Translate this page into:
Dermoscopic monitoring of erythroplasia of Queyrat treated with photodynamic therapy
Corresponding author: Dr. Liang Zhao, Institute of Dermatology, Chinese Academy of Medical Sciences and Peking Union Medical College, 12 Jiang-Wang-Miao Road, Nanjing 210042, Jiangsu Province, China. zhaoliang210042@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wu M, Yang L, Li J, Zhao L. Dermoscopic monitoring of erythroplasia of Queyrat treated with photodynamic therapy. Indian J Dermatol Venereol Leprol 2021;87:396-9.
Sir,
Erythroplasia of Queyrat is a type of squamous cell carcinoma in situ that mainly occurs on the glans penis. Surgery is the standard treatment for erythroplasia of Queyrat. However, it can cause problems to the appearance and function of the penis. Photodynamic therapy is a non-surgical treatment modality. Feldmeyer et al. performed photodynamic therapy in 11 men with erythroplasia of Queyrat. After an average of 8 treatment sessions, 3 patients demonstrated complete remission, 4 showed partial remission, and 4 experienced progressive disease.1 Fai et al. conducted a retrospective analysis on 23 patients undergoing photodynamic therapy for erythroplasia of Queyrat, and after 2 treatment sessions, 83% of patients showed complete clinical remission.2 We report here a case of erythroplasia of Queyrat on the glans penis which was successfully treated by photodynamic therapy and evaluated the outcome using dermoscopy.
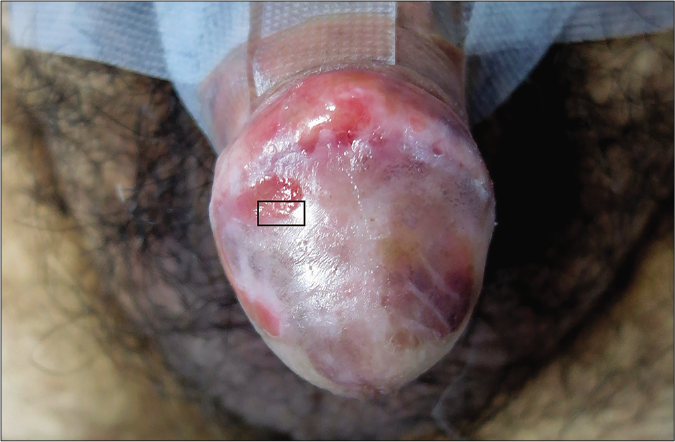
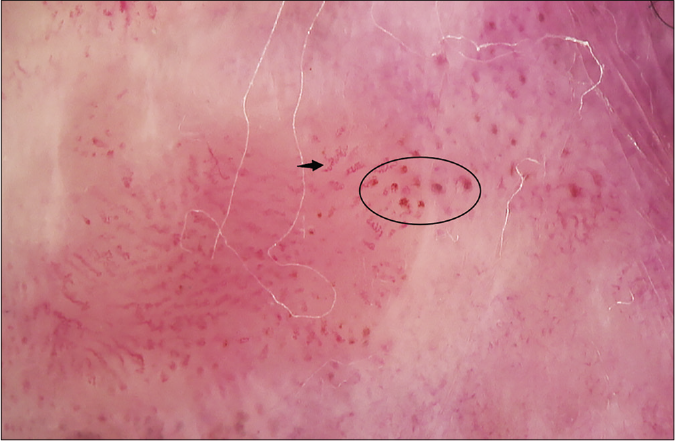
A 52-year-old man presented to our hospital in July 2017 with an erythematous plaque on his glans penis. Two years ago, he had developed an asymptomatic soybean-sized erythematous plaque on the glans penis which increased in size over the last one month and spread to the corona. The surface of the plaque was superficially eroded [Figure 1a]. The patient denied history of recent sexual contact and medical and family history was non-contributory. Dermoscopy (Derm DOC HR, Derma Medical Systems. Austria. Polarized light. 30×) revealed clustered glomerular blood vessels against a red background, some hairpin-like blood vessels, twisted blood vessels and small structureless red areas [Figure 1b]. Skin biopsy of the erythematous plaque showed disorderly arrangement of the atypical keratinocytes with some deeply stained pleomorphic nuclei. In addition, a moderately dense lymphocytic infiltrate was observed in the superficial dermis [Figures 1c and d]. Immunohistochemical analyses indicated positivity for Ki-67 (70%) [Figure 1e] and P16 [Figure 1f]. The result of human papillomavirus qualitative test was negative. Based on the above results, we confirmed the diagnosis of erythroplasia of Queyrat. Computed tomography of the chest and inguinal lymph nodes showed no abnormalities. The abdominal B mode ultrasonography was also normal.
