Translate this page into:
Hereditary leiomyomatosis with renal cell carcinoma
2 Department of Histopathology, Mediciti Hospitals, Hyderabad, Andhra Pradesh, India
Correspondence Address:
Anuradha S Raman
Department of Nephrology, Apollo Hospitals, Hyderabad, 5-9-22, Secretariat Road, Hyderabad, Andhra Pradesh - 500 063
India
| How to cite this article: Soni SS, Gowrishankar S, Adikey GK, Raman AS. Hereditary leiomyomatosis with renal cell carcinoma. Indian J Dermatol Venereol Leprol 2008;74:63-64 |
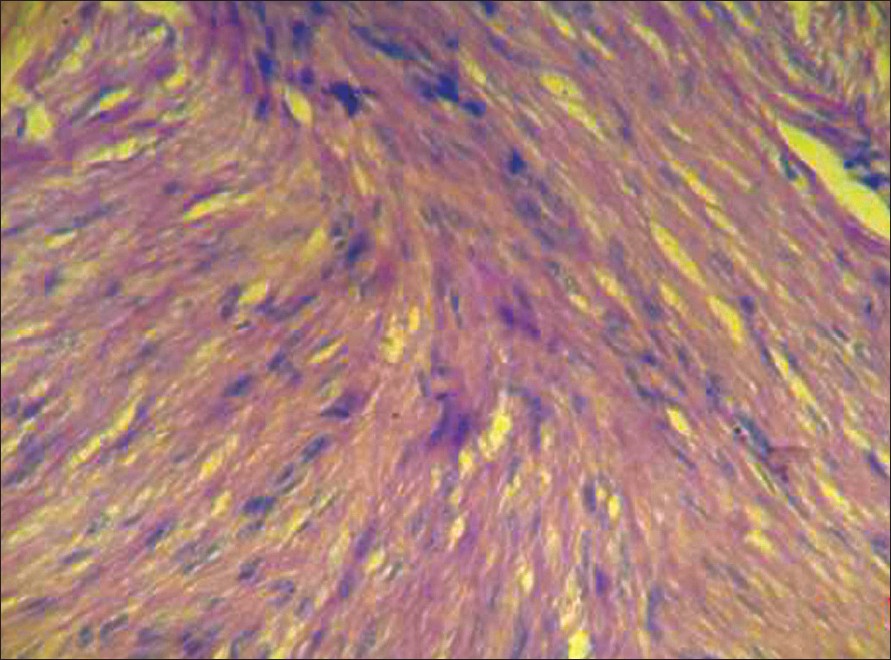 |
| Figure 2: Proliferation of smooth muscle cells in fascicles suggestive of leiomyoma (H and E stain, X400) |
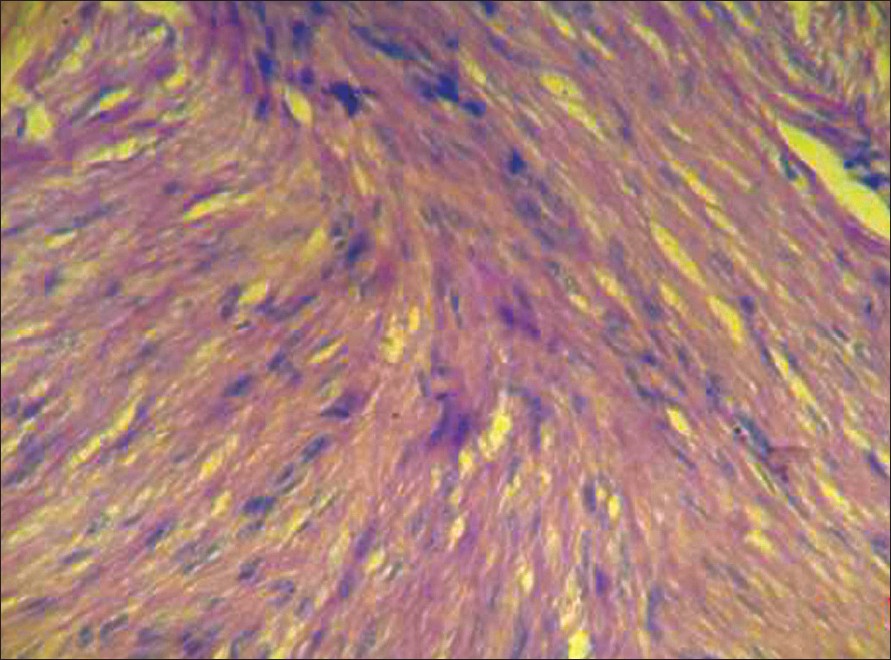 |
| Figure 2: Proliferation of smooth muscle cells in fascicles suggestive of leiomyoma (H and E stain, X400) |
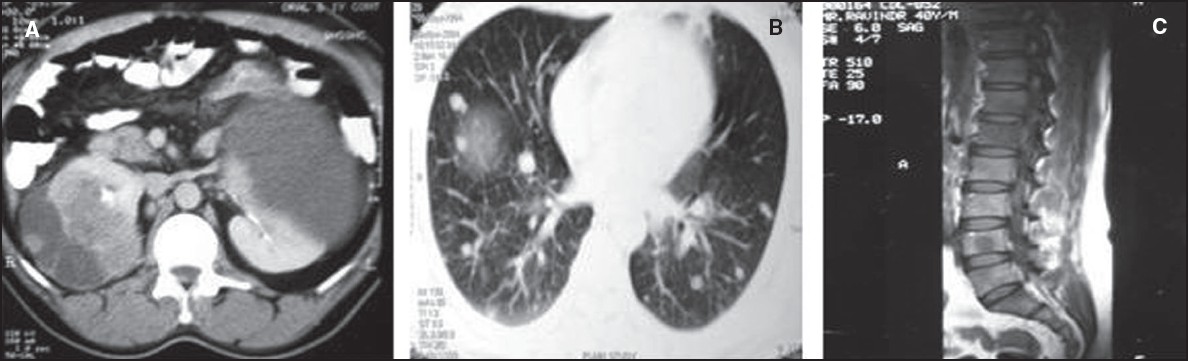 |
| Figure 1: A. Computed tomography (CT) scan of abdomen showing bilateral renal masses B. CT scan of chest showing multiple pulmonary metastases C. Magnetic resonance imaging (MRI) scan showing metastasis to L4 vertebra |
