Translate this page into:
Efficacy of topical photodynamic therapy for keratoacanthomas: A case-series of four patients
2 Faculty of Medicine, Department of Pathology, Pontificia Universidad Cat�lica de Chile, Santiago, Chile
Correspondence Address:
Maria M Farias
Albacete 4420, Dep 56, Las Condes Santiago
Chile
| How to cite this article: Farias MM, Hasson A, Navarrete C, Nicklas C, Garcia-Huidobro I, Gonzalez S. Efficacy of topical photodynamic therapy for keratoacanthomas: A case-series of four patients. Indian J Dermatol Venereol Leprol 2012;78:172-174 |
Abstract
Topical photodynamic therapy (PDT) is an excellent treatment option for various non-melanoma skin cancers and precancerous lesions, including actinic keratosis, Bowen's disease, and basal cell carcinoma. The clinical use of PDT includes a broad range of neoplastic, inflammatory, and infectious skin diseases. There is also anecdotal evidence suggesting the efficacy of PDT for the treatment of keratoacanthomas (KA). We report a case-series of four patients with solitary KA confirmed by histology, treated with topical PDT with methylaminolevulinic acid (MAL) cream. After three sessions of PDT, the lesions completely disappeared. There was no evidence of recurrence and excellent cosmetic outcome was achieved after three years of follow-up. Topical photodynamic therapy with MAL can be a therapeutic alternative for KA with good clinical and cosmetic outcomes.Introduction
The "photodynamic reaction" is the photochemical process involving the absorption of light by a photo-sensitizer and the subsequent generation of reactive oxygen species. Photodynamic therapy (PDT) has emerged as a new therapeutic modality in dermatology. Topical PDT has shown to be effective and well tolerated in the treatment of actinic keratosis, Bowen′s disease, and basal cell carcinoma, among others. [1]
PDT has also been effective against other types of non-melanoma skin cancers and the clinical indications for this treatment modality has expanded to numerous skin disorders. [2] However, only anecdotal evidence has been reported on the efficacy of PDT for the treatment of keratoacanthomas (KA). [3],[4]
Case Report
We report a case series of four patients with solitary KA (Range 71-95 years old, two males and two females).
Since the patients were not eligible for a surgical procedure (because of age and comorbidities), they opted for treatment with PDT after discussion and signing an informed consent form. Diagnosis was confirmed by skin biopsy in all cases [Figure - 1]. KA were localized on the face (two cases), hand (one case) and leg (one case), with a variable evolution time since appearance of 6-36 months.
 |
| Figure 1: Panoramic view of an example of keratoacanthoma showing crateriform shape and superficial squamous nests (H and E, × 40) |
To improve the absorption of the methylaminolevulinic acid (MAL) cream, lesions were curettaged two weeks prior to treatment removing scales and crusts. According to our protocol, a thick layer (about 1 mm) of 160 mg/g MAL cream (Metvix® , Photocure ASA, Oslo, Norway) was applied on the lesions and surrounding tissue (5 mm margin) and then were covered with an occlusive dressing (Tegaderm® ) keeping the cardboard backing. After 3 h, the dressings were removed and the lesions were treated with red light at a wavelength of 632 nm (Waldman™ lamp PDT 1200 L, incoherent light source), light dose of 37 J/cm 2 , light intensity 70 mW/cm 2 , during 8-9 min on each patient. The patients were neither treated with intralesional anesthesia nor systemic analgesic prophylaxis; they only reported mild localized pain and burning sensation during light exposure. The MAL-PDT protocol was repeated one week and one month after the first session in all patients.
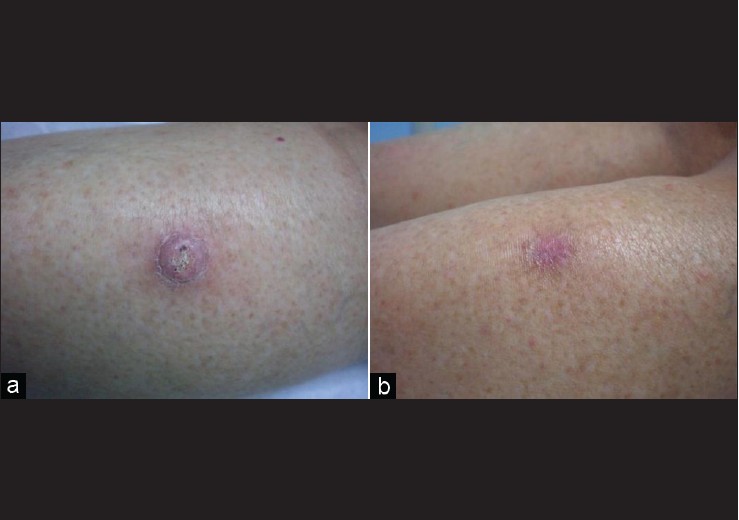
Patients were re-evaluated seven days after completing the last PDT session; they all had complete resolution of KA [Figure - 2], [Figure - 3], [Figure - 4] and [Figure - 5]. After 3 years of follow-up, all four cases were still on remission and were highly satisfied with the clinical and cosmetic outcome.
