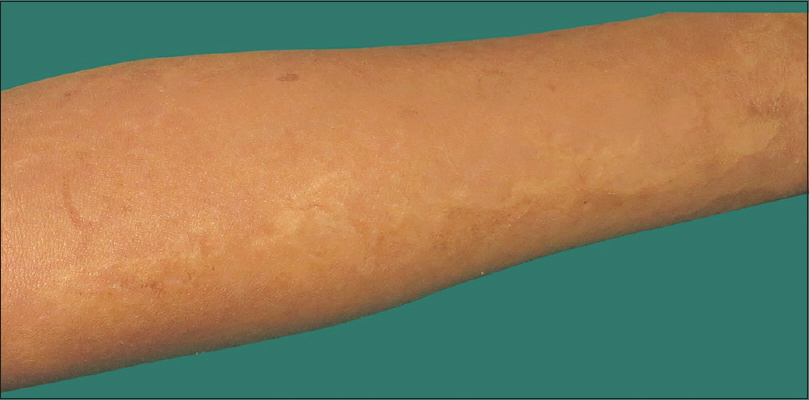 |
| Figure 1: Multiple hypopigmented, reticulate supple scarring on the flexor aspect of forearm in sibling 1 of family 1 |
 |
| Figure 2: Multiple linear and reticulated supple scarring on dorsum of hand and extensor aspect of lower legs and dorsum of feet in sibling 2 of family 1 |
The second family reported two healthy male siblings of age 7 years and 5 years, born at term of an uneventful pregnancy, out of a consanguineous marriage with similar history of erosions on upper and lower limbs at birth, which gradually healed within 15 days to form reticulate scarring. General examination, motor and intellectual development was normal. Cutaneous examination of both siblings showed linear and supple reticulate scarring present bilaterally symmetrically on the flexor aspect of the forearm, dorsum of hand, feet, and lower limbs [Figure - 3] and [Figure - 4]. Oral mucosa, scalp, nails, palms, and soles were normal. Systemic examination and ophthalmological examination were normal in all the four children.
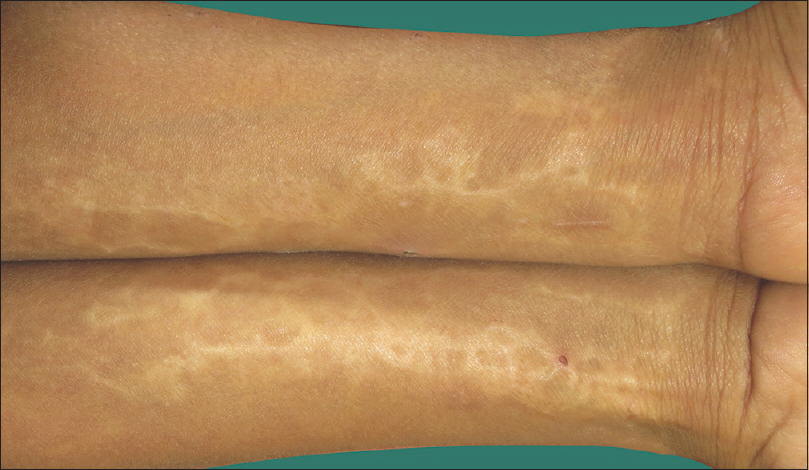 |
| Figure 3: Multiple reticulate supple scarring, bilaterally on the flexor aspect of forearms in sibling 1 of family 2 |
 |
| Figure 4: Reticulated supple scarring on the dorsum of hands in sibling 2 of family 2 |
Due to the retrospective nature of cases, we were unable to obtain results of any investigations done from the neonatal period or any antenatal records. Histopathology from both siblings from the first family showed atrophic epidermis with fibrotic dermis, absent hair follicles and eccrine glands indicative of scar [Figure - 5]. Immunofluorescence antigen mapping to rule out epidermolysis bullosa was normal. Skin biopsy was deferred in the second family as parents did not consent. Routine investigations in all cases were normal. Based on the history, clinical examination and the characteristic appearance of supple reticulated scarring, a diagnosis of congenital erosive and vesicular dermatosis healing with reticulated scarring was established. Due to cost constraints, gene sequencing was deferred.