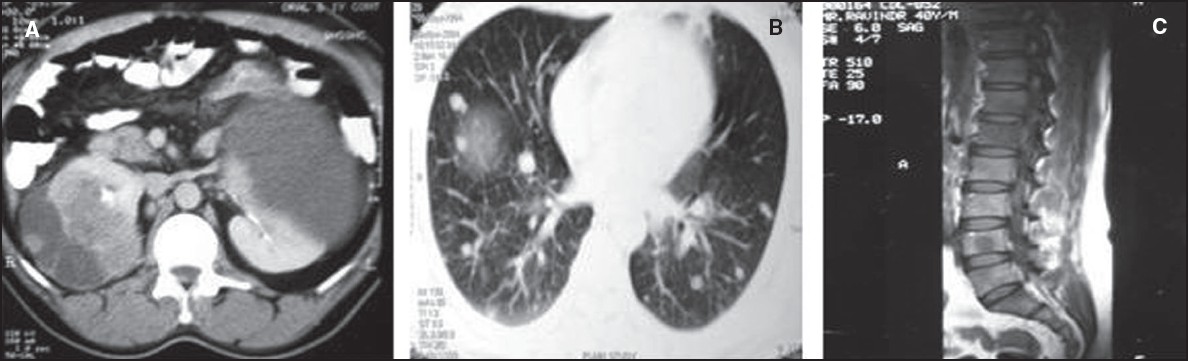 |
| Figure 1: A. Computed tomography (CT) scan of abdomen showing bilateral renal masses B. CT scan of chest showing multiple pulmonary metastases C. Magnetic resonance imaging (MRI) scan showing metastasis to L4 vertebra |
Sir,
Hereditary leiomyomatosis with renal cell carcinoma (HLRCC) is a rare syndrome of cutaneous leiomyoma, uterine leiomyomatosis and renal cell carcinoma. [1] It is an autosomal dominant disorder caused by mutations in the gene encoding the enzyme fumarate hydratase (FH). Launonen et al., [1] identified that the predisposition gene ′HLRCC′ is mapped to 1q42-q44. It is often an unrecognized tumor syndrome. Its awareness is important because of its association with aggressive uterine fibroids and renal cell cancer. We report a case with multiple cutaneous leiomyomas and papillary renal cell cancer.