 |
| Figure 2: (a) Patient with solitary keratoacanthomas on the forehead. (b) Same patient after three sessions of topical photodynamic therapy with methylaminolevulinic acid cream |
 |
| Figure 3: (a) Patient with solitary keratoacanthomas on the left hand. (b) Same patient after three sessions of topical photodynamic therapy with methylaminolevulinic acid cream |
 |
| Figure 4: (a) Patient with solitary keratoacanthomas on the back of the right leg. (b) Same patient after three sessions of topical photodynamic therapy with methylaminolevulinic acid cream |
 |
| Figure 5: (a) Patient with solitary keratoacanthomas on the forehead. (b) Same patient after three sessions of topical photodynamic therapy with methylaminolevulinic acid cream |
Discussion
KA is a unique cutaneous tumor appearing in light-skinned, elderly patients on sun-exposed areas. KA is characterized by rapid growth, sometimes followed by a period of involution. Although KA may spontaneously regress in a variable period of time (usually 4-6 months), there is a significant evidence to consider KA as a well-differentiated squamous cell carcinoma (SCC), though this is an issue still in debate. [5] Furthermore, the scar resulting from spontaneous resolution can sometimes be worse than the scar following treatment.
Therefore, therapeutic intervention is recommended, not only because there are no reliable criteria to differentiate KA from SCC, [5] but also to prevent rapid growth, to achieve minimal scarring, and for cosmetic purposes. [6]
Several treatment options exist, including surgical excision as the treatment of choice; but cryotherapy with liquid nitrogen, [6] electrodessication and curettage, [7] radiotherapy, [8] and argon or YAG lasers have also been used in small and solitary KA with success. [9] Intralesional therapy with methotrexate and 5-fluorouracil, topical treatment with imiquimod, and systemic therapy with retinoids and methotrexate have also been proven effective; however, recurrences and scars often occur. When regular curettage or excision is performed, risk of recurrence is 4%-8%. [6]
Only two reports on the efficacy of PDT for treatment of KA are found in literature. The first case is a 49-year-old man with a 3.5 × 2.8-cm-sized KA treated with delta-aminolevulanic acid (ALA). [3] The second case is a 58-year-old woman with a large KA centrifugum marginatum on the arm, treated with PDT sessions with endogenous purified haematoprotoporphirin derivative (PHD); [4] in both cases, the results were optimal. The mechanism of action could be explained by the generation of cytotoxic radicals that damaged KA tissue cells, microcirculation arrest, induction of an immune response, and cellular inflammatory response in the surrounding tissue. [1]
One of the limitations of this case-series report is that we cannot compare the MAL-PDT outcome with the natural history of KA (potential involution) since this was not the objective of this work. However, studies have shown an increase in the diameter of KA, with only a small proportion of involution (10%) within 1 month follow up. This makes highly improbable that our four patient′s success rate was explained by natural involution. [10] We report a case-series of four patients treated with MAL-PDT with complete resolution of KA lesions without scarring, and with not recurrences after 3-years of follow up.
In conclusion, we consider MAL-PDT as a good therapeutic alternative for KA, due to its clinical effectiveness and outstanding cosmetic outcome without scarring.
| 1. |
Calzavara-Pinton PG, Venturini M, Sala R. Photodynamic therapy: Update 2006, Part 2: Clinical results. J Eur Acad Dermatol Venereol 2007;21:439-51.
[Google Scholar]
|
| 2. |
Calzavara-Pinton P, Arisi M, Sereni E, Ortel B. A critical reappraisal of off-label indications for topical photodynamic therapy with aminolevulinic acid and methylaminolevulinate. Rev Recent Clin Trials 2010;5:112-6.
[Google Scholar]
|
| 3. |
Souza CS, Felício LB, Arruda D, Ferreira J, Kurachi C, Bagnato VS. Systemic photodynamic therapy as an option for keratoacanthoma centrifugum marginatum treatment. J Eur Acad Dermatol Venereol 2009;23:101-2.
[Google Scholar]
|
| 4. |
Radakovic-Fijan S, Hönigsmann H, Tanew A. Efficacy of topical photodynamic therapy of a giant keratoacanthoma demonstrated by partial irradiation. Br J Dermatol 1999;141:936-8.
[Google Scholar]
|
| 5. |
Schwartz RA. Keratoacanthoma: A clinico-pathologic enigma. Dermatol Surg 2004;30:326-33.
[Google Scholar]
|
| 6. |
Karaa A, Khachemoune A. Keratoacanthoma: A tumor in search of a classification. Int J Dermatol 2007;46:671-8.
[Google Scholar]
|
| 7. |
Nedwich JA. Evaluation of curettage and electrodesiccation in treatment of keratoacanthoma. Australas J Dermatol 1991;32:137-41.
[Google Scholar]
|
| 8. |
Donahue B, Cooper JS, Rush S. Treatment of aggressive keratoacanthomas by radiotherapy. J Am Acad Dermatol 1990;23:489-93.
[Google Scholar]
|
| 9. |
Thiele JJ, Ziemer M, Fuchs S, Elsner P. Combined 5-fluorouracil and Er: YAG laser treatment in a case of recurrent giant keratoacanthoma of the lower leg. Dermatol Surg 2004;30:1556-60.
[Google Scholar]
|
| 10. |
Martorell-Calatayud A, Requena C, Nagore E, Sanmartín O, Serra-Guillén C, Botella-Estrada R, et al. Intralesional infusion of methotrexate as neoadjuvant therapy improves the cosmetic and functional results of surgery to treat keratoacanthoma: Results of a randomized trial. Actas Dermosifiliogr 2011;102:605-15.
[Google Scholar]
|
Fulltext Views
3,645
PDF downloads
2,110