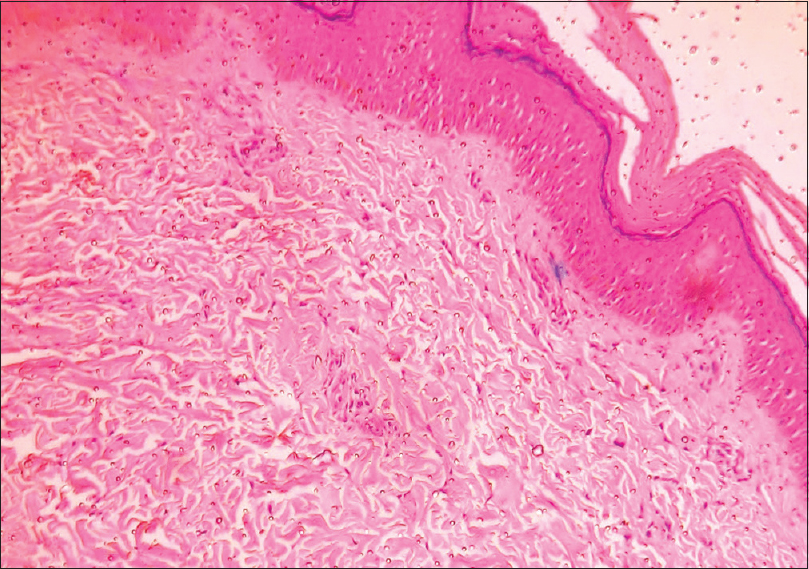 |
| Figure 5: Atrophic epidermis with increased collagenization in dermis indicative of scar (H and E, ×100) |
Congenital erosive vesicular dermatosis healing rapidly within the first month of life with reticulated supple scarring is a rare disorder presenting at birth with vesicles, erythema, erosions, ulceration, crusts and fissures affecting up to 75% of the body surface area without a genetic predisposition. Although the exact mechanism is unknown, etiopathogenesis proposed include birth trauma, premature rupture of membranes, intrauterine infections, chorioamnionitis, amniotic adhesions, purulent, or discolored amniotic fluid and a developmental defect with unusual healing in premature skin. Most of the cases reported in literature are preterm, although six affected term infants are described.[2],[3]
Clinically, scarring is seen along the long axis of extremities and the lines of cleavage on the trunk which may be hypopigmented, occasionally discrete, round and large with irregular borders. Generalized, supple reticulated scar occurs with alternating elevated and depressed areas commonly involving scalp, face, trunk, and extremities. Palms and soles are usually spared or less severely involved with rare flexural involvement.[4] They often have absent or hypoplastic nails, tongue atrophy, scarring alopecia, and hypohidrosis with heat intolerance secondary to paucity of eccrine glands in the areas of scarring and compensatory hyperhidrosis in healthy skin.[5]
Other features associated include neurodevelopmental abnormalities like seizures, cerebral palsy, mild hemiparesis, microcephaly, hydrocephalus and developmental delay. Ocular involvement includes corneal scarring, conjunctival inflammation, lacrimal duct obstruction and vitreous hemorrhage.[3],[4] History of recurrent vesicles after neonatal period has been reported.[5] Rare associations include sensorineural hearing loss, neonatal thrombocytopenia, dystrophic ears, erosive lichen planus, digital tip gangrene, murky appearance of amniotic fluid on prenatal ultrasound, and hydronephrosis.[5],[6] Histopathological features are varied as older lesions in all the cases reported in literature show scar formation, with or without decrease or absence of follicular or eccrine glands. It is still unclear whether associated features of congenital erosive vesicular dermatosis are per se because of the disease or prematurity.[5],[7] Differential diagnoses of congenital erosive vesicular dermatosis that should be considered in the neonatal period include congenital herpes simplex infection, staphylococcal scalded skin syndrome, epidermolysis bullosa, incontinentia pigmenti, focal dermal hypoplasia and autoimmune bullous disorders.[3] History, characteristic scarring and investigations like skin biopsy and immunofluorescence for antigen mapping did not support the above differential diagnoses in our case.
The uniqueness of our cases was the presence of only cutaneous involvement with no extracutaneous features. The above cases with similar findings in siblings may provide an insight into the pathogenesis of congenital erosive vesicular dermatosis, whether there is a possibility of genetic predisposition or any recurrent intrauterine pathology occurring during subsequent pregnancy. Genetic analysis may contribute, in future, to the further understanding of this condition.
Acknowledgement
Authors would like to acknowledge Dr. Asha Kubba, Consultant Dermatopathologist, Delhi Dermpath Laboratory, for performing immunofluorescence antigen mapping for our cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Cohen BA, Esterly NB, Nelson PF. Congenital erosive and vesicular dermatosis healing with reticulated supple scarring. Arch Dermatol 1985;121:361-7.
[Google Scholar]
|
| 2. |
Ma DL. Congenital erosive and vesicular dermatosis healing with reticulated supple scarring with extensive facial involvement. J Eur Acad Dermatol Venereol 2010;24:623-4.
[Google Scholar]
|
| 3. |
Tlougan BE, Paller AS, Schaffer JV, Podjasek JO, Mandell JA, Nguyen XH, et al. Congenital erosive and vesicular dermatosis with reticulated supple scarring: Unifying clinical features. J Am Acad Dermatol 2013;69:909-15.
[Google Scholar]
|
| 4. |
Mashiah J, Wallach D, Leclerc-Mercier S, Bodemer C, Hadj-Rabia S. Congenital erosive and vesicular dermatosis: A new case and review of the literature. Pediatr Dermatol 2012;29:756-8.
[Google Scholar]
|
| 5. |
Metz BJ, Hicks J, Levy M. Congenital erosive and vesicular dermatosis healing with reticulated supple scarring. Pediatr Dermatol 2005;22:55-9.
[Google Scholar]
|
| 6. |
Ciorba A, Corazzi V, Conz V, Tazzari R, Aimoni C. Sensorineural hearing loss in congenital erosive and vesicular dermatosis. J Int Adv Otol 2016;12:208-9.
[Google Scholar]
|
| 7. |
Heymann WR. Congenital erosive and vesicular dermatosis with reticulated supple scarring: Expanding the database of an enigma. Skinmed 2014;12:299-300.
[Google Scholar]
|
Fulltext Views
4,685
PDF downloads
2,058





