Translate this page into:
Edema and ulcers on the legs and dilated abdominal veins caused by thromboembolism of inferior vena cava in a patient with protein C deficiency
Correspondence Address:
Takashi Hashimoto
Department of Dermatology, Kurume University School of Medicine, and Kurume University Institute of Cutaneous Cell Biology, 67 Asahimachi, Kurume, Fukuoka 830-0011
Japan
| How to cite this article: Kawano H, Ohata C, Ono F, Ishii N, Hamada T, Nakama T, Furumura M, Tsuruta D, Hashimoto T. Edema and ulcers on the legs and dilated abdominal veins caused by thromboembolism of inferior vena cava in a patient with protein C deficiency. Indian J Dermatol Venereol Leprol 2013;79:725 |
Sir,
The major clinical symptom of protein C deficiency is venous thromboembolism, which mostly occurs in deep veins of the lower extremities, but can also cause thrombosis in inferior vena cava. [1] We report a case of inferior vena cava thrombosis caused by Protein C deficiency, which subsequently caused leg ulcers without deep vein thrombosis (DVT) of the lower extremities.
A 33-year-old Japanese male cook noticed pain in the legs and the lower back and visited an orthopedist. Computed tomography (CT) revealed thrombosis of inferior vena cava, just below bifurcation area of renal vein, left iliac vein, left femoral vein, and left greater saphenous vein. Subsequently, the patient was referred to cardiovascular department in our hospital, and was diagnosed as having hereditary protein C deficiency, which was considered as a cause of thrombosis. Patient had a family history of cerebral infarction in his father. Anticoagulant therapy was started; however, the patient discontinued all treatments 6 months later. The patient had no treatment for approximately 5 years, and then noticed edema on the legs, followed by slowly developing ulcers on the right leg. The patient visited us again.
Physical examination revealed symmetrical scaly erythema on the both legs with extensive edema [Figure - 1]. Two skin ulcers 20 mm in size were found within the erythema on the inner surface of the right leg [Figure - 1]. In addition, extensively dilated epigastric veins were shown on the abdomen [Figure - 2]. Neither livedo nor varix was recognized on the both legs. Laboratory tests revealed decreased activated protein C (58%, normal range 64-146) and protein C antigen levels (45%, normal range 70-150). The results of other coagulation tests including D-dimer and activated Protein S were within normal limits. Antinuclear antibody, anti-cardiolipin antibody, lupus anticoagulant, myeloperoxidase-antineutrophil cytoplasmic antibody (ANCA), and proteinase 3 -ANCA were not detected. Chest, abdomen, and leg contrast enhanced CT revealed obstruction of inferior vena cava below the level of diaphragm and bilateral common iliac veins with several collateral veins, including mesenteric veins, subcutaneous veins of the abdomen and paravertebral veins [Figure - 3]. There was neither DVT in the legs nor pulmonary embolism. Skin biopsy from the edge of the ulcer revealed dilation and proliferation of the capillaries with thick walled vessels in the superficial dermis. There was no thrombus formation in the specimen. We diagnosed leg ulcers due to venous stasis in association with inferior vena cava thrombosis caused by congenital heterozygous protein C deficiency. Re-started anticoagulation therapy with warfarin sodium cleared the ulcers dramatically along with the improvement of extensive edema and scaly erythema on both legs in 3 weeks.
