Translate this page into:
Dermatomyositis and nasopharyngeal carcinoma in an Indian patient
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
3 Department of Radiation Oncology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Somesh Gupta
Room 4066, Teaching Block, Fourth Floor, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Gupta V, Seshadri D, Vijay MK, Sahai P, Gupta S. Dermatomyositis and nasopharyngeal carcinoma in an Indian patient. Indian J Dermatol Venereol Leprol 2014;80:167-168 |
Sir,
Dermatomyositis is an idiopathic inflammatory myopathy with characteristic skin changes. Patients with dermatomyositis have a three- to eightfold increased risk for developing an associated malignancy compared with the general population. We describe a case of dermatomyositis and nasopharyngeal carcinoma treated successfully with concurrent chemo-radiation.
A 42-year-old man, resident of Manipur (in North Eastern India), presented with swelling and redness around eyes for the last 6 months. Ill-defined lilac erythema extended from the peri-orbital region to the cheeks and nasal bridge [Figure - 1]. Similar lilac erythema was present over the V area of chest, elbows, and knees. There were erythematous papules over the knuckles and interphalangeal joints of both hands. He had symmetrical proximal muscle weakness and myalgias for the last 6 months. The muscle power was 4+/5 for both proximal upper and lower limbs and 5/5 for both distal upper and lower limbs. In addition, he complained of non-progressive left-sided hearing loss for 1 year and intermittent nasal stuffiness for the last 4 months with an episode of epistaxis 5 months back. A clinical diagnosis of dermatomyositis was made and the nasal and ear symptoms were evaluated in consultation with the ENT department. Routine investigations showed no abnormality except for mild transaminitis. His creatine phosphokinase (CPK) and lactate dehydrogenase (LDH) levels were elevated (418 and 437, respectively; normal values being up to 226 and 420, respectively). Electromyographic studies were suggestive of a myopathic pattern. X-ray revealed a soft tissue density in the roof of the nasopharynx. A contrast CT scan of the head and neck showed a homogenous enhancing soft tissue mass in the nasopharynx [Figure - 2]a, which on histopathological examination showed syncytial-appearing large tumor cells with vesicular nuclei and large central nucleoli arranged in solid sheets and irregular islands intermingled with lymphocytes and plasma cells. Pancytokeratin stained the peripheral rim of cytoplasm, an appearance characteristic of undifferentiated carcinoma. Tumor cells were positive for epithelial membrane antigen (EMA) and Ebstein Barr Virus (EBV)-LMP1. On the basis of histomorphology and immunohistochemistry, a diagnosis of undifferentiated non-keratinizing nasopharyngeal carcinoma was made [Figure - 3]. The tumor was staged as T1N0M0 and was treated with concurrent chemoradiotherapy, while no specific treatment was instituted for dermatomyositis. After completing seven cycles of chemoradiotherapy, the nasopharyngeal mass disappeared [Figure - 2]b, while there was continuous improvement in his skin and muscle symptoms. The patient has now been off all treatment for 8 months with no evidence of either nasopharyngeal malignancy or dermatomyositis.
 |
| Figure 1: Heliotrope rash |
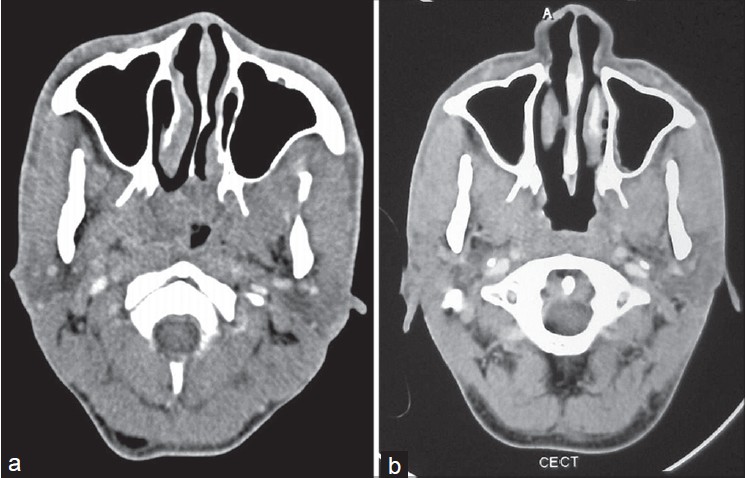 |
| Figure 2: CECT head and neck: Homogenous enhancing soft tissue mass in nasopharynx (a), and no mass seen in the nasopharynx following therapy (b) |
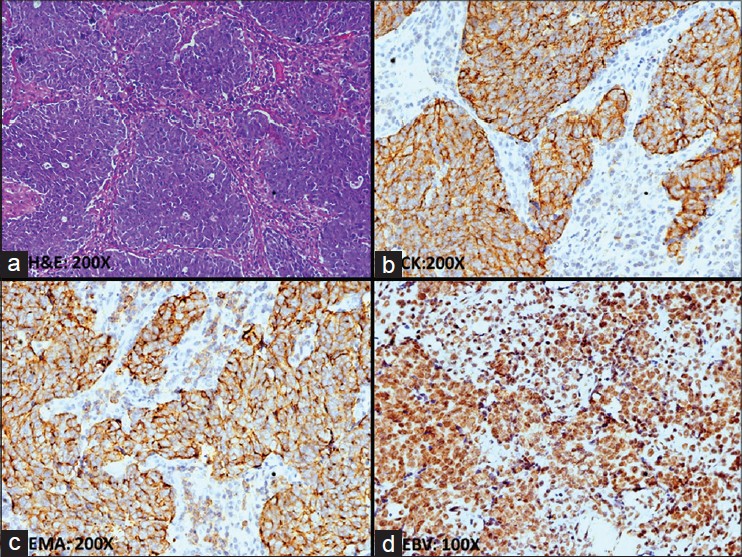 |
