Translate this page into:
Epidermolysis bullosa acquisita associated with dysphagia and stricture of esophagus
2 Department of Dermatology, B Y L Nair Charitable Hospital and T N Medical College, Mumbai Central, Mumbai, Maharashtra, India
Correspondence Address:
Sunil Vyankatrao Pawar
Department of Gastroenterology, B Y L Nair Charitable Hospital and T N Medical College, Mumbai Central, Mumbai - 400 008, Maharashtra
India
| How to cite this article: Pawar SV, Mohite AR, Surude RG, Rathi PM, Nayak CS. Epidermolysis bullosa acquisita associated with dysphagia and stricture of esophagus. Indian J Dermatol Venereol Leprol 2016;82:717-719 |
Sir,
Epidermolysis bullosa acquisita (EBA) is a rare subepidermal autoimmune blistering skin disease. Dysphagia is a rare presentation. We present a case that required mechanical and pharmacological interventions.
A 46-year-old man presented to the gastroenterology outpatient department with progressive difficulty in swallowing solids for 3 years. He developed dysphagia to liquids too, since 3 months; it progressed to such an extent that he was unable to swallow anything for the last 5 days. There was weight loss of about 10 kg. The patient also had a history of blistering of skin at sites of minor trauma for the past 9 years. These lesions would rupture and heal with scarring. Examination revealed contracture of elbows and syndactyly with loss of nails. Ichthyosis was observed over the limbs [Figure - 1]a. He had bullous lesions on the face and oral mucosa which healed, leading to microstomia [Figure - 1]b. Deformed teeth with caries were present. Barium swallow showed complete obstruction at the level of mid-esophagus [Figure - 1]c. An esophago-gastro-duodenoscopy demonstrated a web [Figure - 2]a, bullous lesions [Figure - 2]b and a small slit-like opening [Figure - 2]c. The scope could not be negotiated beyond this point. Skin biopsy revealed a split at the subepidermal level with bulla formation [Figure - 2]d. Direct immunofluorescence studies showed linear deposits of IgG and C3 at the dermo-epidermal junction and the diagnosis of epidermolysis bullosa acquisita was confirmed with the salt-split skin technique. He was started on oral prednisolone, 40mg in tapering dose and azathioprine, following which the skin lesions improved, but dysphagia persisted. Serial dilatation of the esophagus was performed on a guide wire with Savary–Gilliard tubes up to 9 mm in view of the long stricture following which he was able to take semi-solid food. The patient gained 10 kg weight over the next 2 months.
 |
| Figure 1a: Icthyosis, syndactyly with loss of nails of both feet |
 |
| Figure 1b: contracture of elbows and syndactyly with loss of nails. Ichthyosis was observed over the limbs microstomia |
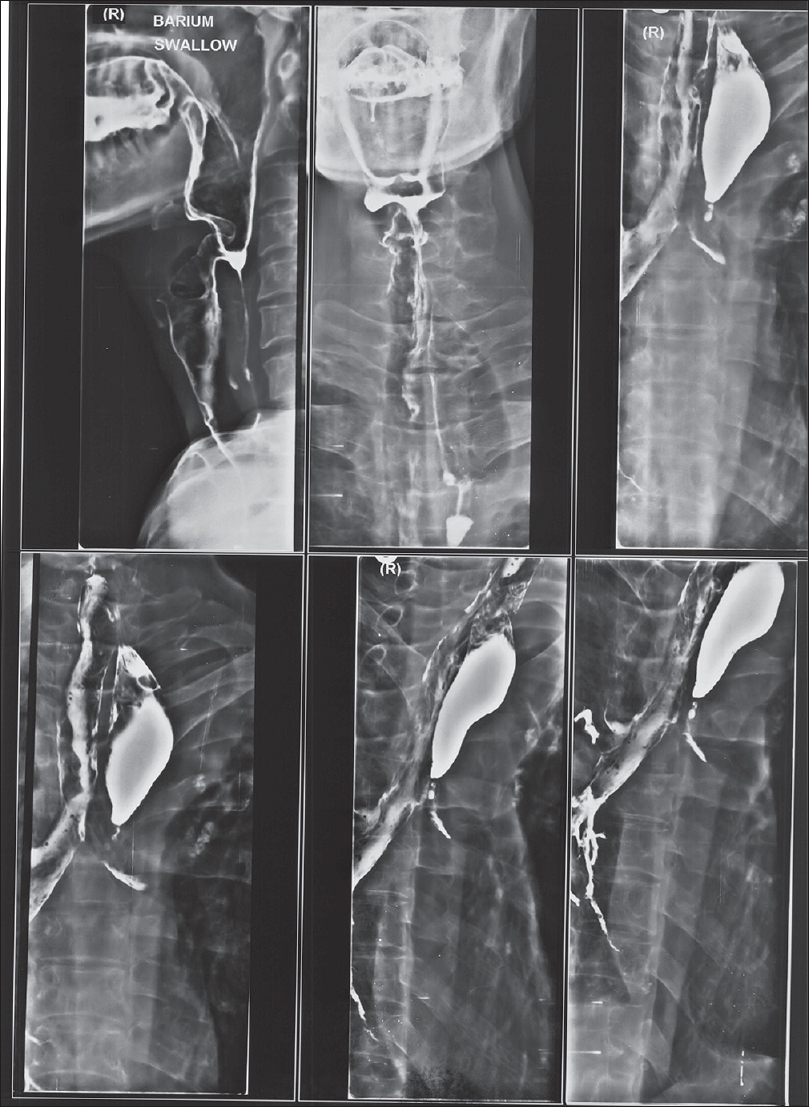 |
| Figure 1c: Barium swallow showed complete obstruction at the level of mid-esophagus |
 |
| Figure 2a: An esophago-gastro-duodenoscopy demonstrated, web |
 |
| Figure 2b: An esophago-gastro-duodenoscopy demonstrated, bullous lesions |
 |
| Figure 2c: An esophago-gastro-duodenoscopy demonstrated, small slit-like opening |
 |
| Figure 2d: An esophago-gastro-duodenoscopy demonstrated, a skin biopsy revealed a split at the sub-epidermal level with bulla formation |