 |
| Figure 1: Clinical appearance. Two skin ulcers 2 cm in size with erythema on the right inner leg |
 |
| Figure 2: Multiple dilated subcutaneous veins in the abdomen |
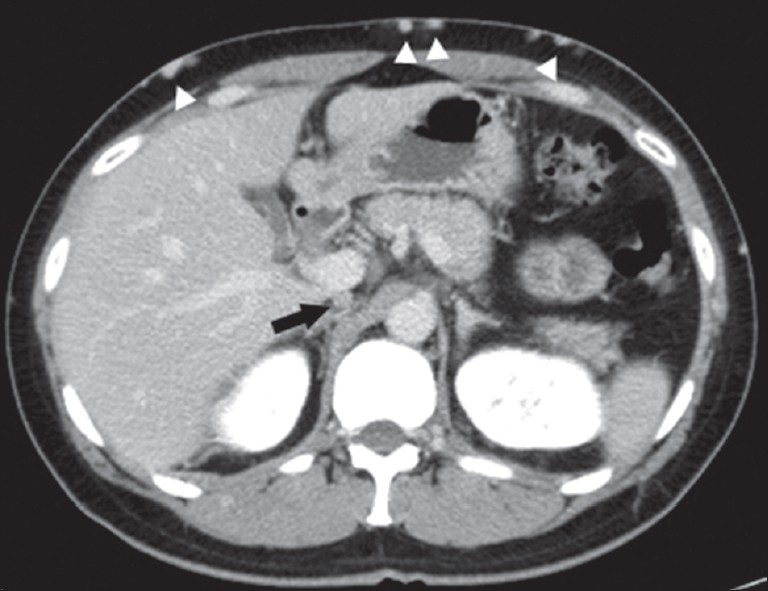 |
| Figure 3: Transverse contrast-enhanced computed tomography revealed obstruction of inferior vena cava (arrow) and dilated collateral veins in superficial abdominal wall (arrow head) |
In our case, protein C deficiency first caused obstruction of inferior vena cava, and subsequently, edema of the legs with leg ulcers and dilated abdominal veins developed. The most common physical signs of chronic inferior vena cava obstructions are bilateral edema of the legs and dilated superficial abdominal wall collateral veins. [2] However, a review of 24 patients with inferior vena cava obstruction revealed bilateral leg edema in only 10 (42%) patients, and dilated abdominal veins in 12 (50%) patients. [3] Out of 24, 3 patients developed bilateral leg ulcers without DVT on the leg. Among these 3 patients, only one patient was accompanied with bilateral leg edema and dilated abdominal veins. Thus, concurrence of edema and ulcers on the legs and dilated abdominal veins due to obstruction of inferior vena cava without DVT on the leg, which was exactly the same condition in our case, seems to occur rarely.
Our patient was a cook, and spent a long time in a standing position. Therefore, the patient′s life-style is probably responsible for the disease development; although, external injury could also be a trigger for the skin ulcers.
For the treatment of heterozygous protein C deficiency, oral anticoagulant with a coumarin-derivative or heparin remains standard therapy. [4] In our patient, both edema and ulcers on the legs were cured only 3 weeks after initiation of anticoagulant therapy. Furthermore, thrombosis found in left femoral vein and left greater saphenous vein in the first CT disappeared in the second CT, 6 months after anticoagulant therapy. These results signify that our patient responded well to anticoagulant therapy. However, the delay of initiation of the treatment might have led to Budd-Chiari syndrome, the most severe complication of protein C deficiency, because thrombosis extended to the level of the diagram in the second CT. [5]
Laboratory tests and physical examination excluded leg ulcers caused by venous valve dysfunction, artheriosclerosis, arterial embolism, arteritis, and phlebitis. Although some patients with protein C deficiency develop warfarin induced necrosis, our patient did not.
Acknowledgments
We gratefully appreciate the secretarial work of Ms. Hanako Nakagawa and Ms. Sachika Notomi. We thank the patient for his participation.
| 1. |
Kobayashi T, Ito A, Okada Y, Kojima N, Fujita A, Teruya M. Protein C deficiency as a cause of simultaneous acute thrombosis of the superior mesenteric vein and inferior vena cava with jejunal infarction. Surgery 2005;137:482-3.
[Google Scholar]
|
| 2. |
Missal ME, Robinson JA, Tatum RW. Inferior vena cava obstruction: Clinical manifestations, diagnostic methods, and related problems. Ann Intern Med 1965;62:133-61.
[Google Scholar]
|
| 3. |
Jackson BT, Thomas ML. Post-thrombotic inferior vena caval obstruction. A review of 24 patients. Br Med J 1970;1:18-22.
[Google Scholar]
|
| 4. |
Pescatore SL. Clinical management of protein C deficiency. Expert Opin Pharmacother 2001;2:431-9.
[Google Scholar]
|
| 5. |
Hiroe S, Itoh H, Matsumoto H, Takahasi S, Sato Y, Yamada S, et al. Case of Budd-Chiari syndrome 3 months after vaginal delivery. J Obstet Gynaecol Res 2008;34:605-8.
[Google Scholar]
|
Fulltext Views
4,678
PDF downloads
1,856