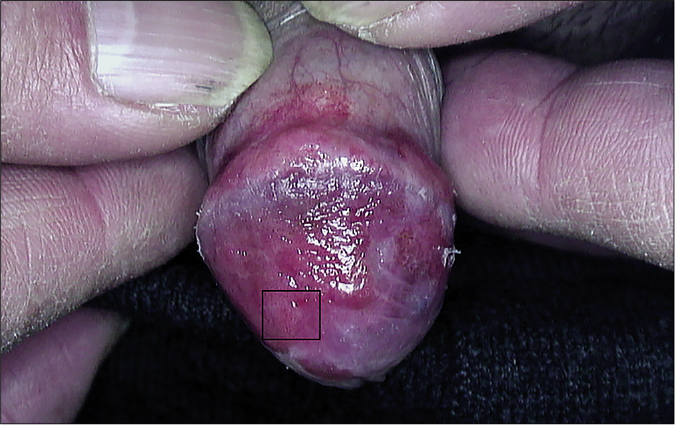
- Patient’s clinical presentation before photodynamic treatment. The rectangle shows exact scoped area
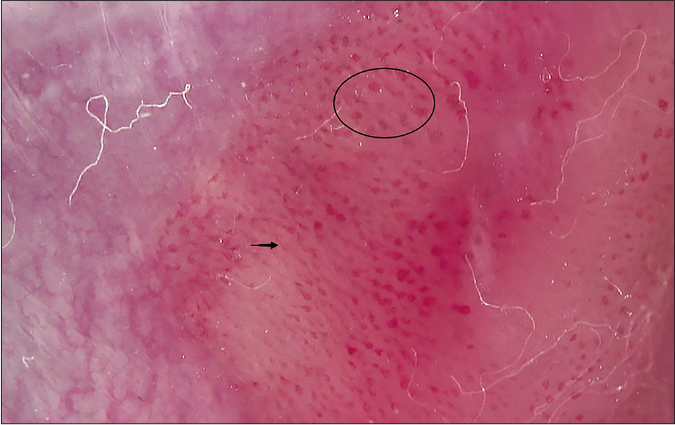
- Patient’s dermoscopy image before photodynamic treatment. The oval shape represents glomerular vessels. The arrow represents twisted blood vessels or hairpin-like blood vessels
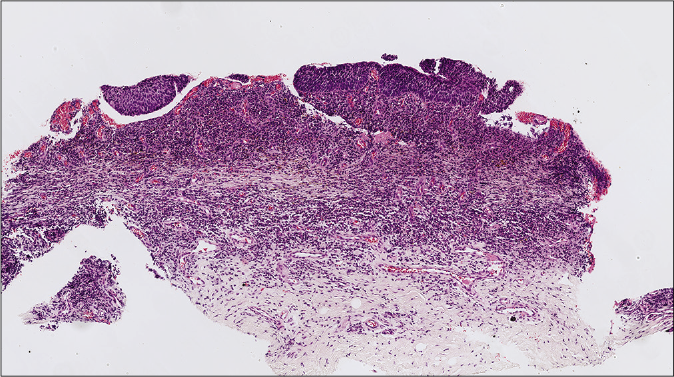
- Epidermis showing disorderly arrangement of keratinocytes and some deeply stained pleomorphic nuclei. Capillary proliferation and dense lymphocytes in the mid-dermis. (H and E, ×40)
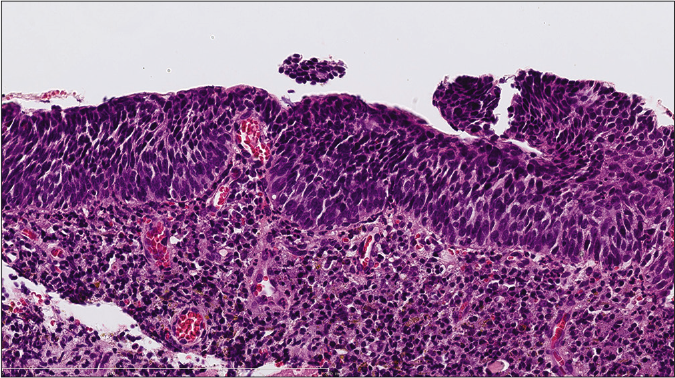
- Higher magnification showing dysplasia and nuclear pleomorphism (H and E, ×100 )
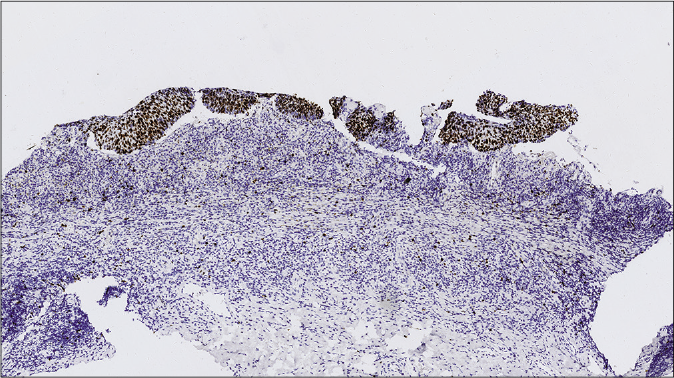
- Positive immunohistochemical staining result for positive Ki-67 (×40)
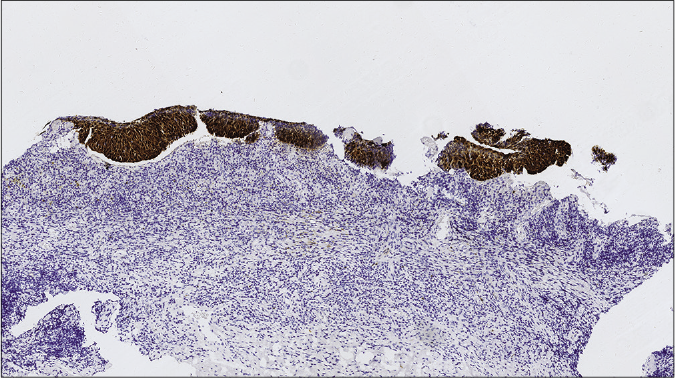
- Positive immunohistochemical staining result for P16 (×40)
The patient refused partial resection of the penis. He was hence treated with photodynamic therapy after obtaining informed consent. A thin-layered cotton soaked with 20% 5-aminolevulinic acid solution was used to cover the lesions for 3 hours, extending 1 cm beyond the lesion. It was then irradiated using red light (635 nm, 80 mw/ cm2) for 20 minutes. Treatments were repeated every 7-10 days. Dermoscopy was performed before each treatment session. At the 6th session, most of the skin lesions had disappeared [Figure 2a], and dermoscopy showed only a few glomerular vessels [Figure 2b]. By the 13th session, the lesions had completely disappeared [Figure 2c], dermoscopy showed almost no glomerular vessels [Figure 2d] and no subsequent treatment was administered. One year later (February 2019), brown pigmentation was seen on the left side of glans [Figure 2e]. A light red background and a few brown globules (considering hemosiderin deposits) were observed under dermoscopy [Figure 2f]. No obvious glomerular vessels were seen. The second biopsy was made in February 28, 2019 and showed no abnormality. Currently, the patient is being followed up.