Epidermolysis bullosa acquisita is a relatively rare disorder affecting 0.2 cases per 1 million people.[1] It affects all ages and has a slight female predominance with onset of disease usually in adulthood. Blisters heal with scarring leading to contractures, loss of nails or syndactyly. In the head and neck region, blisters, ankyloglossia, restriction of mouth opening, dental caries, loss of alveolar bone, nasal synechiae, blockage of naso-lacrimal duct and symblepharon may be seen. Supraglottic stenosis, esophageal blisters and strictures are also common.[2] Childhood disease is more inflammatory with mucosal involvement but has a good long-term prognosis.[3] The presentations include a classic form, characterized by non-inflammatory blisters, primarily involving the trauma-prone areas. Bullous pemphigoid-like epidermolysis bullosa acquisita is an inflammatory eruption that involves the trunk. Mucous membrane pemphigoid and Brunsting–Perry pemphigoid-like epidermolysis bullosa acquisita present primarily involving the mucosal surfaces.[4]
The disease is associated with inflammatory bowel disease, rheumatoid arthritis, diabetes mellitus, cryoglobulinemia, psoriasis, myeloma and systemic lupus erythematosus.[5] These patients are found to have autoantibodies against type VII collagen. On histopathology, sub epidermal bullae are seen with infiltrates of leukocytes. Direct immunofluorescence reveals linear IgG deposition along the dermo-epidermal junction. The use of the salt-split skin technique detects autoantibodies binding to the dermal side of the separation which distinguishes the condition from bullous pemphigoid, where these bind to the epidermal side.[6] Definite treatment guidelines are not available due to the low prevalence of the disease. We used 40 mg oral prednisolone in a tapering dose along with azathioprine. Different treatments have been tried in this condition, along with steroids, such as cyclosporine, minocycline, dapsone, mycophenolic acid and methotrexate. Plasmapheresis, intravenous immunoglobulins and rituximab have been tried in resistant cases. Progressive dysphagia may be alleviated by medications and in non-responders, by dilatation. Esophageal reflux should be treated to prevent laryngeal injury.
In conclusion, epidermolysis bullosa acquisita with esophageal involvement is best tackled by a multidisciplinary approach. Dysphagia can be due to erosions or strictures and can be treated with immunosuppression and if required, esophageal dilatation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hallel-Halevy D, Nadelman C, Chen M, Woodley DT. Epidermolysis bullosa acquisita: Update and review. Clin Dermatol 2001;19:712-8.
[Google Scholar]
|
| 2. |
Luke MC, Darling TN, Hsu R, Summers RM, Smith JA, Solomon BI, et al. Mucosal morbidity in patients with epidermolysis bullosa acquisita. Arch Dermatol 1999;135:954-9.
[Google Scholar]
|
| 3. |
Lacour JP, Bernard P, Rostain G, Baechler-Sadoul E, Pisani A, Ortonne JP. Childhood acquired epidermolysis bullosa. Pediatr Dermatol 1995;12:16-20.
[Google Scholar]
|
| 4. |
Remington J, Chen M, Burnett J, Woodley DT. Autoimmunity to type VII collagen: Epidermolysis bullosa acquisita. Curr Dir Autoimmun 2008;10:195-205.
[Google Scholar]
|
| 5. |
Klein JS, Goldin HM, Keegan C, Shiomoto G, Israel SR, Bronson DM. Clear-cell carcinoma of the lung in a patient treated with cyclosporine for epidermolysis bullosa acquisita. J Am Acad Dermatol 1991;24:297.
[Google Scholar]
|
| 6. |
Gammon WR, Briggaman RA, Inman AO 3rd, Queen LL, Wheeler CE. Differentiating anti-lamina lucida and anti-sublamina densa anti-BMZ antibodies by indirect immunofluorescence on 1.0 M sodium chloride-separated skin. J Invest Dermatol 1984;82:139-44.
[Google Scholar]
|
Fulltext Views
2,365
PDF downloads
1,290