| Figure 3: Nasopharyngeal carcinoma, undifferentiated: the tumor is composed of sheets or bands of large undifferentiated cells that also contain a population of non-neoplastic small lymphocytes (a). These tumor cells are diffusely immunopositive for pancytokeratin (b), EMA (c), and EBV-LMP (d) |
The frequency of occurrence of malignancies in dermatomyositis patients varies from 15% to 60% in different series. The malignancy is usually an adenocarcinoma of the ovary, lung, or gastrointestinal tract in Western countries, and nasopharyngeal carcinoma in Southeast Asia and Northern Africa. Dermatomyositis precedes the neoplasm in 40%; both occur together in 26% or the neoplasm may occur first in 34%. The risk of detecting an associated malignancy is highest at the time of or within a year of the diagnosis of dermatomyositis. [1]
Although the association of dermatomyositis and nasopharyngeal carcinoma is well documented, [1],[2],[3] it is rare; the coexistence of dermatomyositis is seen in less than 1/1000 cases of nasopharyngeal carcinoma. [4] The association of dermatomyositis with nasopharyngeal carcinoma has been reported from Southern China, South-East Asia, North Africa, and the Alaskan Inuits, but to our knowledge this is the first report from India.
Various pathogenic mechanisms have been proposed for the association of dermatomyositis and nasopharyngeal carcinoma. EBV has been linked pathogenetically with both these conditions. [5] In our patient, immunostain for EBV-LMP1 was positive in the nasopharyngeal carcinoma specimen implicating EBV in the pathogenesis.
Most available literature suggests that dermatomyositis generally tends to improve with the treatment of nasopharyngeal carcinoma and it is the stage of the nasopharyngeal carcinoma that determines the overall prognosis. [3] Radiotherapy plays a central role in the treatment of all stages of nasopharyngeal carcinoma and may be combined with chemotherapy and surgery. Treatment of dermatomyositis can be carried out along conventional lines according to severity of symptoms. The use of systemic steroids appears to be safe and does not result in a significantly increased rate of metastasis.
We suspected nasopharyngeal carcinoma in our patient because of his ethnicity and symptoms referring to the nasopharynx, which were followed shortly by the onset of skin lesions and muscle weakness. Although treatment was directed only towards the malignancy, we noticed a simultaneous improvement of skin and muscle symptoms in conjunction with regression of nasopharyngeal carcinoma.
Awareness of paraneoplastic dermatomyositis in association with nasopharyngeal carcinoma will help in appropriate screening, especially in patients belonging to susceptible ethnic groups.
| 1. |
Hu WH. Nasopharyngeal carcinoma with dermatomyositis: An analysis of 30 cases. [Article in Chinese]. Zhonghua Zhong Liu Za Zhi 1986;8:133-5.
[Google Scholar]
|
| 2. |
Ang P, Sugeng MW, Chua SH. Classical and amyopathic dermatomyositis seen at the National Skin Centre of Singapore: A 3-year retrospective review of their clinical characteristics and association with malignancy. Ann Acad Med Singapore 2000;29:219-23.
[Google Scholar]
|
| 3. |
Hu WJ, Chen DL, Min HQ. Study of 45 cases of nasopharyngeal carcinoma with dermatomyositis. Am J Clin Oncol 1996;19:35-8.
[Google Scholar]
|
| 4. |
Chakroun A, Guigay J, Lusinchi A, Marandas P, Janot F, Hartl DM. Paraneoplastic dermatomyositis accompanying nasopharyngeal carcinoma: Diagnosis, treatment and prognosis. Eur Ann Otorhinolaryngol Head Neck Dis 2011;128:127-31.
[Google Scholar]
|
| 5. |
Chen DY, Chen YM, Lan JL, Chen HH, Hsieh CW, Wey SJ, et al. Polymyositis/dermatomyositis and nasopharyngeal carcinoma: The Epstein-Barr virus connection? J Clin Virol 2010;49:290-5.
[Google Scholar]
|
Fulltext Views
2,423
PDF downloads
1,464