- Clinical appearance of skin lesions after 6 sessions of photodynamic therapy (the rectangle shows exact scoped area)
- Dermoscopic image after the sixth treatment. The oval shape represents glomerular vessels. The arrow points to twisted blood vessels or hairpin-like blood vessels

- Patient’s clinical presentation after the 13th treatment. The rectangle shows exact scoped area
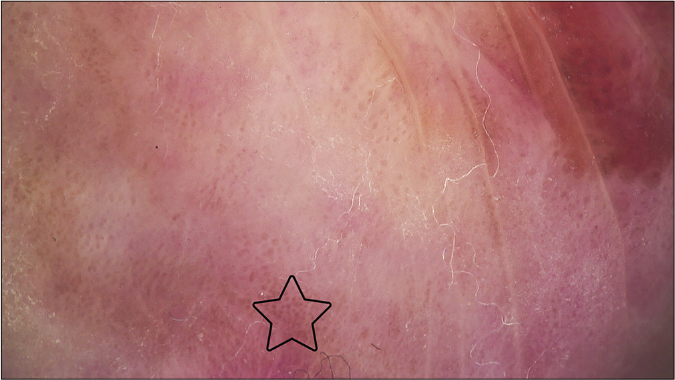
- Patient’s dermoscopy image after the 13th treatment. The star represents brown globules
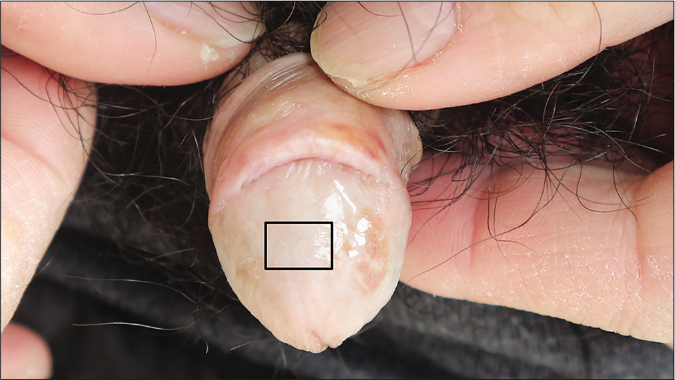
- Patient’s clinical presentation after 1 year follow up. The rectangle shows exact scoped area
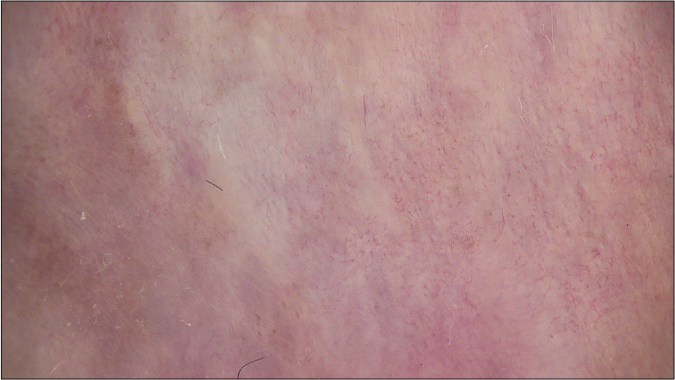
- Patient’s dermoscopy image after 1 year follow up
Although biopsy is the best way to evaluate the efficacy of skin tumor treatment, it is invasive. Dermoscopy is a convenient, noninvasive, inexpensive method of detection and plays an important role in the diagnosis and treatment evaluation of skin tumors.3 The characteristic manifestations of erythroplasia of Queyrat under dermoscopy are clustered or scattered glomerular blood vessels with different morphology, structureless red areas, linear blood vessels and erosion. Linearly arranged brown dots, scale and scar-like area can also be seen.4,5 In our case, glomerular vessels, hairpin-like vessels and small red structureless areas were observed. When the skin lesions clinically improved, the visible glomerular vessels and structureless red areas under the dermoscopy were significantly reduced. After 6 sessions of photodynamic therapy, the skin lesions of the patient had clinically resolved, but glomerular blood vessels and structureless red areas were still visible under dermoscopy. Thus it was speculated that the tumor had not been completely removed and the photodynamic therapy should be continued until the abnormal vessels completely disappeared under dermoscopy. Hence, 7 more sessions of photodynamic therapy were performed consecutively on the patient until these changes