A 40-year-old male, a known case of hypertension controlled with one drug from two years presented with complaints of fullness in abdomen, anorexia, weakness, weight loss and intermittent fever since one month. Clinical examination revealed stable vitals and bilateral ballotable kidneys. He also had firm brown-colored non-painful, small skin nodules, six in number on the right arm, three on the left arm and four in the right thigh region. He was the eldest of the six siblings (two sons, four daughters). His father died of renal carcinoma at the age of 50 and his grandmother had similar skin nodules. The eldest of his four younger sisters had multiple uterine fibroids.
His investigations revealed hematocrit of 30 Vol%, serum creatinine-1.2 mg/dl, and serum calcium-10.4 mg/dl. Computerized tomography of abdomen showed bilateral enlarged kidneys with a mass lesion of 8 x 6 cm in each kidney [Figure - 1]. Fine needle aspiration biopsy of a mass was suggestive of papillary renal carcinoma. Biopsies of skin nodules from the right arm and the right thigh showed cutaneous leiomyomatosis [Figure - 2]. Assessment for the spread of malignancy was positive with multiple metastases. Bilateral papillary renal malignancy at a young age, distant metastases at diagnosis, positive family history and cutaneous leiomyomatosis make it a case of hereditary leiomyomatosis with renal cell carcinoma.
Tomlinson et al., [2] studied individuals with germline mutations in the FH gene. The activity of this enzyme of the TCA (tricarboxylic acid) cycle was reduced in lymphoblastoid cells from cases with leiomyomatosis. Chan et al., [3] suggested that the ′HLRCC′ is likely to be a tumor suppressor gene. Kiuru et al., [4] concluded that this is a two-hit condition.
The majority (76%) of individuals with HLRCC present with a single or multiple cutaneous leiomyomas. Forty per cent of individuals with HLRCC have mild cutaneous manifestations with five or fewer lesions. [5] Histopathologically, proliferation of interlacing bundles of smooth muscle fibers with centrally located long blunt-ended nuclei is observed. Classical histological findings, family history of renal cell carcinoma and leiomyoma (both cutaneous and uterine) make the diagnosis of HLRCC likely in this case. Molecular diagnosis has not been made due to lack of facilities. This is the first case of the syndrome being reported from India. In view of the recent identification of this syndrome and lack of adequate clinical data, prognosis of these patients is not well defined although it appears to depend upon the staging of the tumor.
| 1. |
Launonen V, Vierimaa O, Kiuru M, Isola J, Roth S, Pukkala E, et al. Inherited susceptibility to uterine leiomyomas and renal cell cancer. Proc Natl Acad Sci 2001;98:3387-92.
[Google Scholar]
|
| 2. |
Alam NA, Olpin S, Rowan A, Kelsell D, Leigh IM, Tomlinson IP, Weaver T. Missense mutations in fumarate hydratase in multiple cutaneous and uterine leiomyomatosis and renal cell cancer. J Mol Diagn 2005;7:437-43.
[Google Scholar]
|
| 3. |
Chan I, Wong T, Martinez-Mir A, Christiano AM, McGrath JA. Familial multiple cutaneous and uterine leiomyomas associated with papillary renal cell cancer. Clin Exp Dermatol 2005;30:75-8.
[Google Scholar]
|
| 4. |
Kiuru M, Launonen V, Hietala M, Aittomaki K, Vierimaa O, Salovaara R, et al. Familial cutaneous leiomyomatosis is a two-hit condition associated with renal cell cancer of characteristic histopathology. Am J Pathol 2001;159:825-9.
[Google Scholar]
|
| 5. |
Wei MH, Toure O, Glenn GM, Pithukpakorn M, Neckers L, Stolle C, et al. Novel mutations in FH and expansion of the spectrum of phenotypes expressed in families with hereditary leiomyomatosis and renal cell cancer. J Med Genet 2006;43:18-27.
[Google Scholar]
|
Fulltext Views
2,410
PDF downloads
3,373