disappeared. The glomerular vessels did not reappear during the one year follow-up period and the skin lesions did not recur. Histopathological findings also confirmed the complete removal of the tumor. This indicated that dermoscopy would be useful in monitoring the treatment of erythroplasia of Queyrat and determining the endpoint of this therapy and could improve the accuracy of evaluation compared with clinical examination alone. The limitation of this study is that it is a report of a single patient. A larger case series would lend further support that dermoscopic disappearance of glomerular vessels equals histological cure and also determine the average number of therapy sessions required for erythroplasia of Queyrat to be dermoscopically negative. Only then can the need for a follow up biopsy be obviated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
(1) Scientific Research Project of Jiangsu Commission of Health (BJ16007); (2) Youth Medical Key Talents with National Tutorial System Training Program of Suzhou (GGRC028).
Conflicts of interest
There are no conflicts of interest.
References
- Methylaminolaevulinic acid photodynamic therapy in the treatment of erythroplasia of Queyrat. Dermatology. 2011;223:52-6.
- [CrossRef] [PubMed] [Google Scholar]
- Methyl-aminolevulinate photodynamic therapy for the treatment of erythroplasia of Queyrat in 23 patients. J Dermatolog Treat. 2012;23:330-2.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy in the diagnosis and management of basal cell carcinoma. Future Oncol. 2015;11:2975-84.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopic findings of penile intraepithelial neoplasia: Bowenoid papulosis, Bowen disease and erythroplasia of Queyrat. Australas J Dermatol. 2019;60:e201-7.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of dermoscopy in distinguishing erythroplasia of Queyrat from common forms of chronic balanitis: Results from a multicentric observational study. J Eur Acad Dermatol Venereol. 2019;33:966-72.
- [CrossRef] [PubMed] [Google Scholar]





